Orchiectomy
What is an orchiectomy?
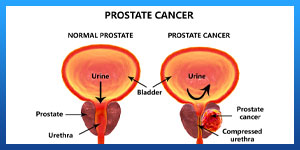
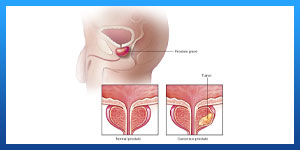
An orchiectomy surgery is done to remove one or both of your testicles. It’s commonly performed to treat or prevent prostate cancer from spreading.
An orchiectomy may be used to treat some cases of:
. Testicular and/or prostate cancer.
. Male breast cancer.
. Cancer prevention in men with an undescended testicle after puberty.
. Severe trauma.
. Male-to-female gender reassignment surgery.
Read more about : Testicular Cancer Treatment
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Surgeons to treat your prostate cancer in Iran. The price of Orchiectomy in Iran can vary according to each individual’s case and will be determined by the type of Orchiectomy surgery and an in-person assessment with the doctor. So if you are looking for the cost of Orchiectomy surgery in Iran, you can contact us and get free consultation from Iranian surgery.
Read more about : Metastatic myxofibrosarcoma treatment with the best Iranian oncologist surgeon
Before Orchiectomy
Who is a good candidate for an orchiectomy?
Your doctor may do this surgery to treat breast cancer or prostate cancer. Without the testicles, your body can’t make as much testosterone. Testosterone is a hormone that can cause prostate or breast cancer to spread more quickly. Without testosterone, the cancer may grow at a slower rate, and some symptoms, such as bone pain, may be more bearable.
Your doctor may recommend orchiectomy if you’re in generally good health, and if the cancer cells have not spread beyond your testicles or far beyond your prostate gland.
You may want to do an orchiectomy if you’re transitioning from male to female and want to reduce how much testosterone your body makes.
How do I prepare for this procedure?
Before an orchiectomy, your doctor may take blood samples to make sure you’re healthy enough for surgery and to test for any indicators of cancer.
This is an outpatient procedure that takes 30-60 minutes. Your doctor may use either local anesthesia to numb the area or general anesthesia. General anesthesia has more risks but lets you remain unconscious during the surgery.
Before the appointment, be sure that you have a ride home. Take a few days off work and be ready to limit your amount of physical activity after the surgery. Tell your doctor about any medications or dietary supplements that you’re taking.
Read more about : Newest prostate cancer treatments
Risks and side effects of orchiectomy
As with any surgery, there are risks and possible side effects. These can be:
. Reaction to anesthesia.
. Bleeding.
. Infection.
. Blood clots.
. Loss of fertility.
. Erectile dysfunction.
. Loss of feeling in the groin and/or genitals.
. Low libido (sex drive).
. Hot flashes, mood swings, depression.
. Loss of muscle mass.
. Osteoporosis.
. Breast enlargement (gynecomastia).
. Weight gain.
. Fatigue.
. Fever over 100°F (37.8°C).
. Inability to urinate.
. Hematoma, which is blood in the scrotum and usually looks like a large purple spot.
. Change in self-image.
Transgender women who undergo an orchiectomy are also likely to experience a number of positive side effects, including:
. A drastic decrease in testosterone, which may allow you to reduce your dose of feminizing hormones
. Reduced gender dysphoria as you take a step closer to matching your physical appearance with your gender identity.
Read more about : Penile implant
 Disadvantages
Disadvantages
What are the disadvantages of orchiectomy?
The major disadvantage appears to be the psychological one associated with “loss of manhood.” For many men this loss appears to be all but unbearable. Interestingly, the loss of “manhood” is not usually a problem for the partners of most prostate cancer patients when compared to the possibility of loss of life. However, the male association between his theoretical ability to be able to have sexual intercourse and his sense of self-worth appears to be astonishingly strong, regardless of the truth about his actual level of sexual activity and/or capability.
The other disadvantage is that the procedure is not reversible. However, since cases of complete remission of advanced prostate cancer are almost completely unheard of and certainly not well documented, it would appear that the need for reversing this operation is about as close to zero as one can get!
During Orchiectomy
Types of orchiectomy
What are the types of orchiectomy?
There are different types of orchiectomy, including:
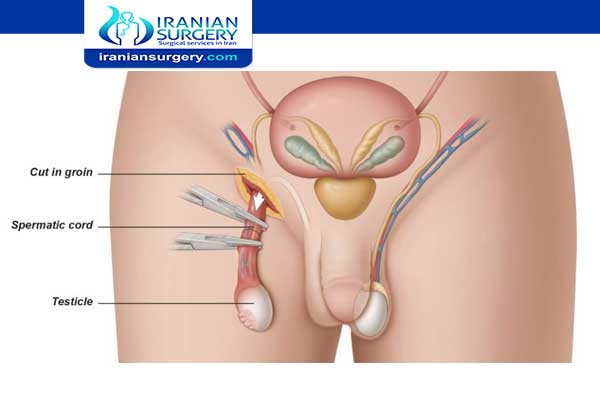
. Radical Inguinal Orchiectomy: The testicle and spermatic cord are removed through an incision made in the groin. At times, a prosthetic saline-filled testicular implant can be inserted.
. Simple Orchiectomy: During a simple orchiectomy, the testicle is removed through the scrotum. As in a radical inguinal orchiectomy, a prosthetic testicle can be inserted. In both simple and radical orchiectomy, a single testicle can be removed, or both testicles, which is called bilateral orchiectomy.
