Bladder Cancer
What is Bladder Cancer?
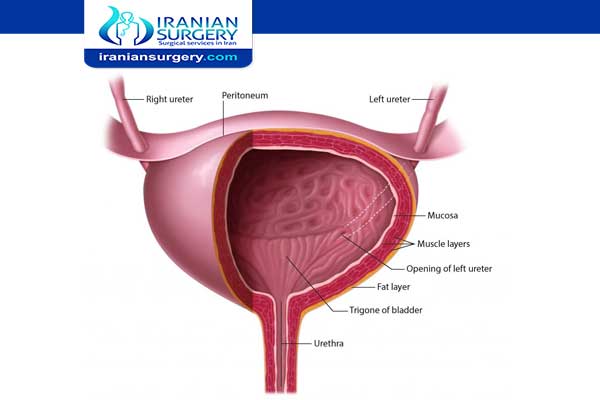
Bladder cancer is a common type of cancer that begins in the cells of the bladder. The bladder is a hollow muscular organ in your lower abdomen that stores urine. Bladder cancer most often begins in the cells (urothelial cells) that line the inside of your bladder. Most bladder cancers are diagnosed at an early stage, when the cancer is highly treatable.
Read more about : Urinary Incontinence
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Surgeons to treat your Bladder cancer in Iran. The price of treating a Bladder cancer in Iran can vary according to each individual’s case and will be determined by the type of Bladder cancer treatment you undergo and an in-person assessment with the doctor. So if you are looking for the cost of Bladder cancer treatment in Iran, you can contact us and get free consultation from Iranian surgery.
Read more about : There are different types of bladder cancer
Read more about : Orchiectomy surgery for prostate cancer
Read more about : Prostate Cancer Treatments Pros and Cons
Before Bladder Cancer Treatment
Symptoms of Bladder Cancer
Many people with bladder cancer can have blood in their urine but no pain while urinating. There are a number of symptoms that might indicate bladder cancer like fatigue, weight loss, and bone tenderness, and these can indicate more advanced disease. You should pay particular attention to the following symptoms:
. Blood in the urine
. Painful urination
. Frequent urination
. Urgent urination
. Urinary incontinence
. Pain in the abdominal area
. Pain in the lower back
When to see a doctor
If you notice that you have discolored urine and are concerned it may contain blood, make an appointment with your doctor to get it checked. Also make an appointment with your doctor if you have other signs or symptoms that worry you.
Causes
Bladder cancer begins when cells in the bladder develop changes (mutations) in their DNA. A cell’s DNA contains instructions that tell the cell what to do. The changes tell the cell to multiply rapidly and to go on living when healthy cells would die. The abnormal cells form a tumor that can invade and destroy normal body tissue. In time, the abnormal cells can break away and spread (metastasize) through the body.
Risk factors
Factors that may increase bladder cancer risk include:
. Smoking. Smoking cigarettes, cigars or pipes may increase the risk of bladder cancer by causing harmful chemicals to accumulate in the urine. When you smoke, your body processes the chemicals in the smoke and excretes some of them in your urine. These harmful chemicals may damage the lining of your bladder, which can increase your risk of cancer.
. Increasing age. Bladder cancer risk increases as you age. Though it can occur at any age, most people diagnosed with bladder cancer are older than 55.
. Being male. Men are more likely to develop bladder cancer than women are.
. Exposure to certain chemicals. Your kidneys play a key role in filtering harmful chemicals from your bloodstream and moving them into your bladder. Because of this, it’s thought that being around certain chemicals may increase the risk of bladder cancer. Chemicals linked to bladder cancer risk include arsenic and chemicals used in the manufacture of dyes, rubber, leather, textiles and paint products.
. Previous cancer treatment. Treatment with the anti-cancer drug cyclophosphamide increases the risk of bladder cancer. People who received radiation treatments aimed at the pelvis for a previous cancer have a higher risk of developing bladder cancer.
. Chronic bladder inflammation. Chronic or repeated urinary infections or inflammations (cystitis), such as might happen with long-term use of a urinary catheter, may increase the risk of a squamous cell bladder cancer. In some areas of the world, squamous cell carcinoma is linked to chronic bladder inflammation caused by the parasitic infection known as schistosomiasis.
. Personal or family history of cancer. If you’ve had bladder cancer, you’re more likely to get it again. If one of your blood relatives — a parent, sibling or child — has a history of bladder cancer, you may have an increased risk of the disease, although it’s rare for bladder cancer to run in families. A family history of Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), can increase the risk of cancer in the urinary system, as well as in the colon, uterus, ovaries and other organs.
