What is Thyroid Cancer?
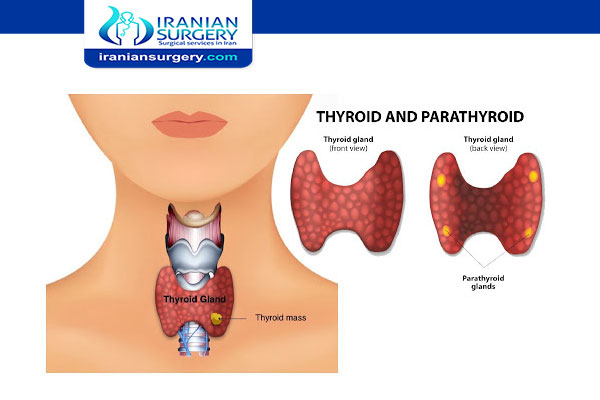
Thyroid cancer occurs in the cells of the thyroid — a butterfly-shaped gland located at the base of your neck, just below your Adam’s apple. Your thyroid produces hormones that regulate your heart rate, blood pressure, body temperature and weight.
Thyroid cancer might not cause any symptoms at first. But as it grows, it can cause pain and swelling in your neck.
Several types of thyroid cancer exist. Some grow very slowly and others can be very aggressive. Most cases of thyroid cancer can be cured with treatment.
Thyroid cancer rates seem to be increasing. Some doctors think this is because new technology is allowing them to find small thyroid cancers that may not have been found in the past.
What is the Thyroid Gland?
Your thyroid gland is one of many glands that make up your endocrine system. Endocrine glands release hormones that control different bodily functions.
The pituitary gland in your brain controls your thyroid gland and other endocrine glands. It releases thyroid-stimulating hormone (TSH). As the name suggests, TSH stimulates your thyroid gland to produce thyroid hormone.
Your thyroid needs iodine, a mineral, to make these hormones. Iodine-rich foods include cod, tuna, dairy products, whole-grain bread and iodized salt.
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best surgeons in Iran. The price of Thyroid Cancer Treatment in Iran can vary according to each individual’s case and will be determined based on an in-person assessment with the doctor.
For more information about the cost of Thyroid Cancer Treatment in Iran and to schedule an appointment in advance, you can contact Iranian Surgery consultants via WhatsApp number 0098 901 929 0946. This service is completely free.
Before Thyroid Cancer Treatment
Symptoms
Thyroid cancer typically doesn’t cause any signs or symptoms early in the disease. As thyroid cancer grows, it may cause:
. A lump (nodule) that can be felt through the skin on your neck
. Changes to your voice, including increasing hoarseness
. Difficulty swallowing
. Pain in your neck and throat
. Swollen lymph nodes in your neck
Read more about : Liver cancer treatment
When to see a doctor
If you experience any signs or symptoms that worry you, make an appointment with your doctor.
Causes
It’s not clear what causes thyroid cancer.
Thyroid cancer occurs when cells in your thyroid undergo genetic changes (mutations). The mutations allow the cells to grow and multiply rapidly. The cells also lose the ability to die, as normal cells would. The accumulating abnormal thyroid cells form a tumor. The abnormal cells can invade nearby tissue and can spread (metastasize) to other parts of the body.
Who might have thyroid cancer?
Risk factors
Women are three times more likely than men to get thyroid cancer. The disease is commonly diagnosed in women in their 40s and 50s, and men in their 60s and 70s. Even children can develop the disease.
Risk factors include:
. Enlarged thyroid (goiter).
. Family history of thyroid disease or thyroid cancer.
. Thyroiditis (inflammation of the thyroid gland).
. Gene mutations (changes) that cause endocrine diseases, such as multiple endocrine neoplasia type 2A (MEN2A) or type 2B (MEN2B) syndrome.
. Low iodine intake.
. Obesity (high body mass index).
. Exposure to radioactive fallout from nuclear weapons or a power plant accident.
. Female sex. Thyroid cancer occurs more often in women than in men.
. Exposure to high levels of radiation. Radiation therapy treatments to the head and neck increase the risk of thyroid cancer.
. Certain inherited genetic syndromes. Genetic syndromes that increase the risk of thyroid cancer include familial medullary thyroid cancer, multiple endocrine neoplasia, Cowden’s syndrome and familial adenomatous polyposis.
