Rectocele Repair
What is a Rectocele?
A rectocele is a type of pelvic organ prolapse. It happens when the supporting ligaments and muscles weaken in the pelvic floor. Other names for a rectocele are a posterior vaginal wall prolapse or proctocele.
Childbirth, age, and a range of other factors can cause the normally tough, fibrous, sheet-like divider between the rectum and vagina to weaken.
A bulge may protrude as a hernia into the back of the vagina during a time of straining, such as a bowel movement.
A rectocele can lead to constipation and discomfort, but if it is small, there may be no symptoms. Most people can treat a rectocele at home, but a severe case may need surgery.
Read more about : how to pop a bartholin cyst yourself?
Read more about : ovarian cyst size chart
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Surgeons to treat your Rectocele in Iran. The price of treating a Rectocele in Iran can vary according to each individual’s case and will be determined by the type of treatment you have and an in-person assessment with the doctor. So if you are looking for the cost of Rectocele treatment in Iran, you can contact us and get free consultation from Iranian surgery.
Before Rectocele Repair
Symptoms
A small posterior vaginal prolapse (rectocele) may cause no signs or symptoms.
Otherwise, you may notice:
. A soft bulge of tissue in your vagina that might protrude through the vaginal opening.
. Difficulty having a bowel movement
. Sensation of rectal pressure or fullness
. A feeling that the rectum has not completely emptied after a bowel movement
. Sexual concerns, such as feeling embarrassed or sensing looseness in the tone of your vaginal tissue.
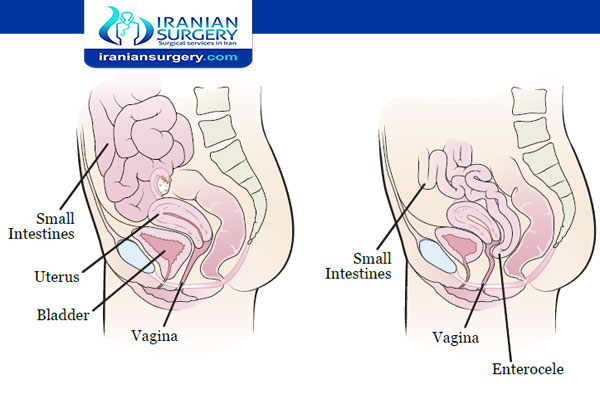
Many women with posterior vaginal prolapse also experience prolapse of other pelvic organs, such as the bladder, uterus or — for women who have had surgery to remove the uterus (hysterectomy) — the top of the vagina.
]
When to see a doctor
Posterior vaginal prolapse (rectocele) is common, even in women who haven’t had children. In fact, you may not even know you have posterior vaginal prolapse.
But sometimes moderate or severe posterior vaginal prolapses can be bothersome or uncomfortable. See your doctor if:
. You have a bothersome bulge of tissue that protrudes through your vaginal opening.
. Constipation treatment isn’t successful at producing soft and easy-to-pass stool between three times a day to three times a week.
Read more about : clitoromegaly surgery pictures
Read more about : amoxicillin for bartholin cyst
Causes
Posterior vaginal prolapse (rectocele) results from pressure on the pelvic floor. Causes of increased pelvic floor pressure include:
. Chronic constipation or straining with bowel movements
. Chronic cough or bronchitis
. Repeated heavy lifting
. Being overweight or obese
Pregnancy and childbirth
The muscles, ligaments and connective tissue that support your vagina become stretched and weakened during pregnancy, labor and delivery. The more pregnancies you have, the greater your chance of developing posterior vaginal prolapse.
Women who have had only cesarean deliveries are less likely to develop posterior vaginal prolapse, but still may.
Risk factors
Factors that may increase your risk of posterior vaginal prolapse include:
. Genetics. Some women are born with weaker connective tissues in the pelvic area, making them naturally more likely to develop posterior vaginal prolapse.
. Childbirth. If you have vaginally delivered multiple children, you have a higher risk of developing posterior vaginal prolapse. If you’ve had tears in the tissue between the vaginal opening and anus (perineal tears) or incisions that extend the opening of the vagina (episiotomies) during childbirth, you may also be at higher risk.
. Aging. As you grow older, you naturally lose muscle mass, elasticity and nerve function, causing muscles to stretch or weaken.
. Obesity. Extra body weight places stress on pelvic floor tissues.
Read more about : Cervical cancer treatment
Read more about : Risk factors of cervical cancer
Diagnosis
A diagnosis of rectocele generally occurs during a pelvic exam of your vagina and rectum.
During the pelvic exam your doctor is likely to ask you:
. To bear down as if having a bowel movement. Bearing down may cause the posterior vaginal prolapse to bulge, so your doctor can assess its size and location.
. To tighten your pelvic muscles as if you’re stopping a stream of urine. This test checks the strength of your pelvic muscles.
You might fill out a questionnaire that helps your doctor assess how far the bulge extends into your vagina and how much it affects your quality of life. This information helps guide treatment decisions.
Rarely, your doctor might recommend imaging tests:
. MRI or an X-ray can determine the size of the tissue bulge
. Defecography can determine how efficiently your rectum empties
Read more about : Early symptoms of Cervical cancer
Risks and Complications
What complications can occur after rectocele repair?
Risks of surgical rectocele repair include the following:
. Bleeding.
. Infection.
. Urinary retention.
. Bladder injury.
. Bowel or rectal injury.
. Pain during sexual intercourse.
. Development of a fistula (an open channel) between the vagina and rectum.
. Recurrence of the rectocele.
Prevention
To reduce your risk of worsening posterior vaginal prolapse (rectocele), try to:
. Perform Kegel exercises regularly. These exercises can strengthen your pelvic floor muscles — especially important after you have a baby.