Read more about: Interstitial cystitis (bladder pain syndrome)
Read more about: Bladder Cancer Risk Factors
Diagnosis
Diagnosing bladder cancer
Tests and procedures used to diagnose bladder cancer may include:
. Using a scope to examine the inside of your bladder (cystoscopy). To perform cystoscopy, your doctor inserts a small, narrow tube (cystoscope) through your urethra. The cystoscope has a lens that allows your doctor to see the inside of your urethra and bladder, to examine these structures for signs of disease. Cystoscopy can be done in a doctor’s office or in the hospital.
. Removing a sample of tissue for testing (biopsy). During cystoscopy, your doctor may pass a special tool through the scope and into your bladder to collect a cell sample (biopsy) for testing. This procedure is sometimes called transurethral resection of bladder tumor (TURBT). TURBT can also be used to treat bladder cancer.
. Examining a urine sample (urine cytology). A sample of your urine is analyzed under a microscope to check for cancer cells in a procedure called urine cytology.
. Imaging tests. Imaging tests, such as computerized tomography (CT) urogram or retrograde pyelogram, allow your doctor to examine the structures of your urinary tract.
During a CT urogram, a contrast dye injected into a vein in your hand eventually flows into your kidneys, ureters and bladder. X-ray images taken during the test provide a detailed view of your urinary tract and help your doctor identify any areas that might be cancer.
Retrograde pyelogram is an X-ray exam used to get a detailed look at the upper urinary tract. During this test, your doctor threads a thin tube (catheter) through your urethra and into your bladder to inject contrast dye into your ureters. The dye then flows into your kidneys while X-ray images are captured.
Determining the extent of the cancer
After confirming that you have bladder cancer, your doctor may recommend additional tests to determine whether your cancer has spread to your lymph nodes or to other areas of your body.
. Tests may include:
. CT scan
. Magnetic resonance imaging (MRI)
. Positron emission tomography (PET)
. Bone scan
. Chest X-ray
Your doctor uses information from these procedures to assign your cancer a stage. The stages of bladder cancer are indicated by Roman numerals ranging from 0 to IV. The lowest stages indicate a cancer that’s confined to the inner layers of the bladder and that hasn’t grown to affect the muscular bladder wall. The highest stage — stage IV — indicates cancer that has spread to lymph nodes or organs in distant areas of the body
Bladder cancer grade
Bladder cancers are further classified based on how the cancer cells appear when viewed through a microscope. This is known as the grade, and your doctor may describe bladder cancer as either low grade or high grade:
. Low-grade bladder cancer. This type of cancer has cells that are closer in appearance and organization to normal cells (well differentiated). A low-grade tumor usually grows more slowly and is less likely to invade the muscular wall of the bladder than is a high-grade tumor.
. High-grade bladder cancer. This type of cancer has cells that are abnormal-looking and that lack any resemblance to normal-appearing tissues (poorly differentiated). A high-grade tumor tends to grow more aggressively than a low-grade tumor and may be more likely to spread to the muscular wall of the bladder and other tissues and organs.
Prevention
Although there’s no guaranteed way to prevent bladder cancer, you can take steps to help reduce your risk. For instance:
. Don’t smoke. If you don’t smoke, don’t start. If you smoke, talk to your doctor about a plan to help you stop. Support groups, medications and other methods may help you quit.
. Take caution around chemicals. If you work with chemicals, follow all safety instructions to avoid exposure.
. Choose a variety of fruits and vegetables. Choose a diet rich in a variety of colorful fruits and vegetables. The antioxidants in fruits and vegetables may help reduce your risk of cancer.
. Drink plenty of liquids. There’s evidence that drinking a lot of fluids – mainly water – might lower a person’s risk of bladder cancer.
During Bladder Cancer Treatment
Types of bladder cancer
Different types of cells in your bladder can become cancerous. The type of bladder cell where cancer begins determines the type of bladder cancer. Doctors use this information to determine which treatments may work best for you.
Read more about: Common side effects of thyroid cancer treatment
Read more about: What happens during radical prostatectomy?
Types of bladder cancer include:
. Urothelial carcinoma. Urothelial carcinoma, previously called transitional cell carcinoma, occurs in the cells that line the inside of the bladder. Urothelial cells expand when your bladder is full and contract when your bladder is empty. These same cells line the inside of the ureters and the urethra, and cancers can form in those places as well. Urothelial carcinoma is the most common type of bladder cancer in the United States.
. Squamous cell carcinoma. Squamous cell carcinoma is associated with chronic irritation of the bladder — for instance, from an infection or from long-term use of a urinary catheter. Squamous cell bladder cancer is rare in the United States. It’s more common in parts of the world where a certain parasitic infection (schistosomiasis) is a common cause of bladder infections.
. Adenocarcinoma. Adenocarcinoma begins in cells that make up mucus-secreting glands in the bladder. Adenocarcinoma of the bladder is very rare.