Complications
Thyroid cancer that comes back
Despite treatment, thyroid cancer can return, even if you’ve had your thyroid removed. This could happen if microscopic cancer cells spread beyond the thyroid before it’s removed.
Thyroid cancer may recur in:
. Lymph nodes in the neck
. Small pieces of thyroid tissue left behind during surgery
. Other areas of the body, such as the lungs and bones
Thyroid cancer that recurs can be treated. Your doctor may recommend periodic blood tests or thyroid scans to check for signs of a thyroid cancer recurrence.
Prevention
Doctors aren’t sure what causes most cases of thyroid cancer, so there’s no way to prevent thyroid cancer in people who have an average risk of the disease.
. Prevention for people with a high risk
Adults and children with an inherited gene mutation that increases the risk of medullary thyroid cancer may consider thyroid surgery to prevent cancer (prophylactic thyroidectomy). Discuss your options with a genetic counselor who can explain your risk of thyroid cancer and your treatment options.
. Prevention for people near nuclear power plants
A medication that blocks the effects of radiation on the thyroid is sometimes provided to people living near nuclear power plants. The medication (potassium iodide) could be used in the unlikely event of a nuclear reactor accident. If you live within 10 miles of a nuclear power plant and are concerned about safety precautions, contact your state or local emergency management department for more information.
 Diagnosis
Diagnosis
Tests and procedures used to diagnose thyroid cancer include:
. Physical exam. Your doctor will examine your neck to feel for physical changes in your thyroid, such as thyroid nodules. He or she may also ask about your risk factors, such as past exposure to radiation and a family history of thyroid tumors.
. Blood tests. Blood tests help determine if the thyroid gland is functioning normally.
. Ultrasound imaging. Ultrasound uses high-frequency sound waves to create pictures of body structures. To create an image of the thyroid, the ultrasound transducer is placed on your lower neck. The appearance of your thyroid on the ultrasound helps your doctor determine whether a thyroid nodule is likely to be noncancerous (benign) or whether there’s a risk that it might be cancerous.
. Removing a sample of thyroid tissue. During a fine-needle aspiration biopsy, your doctor inserts a long, thin needle through your skin and into the thyroid nodule. Ultrasound imaging is typically used to precisely guide the needle into the nodule. Your doctor uses the needle to remove samples of suspicious thyroid tissue. The sample is analyzed in the laboratory to look for cancer cells.
. Other imaging tests. You may have one or more imaging tests to help your doctor determine whether your cancer has spread beyond the thyroid. Imaging tests may include CT, MRI and nuclear imaging tests that use a radioactive form of iodine.
. Genetic testing. Some people with medullary thyroid cancer may have genetic changes that can be associated with other endocrine cancers. Your family history may prompt your doctor to recommend genetic testing to look for genes that increase your risk of cancer.
Risks and Side effects of Thyroid Surgery
Some possible side effects are common to nearly all operations. These include:
. Numbness over the area
. Infection, for example, a wound infection or chest infection
. A blood clot or risk of bleeding
. Swelling in the area
Your healthcare team monitor you closely to check for these. You have treatment, such as antibiotics, if you need it.
You may have other side effects following your thyroid surgery for example:
. Voice changes
After thyroid surgery some people have voice changes. Your voice may be hoarse or sound different. The thyroid gland lies close to your voice box (larynx). So surgery can damage the nerve to your voice box. This usually gets better within a few weeks.
It’s rare to have permanent changes. Your team might refer you to a voice therapist or speech therapist if you continue to have problems.
. A change in thyroid hormones
If you have had your whole thyroid removed, you will need to take tablets to replace the hormones that your thyroid would normally make. This is called thyroid hormone replacement.
The thyroid hormones are thyroxine (T4) and liothyronine (T3). You need one of these hormones to keep your body metabolism working effectively. You will need to take them for the rest of your life. Without the hormones, you would feel tired, gain weight, have dry skin and hair, and feel physically and mentally lacking in energy. Your doctor or specialist nurse will talk to you about which hormones you need to take and the correct dose.
You don’t generally need to take thyroid hormones if you have had part of your gland removed. Your remaining thyroid usually makes all the hormone you need. But you have blood tests to check that it is working well.