. Treat and prevent constipation. Drink plenty of fluids and eat high-fiber foods, such as fruits, vegetables, beans and whole-grain cereals.
. Avoid heavy lifting and lift correctly. When lifting, use your legs instead of your waist or back.
. Control coughing. Get treatment for a chronic cough or bronchitis, and don’t smoke.
. Avoid weight gain. Talk with your doctor to determine your ideal weight and get advice on weight-loss strategies, if you need them.
During Rectocele Repair
Treatment
Depending on how severe the rectocele is, a doctor may suggest home remedies, medication, or, in some cases, surgery.
Home remedies
The following tips can help prevent a rectocele from developing, and — if a rectocele is already present — stop symptoms from getting worse.
. Pelvic floor exercises, such as Kegel exercises, can strengthen the pelvic floor muscles.
. Drinking plenty of fluids and eating high-fiber foods can reduce constipation.
. Avoiding any type of heavy lifting can also prevent a worsening of symptoms.
. Getting treatment for prolonged coughing can reduce strain on the pelvic floor muscles.
. Losing weight may be advisable if a person has obesity or excess weight.
Straining for a long time when defecating can make the problem worse. Avoiding constipation can help prevent this.
Medications
The doctor may prescribe:
. Stool softeners to ease constipation
. Hormone replacement therapy (HRT) for use after menopause.
. A vaginal pessary — a plastic or rubber round disk inserted into the vagina — to support the protruding tissues.
Surgery
What types of surgical repairs are available for a rectocele?
If non-surgical methods do not help control rectocele symptoms, surgery may be needed. Talking with a reconstructive surgeon who specializes in pelvic floor conditions can help women decide upon the best approach. In most cases, surgery is done under general anesthesia and takes approximately 1 hour.
There are a number of different surgical repair options, each of which takes its name from the path used by the surgeon to reach the rectocele.
. Transvaginal repair: The rectocele is reached through the vagina. This is the traditional approach to rectocele repair by gynecologists. It offers the chance to correct not only the rectocele but a relaxed perineum and widened vaginal opening. It also has the advantage of not disturbing any tissue in the rectal area.
. Transperineal repair: The rectocele is reached through the perineum. This method allows the surgical removal of hemorrhoids at the same time, if necessary. However, it usually requires the implanting of a mesh over the entire surgical area to provide added support following surgery.
. Transanal repair: The rectocele is reached through the anus. This method is preferred by many colorectal surgeons because it allows for correction of problems in the anal or rectal area, in addition to repairing the rectocele. Some studies also suggest that pain after surgery may be less with this method than with the transvaginal approach.
Other types of repairs include:
. Laparoscopic repair uses a laparoscope, a thin lighted tube that needs only a small opening to reach the area being repaired. Advantages to this method include clearer visibility of the affected area, quicker recovery time, less pain, and a shorter hospital stay. Disadvantages include difficulties with suturing, increased procedure time and expense, and extra time on the part of the surgeon to master laparoscopic techniques.
. Ventral-rectopexy involves the use of a polypropylene (flexible plastic) mesh that is stitched to the front of the rectum and attached to the back of the pelvis (the hip bone) using special types of tacks. The mesh pulls up the bowel and prevents it from sagging down into the vaginal wall. This operation may be performed using a laparoscope.
Other types of mesh are made from the tissue surrounding a cow’s heart, or from pig skin and intestine. These materials closely resemble the type of tissue found along the wall of the vagina.
After Rectocele Repair
What is the long-term outlook following rectocele repair?
The degree of success after rectocele repair depends on a number of factors, including:
. Type of symptoms present.
. Length of time the symptoms have been present.
. Surgical method and approach taken.
Studies show about 75% to 90% of patients have significant improvement but this level of satisfaction decreases over time.
Recovery
How do I care for myself at home?
Immediately after Surgery:
. You will wake up with a catheter in your bladder and possibly a pack in your vagina, as well as those compression stockings.
. On the first day after your surgery the packing and catheter usually come out. The nurse may check to see if you have emptied your bladder all the way with an ultrasound scanner or by passing a catheter after you try to void. For patients who cannot empty their bladder completely, the nurse will teach you to pass the catheter on your own (self-Cath). Your diet is generally started as only liquids and advanced as you are able. Most often, you can be switched from IV pain medications to oral medications. Also, you will be encouraged to sit in a chair, go for some short walks, and generally increase your activity. Most patients go home on the day after their surgery.
Week 1:
. Rest at home; not responsible for making meals for other, or major care of children, or relatives.
. Up and around the house as desired including stairs if necessary; do not become overtired, take an afternoon nap.
. May shower.
. Stick to a simple diet (light foods and liquids) until your first bowel movement, and then you may eat what you like.
. Refrain from intercourse for six weeks.
. Use either the prescription for pain, or Tylenol or Advil (ibuprofen) equivalent for pain.
Weeks 2 & 3:
. Increase your activity as desired, but avoid all major housekeeping chores.
. Walking inside or outside is encouraged, but do not become overtired.
. Rest for one hour each afternoon.
. You may drive a car when you have no pain.
Weeks 4-12:
. All activities are OK except heavy housework or exercise.
. Discuss return to work with your doctor.
. It remains important not to become overtired or to perform any heavy lifting, strenuous exercise or physically demanding duties for a total of six weeks from the date of operation. Healing is not complete for 12 weeks (3 months) from the time of surgery.
Rectocele Repair Cost
How much does rectocele repair surgery cost in Iran?
The cost of rectocele repair surgery in Iran starts from $ 340.