ICSI Advantages and Disadvantages
What are the pros and cons of ICSI over IVF?
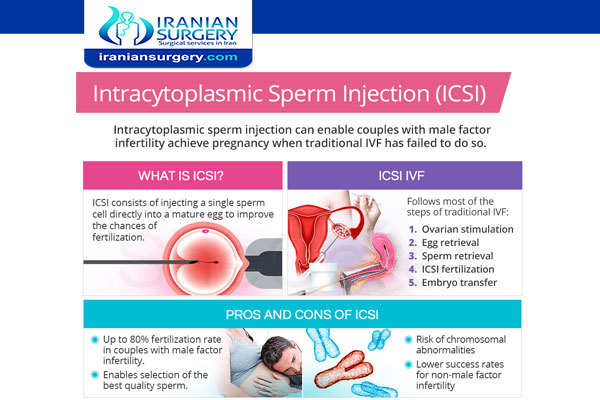
ICSI, intracytoplasmic sperm injection was developed in 1988 as a treatment for male infertility, i.e., men with very poor sperm parameters, to treat failure of fertilization with IVF. ICSI is now used routinely in many IVF programs as the fertilization rate is higher than with standard fertilization techniques and the pregnancy rates are higher. There is inadequate information about a possible increase in congenital anomalies with ICSI. There appears to be an increased risk of identical twinning with ICSI, especially with transferring blastocysts. This may be as high as 2%.
What are the advantages of ICSI?
The main advantage of intracytoplasmic sperm injection is that it can solve the problem of unexplained male and female infertility, when the causes of it are unknown and undefined. Nowadays, unfortunately, there are more and more such cases in the world and families have to seek the medical support to conceive a baby. It is expected, that in 2017 there will be more ICSI requests compared with previous years, taking into account disappointing medical statistics.
The leading reason why couples have to use intracytoplasmic sperm injection are serious male fertility disorders as:
- Low sperm count;
- Abnormal sperm morphology, bad motility;
- Low sperm production or no production owing to genetic disease or other illnesses;
- Issues with erection and ejuculating
- High antibodies level in the semen
In addition there can be other reasons why ICSI is preferable:
- The frozen sperm cannot be used because of low quality;
- Intended parents would like to examine the embryo to detect possible risks of genetic disorders.
What are the risks of ICSI?
In spite of numerous benefits of the ICSI infertility treatment, there is usually certain risk involved. First of all, it is multiple pregnancy that can have potential hazard both for a woman and children since multiple gestation may lead to premature birth and just like at the time of any impregnation there is the risk of ectopic pregnancy development. Also, there is always a possibility that inseminated egg won’t turn into a healthy embryo. Additionally, the children who were conceived due to intracytoplasmic sperm injection tent to be born more often with infantile cerebral paralysis than those children, who were conceived owing to in vitro. It is probable as well, that the baby will inherit male infertility. And last but not least, the ICSI is more expensive than in vitro fertilization treatment.
Controversial Reasons for Using IVF-ICSI
IVF with ICSI can be a great technology when needed. However, there’s some disagreement on when it can and can’t improve success rates. Research is ongoing, but here are some situations that the American Society of Reproductive Medicine reports IVF with ICSI may not be warranted:
- Very few eggs retrieved: The concern is that with so few eggs, why take a risk that they won’t get fertilized? However, research has not found that pregnancy or live birth rates are improved when ICSI is used.
- Unexplained infertility: The logic behind using ICSI to treat unexplained infertility is that since we don’t know what is wrong, treating every possibility is a good plan of action. That said, so far research has not found that ICSI for unexplained infertility significantly improves live birth success rates.
- Advanced maternal age: There’s no current evidence that advanced maternal age impacts fertilization rates. Therefore, ICSI may not be necessary.
- Routine IVF-ICSI (ie, ICSI for everyone): Some reproductive endocrinologists believe that every patient should get ICSI to eliminate the possibility of fertilization failure. However, research has found that for every 33 patients, only one would benefit from routine use of IVF-ICSI. The rest would be receiving the treatment (and risks) without possible benefit.
Is ICSI more successful than IVF?
Is ICSI better than IVF?
When IVF was first developed in the 1980s it helped many couples who had previously been infertile have children. But IVF didn’t work for couples where the man had very poor sperm. That’s why, in the early 1990s, the ICSI procedure was developed. ICSI has been remarkably successful and helped couples with male factor infertility around the world have children.
What is the difference between ICSI and IVF?
In assisted reproductive technology (ART) there are two ways eggs can be fertilised: IVF (in-vitro-fertilisation) or ICSI (intracytoplasmic sperm injection). In IVF thousands of sperm are added to each egg in the hope that one will fertilise the egg. In ICSI the embryologist uses a microscope and very technically advanced equipment to select a single sperm which is injected into the egg. A few days after IVF and ICSI the embryologist checks to see of the eggs have fertilised and developed into embryos. If there are embryos, one (sometimes two) is placed in the uterus and any remaining embryos can be frozen for later use if the treatment is not successful.
What is the success rate for ICSI?
The ICSI procedure fertilizes 50 to 80 percent of eggs. You might assume all eggs get fertilized with ICSI-IVF, but they don’t. Fertilization isn’t guaranteed even when a sperm is injected into the egg. New Scientist reports that a recent study revealed that ICSI boasts a pregnancy success rate of 24%. While IVF without ICSI still has a slightly higher pregnancy success rate at 27%, those aren’t bad odds for anyone who’s already tried other methods of assisted reproductive technology.
Does ICSI increase chance of having a girl?
ICSI with ejaculated sperm produces more girls (48.2% boys) ICSI with testicular sperm produces more girls (47.7% boys).
Read more about: Egg Freezing Advantages and Disadvantages