. Subcapsular Orchiectomy: During a subcapsular orchiectomy, the glandular tissue lining the testicles is removed, leaving the testicles in place.
. Bilateral orchiectomy: Both testicles are removed. This may be done if you have prostate cancer, breast cancer, or are transitioning from male to female.
During Procedure
How is this procedure done?
First, your surgeon will lift your penis and tape it to your abdomen. Then, they’ll make an incision either on your scrotum or the area right above your pubic bone on your lower abdomen. One or both testicles are then cut out from the surrounding tissues and vessels, and removed through the incision.
Your surgeon will use clamps to prevent your spermatic cords from gushing blood. They may put in a prosthetic testicle to replace the one that’s removed. Then, they’ll wash the area with a saline solution and sew the incision shut.
After Orchiectomy
Recovery
Recovery from an orchiectomy may include a short stay in the hospital, depending on the extent of the procedure you have had. You will be taught incisional care before being discharged from the hospital.
Your medical team will discuss with you the medications you will be taking (blood clot and infection prevention, pain management, nausea management, and constipation prevention.
These dos and don’ts after surgery will help you heal:
. Keep an ice pack or cold compress on your scrotum to ease swelling. It should get better in a few days. Don't keep the ice on for more than 15 minutes at a time.
. Your surgeon probably will suggest you wear a jockstrap or snug underwear for a few days to help with swelling, too.
. Take pain medicine as prescribed. Don't drive until you've stopped taking medicine and your doctor says it's OK.
. Your doctor will tell you when you can shower. You'll have to skip baths and swimming until the cut made during surgery heals.
. The doctor will show you how to take care of your cut. Check it every day for signs of infection or other problems.
. If you had surgery due to cancer, you may have to have chemotherapy or radiation to lower the chances that any leftover cancer cells will spread.
For the first week after an orchiectomy:
. Wash the area gently with a mild soap when you bathe.
. Keep your incision area dry and covered in gauze for the first few days.
. Use any creams or ointments following your doctor’s instructions.
. Take nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) for your pain.
. Avoid straining during bowel movements. Drink lots of water and eat high-fiber foods to keep bowel movements regular. You can also take a stool softener.
It can take two weeks to two months to fully recover from an orchiectomy. Don’t lift anything over 10 pounds for the first two weeks or have sex until the incision has fully healed. Avoid exercise, sports, and running for four weeks after surgery.
Life after Orchiectomy
Having one or both testicles removed can change the way you feel about your body. Surgery may affect how you look, your fertility, and your interest in sex.
You may be concerned about how you look to a partner or in a locker room. If it’s a problem, you can have surgery to implant an artificial testicle. It's filled with saline and is made to look like the real thing. There will be a small scar, but your pubic hair can help hide it.
If you still have one testicle, you should still be able to get an erection and have sex. If both are removed, your body won't be able to make sperm. If you want to have children, you may want to store sperm before the procedure. Talk to your doctor to plan ahead.
Without both testicles, your body won't be able to make as much testosterone as it needs. That might lower your sex drive and make it harder to have erections. You could have hot flashes, lose some muscle mass, and be more tired than usual. Talk to your doctor about a testosterone gel, patch, or shot that will help ease these symptoms.
When do I call my healthcare team?
Call your healthcare team if you have any of the following:
. Fever or chills. Your team will tell you at what temperature they should be contacted.
. Groin redness and/or swelling.
. Swelling in the scrotum.
. Drainage and/or bleeding at the incision.
. Not being able to urinate.
Outlook
An orchiectomy is an outpatient surgery that doesn’t take long to fully recover from. It’s much less risky than hormone therapy for the treatment of prostate or testicular cancer.
Be open with your doctor if you’re getting this surgery as part of your transition from male to female. Your doctor may be able to work with you to reduce scar tissue in the area so that future SRS may be more successful.
10 common questions about Orchiectomy surgery for prostate cancer
Related Posts:
- Can egg donation cause cancer?
- Testicular Cancer and Fertility
- What Are the Chances of Getting Pregnant After…
- Nose Tip Surgery
- What Is a Full Body Surgery?
- Can Gastric Bypass Surgery Fail
- Can Gastric Bypass Surgery Kill You?
- How Much Smaller Do Breast Implants Get After Surgery?
- What Are the Side Effects of Lipomatic Surgery?


4 Comments
hello I’m jake Nikson. I’m 55 years old. none smoker and don’t use any drug. I have diagnosed with prostate cancer gleason score of 7.I’ve heard that if gleason score is 7 or higher its a death sentence would you mind help me on this matter? what should I do?
Hello Jake. There is a perception among a lot of patients — especially when they get diagnosed — that having a high Gleason score of 8, 9, or 10 is essentially a “death sentence”, regardless of how they get treated. This is not actually the case at all. Plenty of men with Gleason 8 to 10 disease actually do well after treatment.
now with having a score of 7 you shouldn’t loose your morale,start Contacting your doctor and start the treatment. if you need anymore information feel free to Contact us on what’s app via this number +989019290946
hello Doc, this is Jasem 63 year old man from oman
I have diagnosed with prostate cancer and they have suggested Oriechtomy for me
I wanted to know if you can give me an estimate of how successful is Oriechtomy on prostate cancer?
Hello Jasem Oriechtomy is one of the most common operations for prostate cancer and the success rate is around 90 percent
for more information please message our agents via what’s app on this number +989019290946