Treatment by Stage
Your doctor can rate bladder cancer with a staging system that goes from stages 0 to 4 to identify how far the cancer has spread. The stages of bladder cancer mean the following:
. Stage 0 bladder cancer hasn’t spread past the lining of the bladder.
. Stage 1 bladder cancer has spread past the lining of the bladder, but it hasn’t reached the layer of muscle in the bladder.
. Stage 2 bladder cancer has spread to the layer of muscle in the bladder.
. Stage 3 bladder cancer has spread into the tissues that surround the bladder.
. Stage 4 bladder cancer has spread past the bladder to the neighboring areas of the body.
Your doctor will work with you to decide what treatment to provide based on the type and stage of your bladder cancer, your symptoms, and your overall health.
. Treatment for stage 0 and stage 1
Treatment for stage 0 and stage 1 bladder cancer may include surgery to remove the tumor from the bladder, chemotherapy, or immunotherapy, which involves taking a medication that causes your immune system to attack the cancer cells.
. Treatment for stage 2 and stage 3
Treatment for stage 2 and stage 3 bladder cancer may include:
. Removal of part of the bladder in addition to chemotherapy
. Removal of the whole bladder, which is a radical cystectomy, followed by surgery to create a new way for urine to exit the body.
. Chemotherapy, radiation therapy, or immunotherapy that can be done to shrink the tumor before surgery, to treat the cancer when surgery isn’t an option, to kill remaining cancer cells after surgery, or to prevent the cancer from recurring.
. Treatment for stage 4 bladder cancer
Treatment for stage 4 bladder cancer may include:
. Chemotherapy without surgery to relieve symptoms and extend life
. Radical cystectomy and removal of the surrounding lymph nodes, followed by a surgery to create a new way for urine to exit the body.
. Chemotherapy, radiation therapy, and immunotherapy after surgery to kill remaining cancer cells or to relieve symptoms and extend life.
. Clinical trial drugs
Treatment
Treatment options for bladder cancer
Treatment options for bladder cancer depend on a number of factors, including the type of cancer, grade of the cancer and stage of the cancer, which are taken into consideration along with your overall health and your treatment preferences.
Bladder cancer treatment may include:
. Surgery, to remove the cancer cells
. Chemotherapy in the bladder (intravesical chemotherapy), to treat cancers that are confined to the lining of the bladder but have a high risk of recurrence or progression to a higher stage.
. Chemotherapy for the whole body (systemic chemotherapy), to increase the chance for a cure in a person having surgery to remove the bladder, or as a primary treatment when surgery isn’t an option.
. Radiation therapy, to destroy cancer cells, often as a primary treatment when surgery isn’t an option or isn’t desired.
. Immunotherapy, to trigger the body’s immune system to fight cancer cells, either in the bladder or throughout the body.
. Targeted therapy, to treat advanced cancer when other treatments haven’t helped.
A combination of treatment approaches may be recommended by your doctor and members of your care team.
Bladder cancer surgery
Approaches to bladder cancer surgery might include:
. Transurethral resection of bladder tumor (TURBT). TURBT is a procedure to diagnose bladder cancer and to remove cancers confined to the inner layers of the bladder — those that aren’t yet muscle-invasive cancers. During the procedure, a surgeon passes an electric wire loop through a cystoscope and into the bladder. The electric current in the wire is used to cut away or burn away the cancer. Alternatively, a high-energy laser may be used.
Because doctors perform the procedure through the urethra, you won’t have any cuts (incisions) in your abdomen.
As part of the TURBT procedure, your doctor may recommend a one-time injection of cancer-killing medication (chemotherapy) into your bladder to destroy any remaining cancer cells and to prevent cancer from coming back. The medication remains in your bladder for a period of time and then is drained.
. Cystectomy. Cystectomy is surgery to remove all or part of the bladder. During a partial cystectomy, your surgeon removes only the portion of the bladder that contains a single cancerous tumor.
A radical cystectomy is an operation to remove the entire bladder and the surrounding lymph nodes. In men, radical cystectomy typically includes removal of the prostate and seminal vesicles. In women, radical cystectomy may involve removal of the uterus, ovaries and part of the vagina.
Radical cystectomy can be performed through an incision on the lower portion of the belly or with multiple small incisions using robotic surgery. During robotic surgery, the surgeon sits at a nearby console and uses hand controls to precisely move robotic surgical instruments.
. Neobladder reconstruction. After a radical cystectomy, your surgeon must create a new way for urine to leave your body (urinary diversion). One option for urinary diversion is neobladder reconstruction. Your surgeon creates a sphere-shaped reservoir out of a piece of your intestine. This reservoir, often called a neobladder, sits inside your body and is attached to your urethra. The neobladder allows most people to urinate normally. A small number of people difficulty emptying the neobladder and may need to use a catheter periodically to drain all the urine from the neobladder.