If you have had follicular or papillary thyroid cancer, the hormones may also help to stop the cancer from coming back. They stop your body from producing another hormone called thyroid stimulating hormone (TSH). TSH encourages these types of thyroid cancer cells to grow.
. A change in calcium levels
An operation on your thyroid gland could damage the nearby parathyroid glands. Or your surgeon might need to remove some of the parathyroid glands. The parathyroid glands control the levels of calcium in your blood.
Any damage could mean that these glands don’t work so well and calcium levels fall. If this happens, you will need to take calcium tablets and possibly extra vitamin D. This is usually a temporary side effect, but could be permanent in some people.
. Lymphoedema
After your surgery it is normal to have some swelling close to the wound. This usually goes away after a few weeks as the wound heals.
If you had some lymph nodes in your neck removed, the swelling may continue to be there and sometimes it gets worse. This is called lymphoedema.
Tell your doctor if you continue to have swelling in your neck after a few weeks. You may need some more exercises to help the swelling go down.
During Thyroid Cancer Treatment
Types of thyroid cancer
Thyroid cancer is classified into types based on the kinds of cells found in the tumor. Your type is determined when a sample of tissue from your cancer is examined under a microscope. The type of thyroid cancer is considered in determining your treatment and prognosis.
Types of thyroid cancer include:
. Papillary thyroid cancer. Up to 80% of all thyroid cancers are papillary. The most common form of thyroid cancer, papillary thyroid cancer arises from follicular cells, which produce and store thyroid hormones. Papillary thyroid cancer can occur at any age, but most often it affects people ages 30 to 50. Doctors sometimes refer to papillary thyroid cancer and follicular thyroid cancer together as differentiated thyroid cancer.
This cancer type grows slowly. Although papillary thyroid cancer often spreads to lymph nodes in the neck, the disease responds very well to treatment. Papillary thyroid cancer is highly curable and rarely fatal.
. Follicular thyroid cancer. Follicular thyroid cancer accounts for up to 15% of thyroid cancer diagnoses. Follicular thyroid cancer also arises from the follicular cells of the thyroid. It usually affects people older than age 50. Hurthle cell cancer is a rare and potentially more aggressive type of follicular thyroid cancer.
This cancer is more likely to spread to bones and organs, like the lungs.
. Anaplastic thyroid cancer. This rare cancer type accounts for about 2% of thyroid cancer diagnoses. Anaplastic thyroid cancer is a rare type of thyroid cancer that begins in the follicular cells. It grows rapidly and is very difficult to treat. Anaplastic thyroid cancer typically occurs in adults age 60 and older.
It can grow quickly and often spreads into surrounding tissue and other parts of the body.

. Medullary thyroid cancer. About 2% of thyroid cancers are medullary. A quarter of people with medullary thyroid cancer have a family history of the disease.
Medullary thyroid cancer begins in thyroid cells called C cells, which produce the hormone calcitonin. Elevated levels of calcitonin in the blood can indicate medullary thyroid cancer at a very early stage. Certain genetic syndromes increase the risk of medullary thyroid cancer, although this genetic link is uncommon.
. Other rare types. Other very rare types of cancer that start in the thyroid include thyroid lymphoma, which begins in the immune system cells of the thyroid, and thyroid sarcoma, which begins in the connective tissue cells of the thyroid.
Treatment
Your thyroid cancer treatment options depend on the type and stage of your thyroid cancer, your overall health, and your preferences.
Most thyroid cancers can be cured with treatment.
Treatment may not be needed right away
Very small thyroid cancers that have a low risk of spreading in the body might not need treatment right away. Instead, you might consider active surveillance with frequent monitoring of the cancer. Your doctor might recommend blood tests and an ultrasound exam of your neck once or twice per year.
In some people, the cancer might never grow and never require treatment. In others, growth may eventually be detected and treatment can be initiated.
Surgery
Most people with thyroid cancer undergo surgery to remove the thyroid. Which operation your doctor might recommend depends on the type of thyroid cancer, the size of the cancer, whether the cancer has spread beyond the thyroid and the results of an ultrasound exam of the entire thyroid gland.