. Ileal conduit. For this type of urinary diversion, your surgeon creates a tube (ileal conduit) using a piece of your intestine. The tube runs from your ureters, which drain your kidneys, to the outside of your body, where urine empties into a pouch (urostomy bag) you wear on your abdomen.
. Continent urinary reservoir. During this type of urinary diversion procedure, your surgeon uses a section of intestine to create a small pouch (reservoir) to hold urine, located inside your body. You drain urine from the reservoir through an opening in your abdomen using a catheter a few times each day.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. Chemotherapy treatment for bladder cancer usually involves two or more chemotherapy drugs used in combination.
Chemotherapy drugs can be given:
. Through a vein (intravenously). Intravenous chemotherapy is frequently used before bladder removal surgery to increase the chances of curing the cancer. Chemotherapy may also be used to kill cancer cells that might remain after surgery. In certain situations, chemotherapy may be combined with radiation therapy.
. Directly into the bladder (intravesical therapy). During intravesical chemotherapy, a tube is passed through your urethra directly to your bladder. The chemotherapy is placed in the bladder for a set period of time before being drained. It can be used as the primary treatment for superficial bladder cancer, where the cancer cells affect only the lining of the bladder and not the deeper muscle tissue.
Radiation therapy
Radiation therapy uses beams of powerful energy, such as X-rays and protons, to destroy the cancer cells. Radiation therapy for bladder cancer usually is delivered from a machine that moves around your body, directing the energy beams to precise points.
Radiation therapy is sometimes combined with chemotherapy to treat bladder cancer in certain situations, such as when surgery isn’t an option or isn’t desired.
Immunotherapy
Immunotherapy is a drug treatment that helps your immune system to fight cancer.
Immunotherapy can be given:
. Directly into the bladder (intravesical therapy). Intravesical immunotherapy might be recommended after TURBT for small bladder cancers that haven’t grown into the deeper muscle layers of the bladder. This treatment uses bacillus Calmette-Guerin (BCG), which was developed as a vaccine used to protect against tuberculosis. BCG causes an immune system reaction that directs germ-fighting cells to the bladder.
. Through a vein (intravenously). Immunotherapy can be given intravenously for bladder cancer that’s advanced or that comes back after initial treatment. Several immunotherapy drugs are available. These drugs help your immune system identify and fight the cancer cells.
Targeted therapy
Targeted therapy drugs focus on specific weaknesses present within cancer cells. By targeting these weaknesses, targeted drug treatments can cause cancer cells to die. Your cancer cells may be tested to see if targeted therapy is likely to be effective.
Targeted therapy may be an option for treating advanced bladder cancer when other treatments haven’t helped.
Bladder preservation
In certain situations, people with muscle-invasive bladder cancer who don’t want to undergo surgery to remove the bladder may consider trying a combination of treatments instead. Known as trimodality therapy, this approach combines TURBT, chemotherapy and radiation therapy.
First, your surgeon performs a TURBT procedure to remove as much of the cancer as possible from your bladder while preserving bladder function. After TURBT, you undergo a regimen of chemotherapy along with radiation therapy.
If, after trying trimodality therapy, not all of the cancer is gone or you have a recurrence of muscle-invasive cancer, your doctor may recommend a radical cystectomy.
Read more about: Prostate biopsy recovery
Read more about: prostate biopsy anesthesia
Read more about: Cervical cancer symptoms
After Bladder Cancer Treatment
After bladder cancer treatment
Bladder cancer may recur, even after successful treatment. Because of this, people with bladder cancer need follow-up testing for years after successful treatment. What tests you’ll have and how often depends on your type of bladder cancer and how it was treated, among other factors.
In general, doctors recommend a test to examine the inside of your urethra and bladder (cystoscopy) every three to six months for the first few years after bladder cancer treatment. After a few years of surveillance without detecting cancer recurrence, you may need a cystoscopy exam only once a year. Your doctor may recommend other tests at regular intervals as well.
People with aggressive cancers may undergo more-frequent testing. Those with less aggressive cancers may undergo testing less often.
Outlook
What is the outlook for people with bladder cancer?
Your outlook depends on a lot of variables, including the type and stage of cancer. According to the American Cancer Society, the five-year survival rates by stage are the following:
. The five-year survival rate for people with stage 0 bladder cancer is around 98 percent.
. The five-year survival rate for people with stage 1 bladder cancer is around 88 percent.
. The five-year survival rate for people with stage 2 bladder cancer is around 63 percent.
. The five-year survival rate for people with stage 3 bladder cancer is around 46 percent.
. The five-year survival rate for people with stage 4 bladder cancer is around 15 percent.
There are treatments available for all stages. Also, survival rates don’t always tell the whole story and can’t predict your future. Speak with your doctor about any questions or concerns you may have regarding your diagnosis and treatment.