Operations used to treat thyroid cancer include:
. Removing all or most of the thyroid (thyroidectomy). An operation to remove the thyroid gland might involve removing all of the thyroid tissue (total thyroidectomy) or most of the thyroid tissue (near-total thyroidectomy). The surgeon often leaves small rims of thyroid tissue around the parathyroid glands to reduce the risk of damage to the parathyroid glands, which help regulate the calcium levels in your blood.
. Removing a portion of the thyroid (thyroid lobectomy). During a thyroid lobectomy, the surgeon removes half of the thyroid. It might be recommended if you have a slow-growing thyroid cancer in one part of the thyroid and no suspicious nodules in other areas of the thyroid.
. Removing lymph nodes in the neck (lymph node dissection). When removing your thyroid, the surgeon may also remove nearby lymph nodes in the neck. These can be tested for signs of cancer.
Thyroid surgery carries a risk of bleeding and infection. Damage to your parathyroid glands also can occur during surgery, which can lead to low calcium levels in your body.
There’s also a risk that the nerves connected to your vocal cords might not work normally after surgery, which can cause vocal cord paralysis, hoarseness, voice changes or difficulty breathing. Treatment can improve or reverse nerve problems.
Thyroid hormone therapy
After thyroidectomy, you may take the thyroid hormone medication levothyroxine (Levoxyl, Synthroid, others) for life.
This medication has two benefits: It supplies the missing hormone your thyroid would normally produce, and it suppresses the production of thyroid-stimulating hormone (TSH) from your pituitary gland. High TSH levels could conceivably stimulate any remaining cancer cells to grow.
Radioactive iodine
Radioactive iodine treatment uses large doses of a form of iodine that’s radioactive.
Radioactive iodine treatment is often used after thyroidectomy to destroy any remaining healthy thyroid tissue, as well as microscopic areas of thyroid cancer that weren’t removed during surgery. Radioactive iodine treatment may also be used to treat thyroid cancer that recurs after treatment or that spreads to other areas of the body.
Radioactive iodine treatment comes as a capsule or liquid that you swallow. The radioactive iodine is taken up primarily by thyroid cells and thyroid cancer cells, so there’s a low risk of harming other cells in your body.
Side effects may include:
. Dry mouth
. Mouth pain
. Eye inflammation
. Altered sense of taste or smell
. Fatigue
Most of the radioactive iodine leaves your body in your urine in the first few days after treatment. You’ll be given instructions for precautions you need to take during that time to protect other people from the radiation. For instance, you may be asked to temporarily avoid close contact with other people, especially children and pregnant women.
External radiation therapy
Radiation therapy can also be given externally using a machine that aims high-energy beams, such as X-rays and protons, at precise points on your body (external beam radiation therapy). During treatment, you lie still on a table while a machine moves around you.
External beam radiation therapy may be recommended if surgery isn’t an option and your cancer continues to grow after radioactive iodine treatment. Radiation therapy may also be recommended after surgery if there’s an increased risk that your cancer will recur.
Chemotherapy
Chemotherapy is a drug treatment that uses chemicals to kill cancer cells. Chemotherapy is typically given as an infusion through a vein. The chemicals travel throughout your body, killing quickly growing cells, including cancer cells.
Chemotherapy isn’t commonly used in the treatment of thyroid cancer, but it’s sometimes recommended for people with anaplastic thyroid cancer. Chemotherapy may be combined with radiation therapy.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Targeted drug therapy for thyroid cancer targets the signals that tell cancer cells to grow and divide. It’s typically used in advanced thyroid cancer.
Injecting alcohol into cancers
Alcohol ablation involves injecting small thyroid cancers with alcohol using imaging such as ultrasound to ensure precise placement of the injection. This procedure causes thyroid cancers to shrink.
Alcohol ablation might be an option if your cancer is very small and surgery isn’t an option. It’s also sometimes used to treat cancer that recurs in the lymph nodes after surgery.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care.
Palliative care can be used while undergoing other aggressive treatments, such as surgery, chemotherapy or radiation therapy. Increasingly, it’s being offered early in the course of cancer treatment.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve quality of life for people with cancer and their families.
After Thyroid Cancer Treatment
After thyroid surgery
. Your wound
Your neck wound is usually closed with stitches that are under the skin surface and dissolve over a few weeks. Sometimes surgeons use clips rather than stitches. Clips need to be removed a few weeks after the operation. You may have a sore throat, but this will improve within a few days.
When you wake up, you will have several different tubes going into your body. This can be a bit frightening. But it helps to know what they are all for. You will have:
. A drip (intravenous infusion) to give you fluids until you are drinking again
. One or more tubes (drains) coming out from your wound
Your nurse can normally take out the drip and drains within 24 hours of the surgery.
The tube coming out from the wound will be connected to a drainage bottle or bag. It is there to stop blood and fluids from collecting inside your wound and causing swelling.
Sometimes there is swelling in your neck during your operation. The surgeon may need to make a small hole in your neck (tracheostomy) to help you breathe. This is usually only for a short time until the swelling settles down.
. Painkillers
It is normal to have some pain and stiffness after your operation.
There are many different painkilling drugs you can have. It is important to tell your doctor or nurse as soon as you feel any pain. They can then find the right type and dose of painkiller for you. Painkillers work best when you take them regularly.
You will probably find it uncomfortable to swallow for a few days after your operation. It may help to have a soft diet for a while. You can talk to a dietician about this if you need to. Or your nurse may give you a diet sheet to take home with you.
. Going home
You will be encouraged to be up and about on the first day after your surgery. Most people are in hospital for one or more nights and are then able to go home.
You may go back to the hospital or to your GP surgery every few days for a nurse to check your wound. You will have the phone number of the hospital ward and can call them if you are worried about anything.
It’s important that you don’t do too much and tire yourself out. It may help to prepare or buy some meals in advance that you can just heat up once you are at home.
You will have some exercises to do, to help you with the stiffness in your neck. Normally, you can start these a day or two after surgery. You should keep doing them until you can move your neck and shoulder as freely as you could before. This will be within a few weeks of your operation.
. Your scar
The scar after a thyroid operation is usually a horizontal line towards the bottom and front of your neck. It can be about 3 to 4 inches wide.
After your operation, the scar will be red and sore. But this usually heals well and becomes quite faint after 6 months to one year. Some people can have long term problems with a thick and red scar. Talk to your healthcare team if this is the case.
. Follow up appointments
You will have follow up appointments to check your recovery. This may include blood tests to check hormone and calcium levels if you need them. Your appointments are also an opportunity to raise any concerns you have about your progress.
What is the prognosis (outlook) for people who have thyroid cancer?
Eight out of 10 people who have thyroid cancer develop the papillary type. Papillary thyroid cancer has a five-year survival rate of almost 100% when the cancer is in the gland (localized). Even when the cancer spreads (metastasizes), the survival rate is close to 80%. This rate means that, on average, you’re about 80% as likely to live for at least five years after diagnosis as someone who doesn’t have metastatic papillary thyroid cancer.
Five-year survival rates for other thyroid cancer types include:
. Follicular: Close to 100% for localized; around 63% for metastasized.
. Medullary: Close to 100% for localized; around 40% for metastasized.
. Anaplastic: Close to 31% for localized; 4% for metastasized.
How does thyroid cancer affect pregnancy?
Thyroid cancer is the second most common cancer diagnosed in pregnant women (breast cancer is first). Approximately 10% of thyroid cancers develop during pregnancy or within the first year after childbirth. Experts believe fluctuating hormone levels during pregnancy may trigger the cancer.
If you receive a thyroid cancer diagnosis during pregnancy, your healthcare provider can discuss treatment options. Depending on the cancer type and severity, your provider may recommend delaying treatment until after you deliver your baby. If treatment can’t wait, most women can safely undergo surgery to remove the cancerous gland. You shouldn’t have radioactive diagnostic tests or treatments when you’re pregnant or breastfeeding.
When should I call the doctor?
You should call your healthcare provider if you have thyroid cancer and you experience:
. Lump in the neck.
. Rapid heart rate.
. Unexplained weight loss or gain.
. Extreme fatigue.
Sources:
https://my.clevelandclinic.org/health/diseases/12210-thyroid-cancer
https://www.mayoclinic.org/diseases-conditions/thyroid-cancer/diagnosis-treatment/drc-20354167
https://www.nhs.uk/conditions/thyroid-cancer/treatment/
https://www.cancer.org/cancer/thyroid-cancer/treating/by-stage.html
https://www.cancer.net/cancer-types/thyroid-cancer/types-treatment