Spondylolysis
What is Spondylolysis?
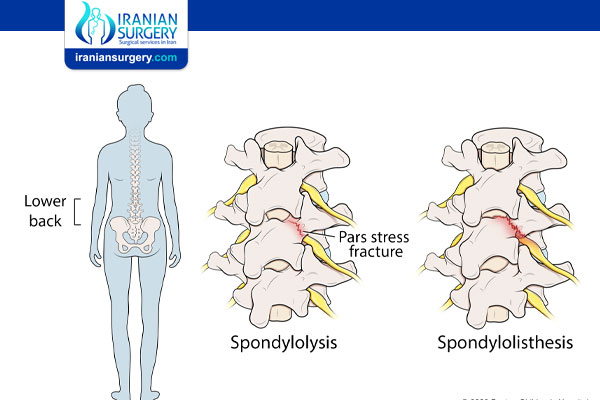
“Spondylolysis” is the medical term for a small crack (fracture) between two vertebrae in your spine. Your vertebrae are the 33 bones that make up your spinal column. A single bone in your spine is a vertebra — vertebrae is the plural form.
Healthcare providers sometimes refer to spondylolysis as pars defect or pars fractures because it affects your pars interarticularis — the tiny ridges of bone that link your vertebrae together.
Spondylolysis most commonly affects your lower back (lumbar spine), but it can also happen in the other sections of your spine — in your neck (cervical spine) or middle back (thoracic spine).
Before Spondylolysis Treatment
Symptoms and Causes
What are the symptoms of spondylolysis?
Lower back pain is the most common spondylosis symptom. The pain usually:
. Spreads (radiates) from your lower back into your thigh and butt muscles (buttocks).
. Feels like a muscle strain in or around your lower back.
. Gets worse during physical activity and improves with rest or when you’re less active.
Some people with spondylolysis never experience symptoms. These people may only learn they have it when they have an imaging test for another reason later on.
What causes spondylolysis?
Damage to part of your vertebrae called the pars interarticularis causes spondylolysis.
The pars interarticularis are thin pieces of bone that link your vertebrae directly above and below each other to form a working unit. These links let your spine move and flex. Anything that damages your pars interarticularis can crack them. Providers call these cracks pars fractures.
The most common causes of pars fractures include:
. Overuse: Repetitive motions that put stress on your low back cause wear and tear on your vertebrae. Over time, this damage can add up to cause a pars fracture. Doing physical work for your job, playing contact sports and repeatedly injuring your low back can all damage your vertebrae.
. Growth spurts: Some kids and teens develop spondylolysis when they’re going through a growth spurt — a period when their bodies are physically growing and changing quickly.
. Genetics: Some people are born with thinner vertebrae. This can make you more likely to experience a pars fracture.
Spondylolysis risk factors
Anyone can experience spondylolysis. Certain groups of people have a higher risk of a pars fracture, including:
. Athletes who play contact sports like football, gymnastics or weightlifting.
. Kids and teens whose bodies are still rapidly growing and changing.
. People of Indigenous Alaskan descent. Studies have found that people with Native Alaskan ethnicity are more likely to be born with thinner vertebrae.
What are the most common complications of spondylolysis?
The back pain that comes with spondylolysis can also lead to reduced mobility (how well or comfortably you can move).
Untreated spondylolysis can lead to spondylolisthesis. Spondylolisthesis happens when your vertebrae are cracked or weakened enough by spondylolysis to slip out of place. If a slipped vertebra presses on a nerve, you may develop shooting pain in your legs (sciatica). Some people need surgery to relieve spondylolisthesis symptoms and get back to their normal routine.
Diagnosis and Tests
How is spondylolysis diagnosed?
A healthcare provider will diagnose spondylolysis with a physical exam and imaging tests. They’ll ask you about your symptoms and medical history. Tell your provider when you first noticed pain in your back and what you were doing right before you started feeling it.
What tests are done to diagnose spondylolysis?
Your provider will use imaging tests to take pictures of your vertebrae and the tissue around your spine, including:
. X-rays.
. Magnetic resonance imaging (MRI).
. Computed tomography (CT) scans.
Prevention
Can spondylolysis be prevented?
You can’t usually prevent spondylolysis. Follow these general safety tips to reduce your risk of a pars fracture:
. Always wear your seatbelt, including the shoulder harness around the upper half of your body.
. Wear the right protective equipment for all activities and sports.
. Make sure your home and workspace are free from clutter that could trip you or others.
. Always use the proper tools or equipment at home to reach things. Never stand on chairs, tables or countertops.
. Follow a diet and exercise plan that will help you maintain good bone health.
. Talk to your provider about a bone density test if you’re older than 50 or if you have a family history of osteoporosis.
. Use a cane or walker if you have difficulty walking or have an increased risk of falls.
During Spondylolysis Treatment
Management and Treatment
How is spondylolysis treated?
Your provider will treat your pain and other symptoms to give the pars fracture time to heal. Depending on which vertebrae are affected and how severe the cracks are, you might need treatment anywhere from a few weeks up to a few months.
The most common spondylolysis treatments include:
. Rest: Taking a break from sports and other intense physical activities reduces stress on your spine.
. Medications: Over-the-counter NSAIDs can help reduce pain and inflammation. Don’t take over-the-counter pain relievers for more than 10 days in a row without talking to your provider.
. Corticosteroids: Corticosteroids reduce inflammation. Your provider might prescribe you an oral medication that you’ll take by mouth. They might also inject medication directly into the affected area to help relieve pain.
. Physical therapy: A physical therapist is a healthcare provider who helps you improve how your body performs physical movements. They’ll help you manage symptoms like pain, stiffness and discomfort that make it hard to move. A physical therapist will give you exercises that will strengthen the muscles around your spine.
. Bracing: Your provider might recommend you wear a back brace to stabilize your spine while the pars fracture heals.
Does spondylolysis require surgery?
It’s rare to need surgery for spondylolysis. Most of the time, people feel better with nonsurgical treatments.
Some people need surgery to stabilize their spine. During a pars repair surgery, your surgeon can usually fix a pars fracture without needing to perform a spinal fusion (fusing two vertebrae together to form one bone). If you need surgery, your provider or surgeon will tell you what to expect and how long it will take to recover.
How long does spondylolysis take to heal?
Pars fractures can take up to six months to heal. Most people with spondylolysis begin feeling better as soon as they start treatment. Follow your treatment plan for as long as your provider or physical therapist suggests, even if your symptoms start to get better sooner. It’s important to give your spine all the time it needs to heal completely.
Ask your provider when you can start playing sports or doing intense physical activity again.
After Spondylolysis Treatment
Outlook / Prognosis
What can I expect if I have spondylolysis?
If you have spondylolysis, nonsurgical treatments like rest, medication and physical therapy should improve your symptoms. These treatments can’t undo the fracture, but they can help you return to your daily activities without pain as soon as possible.
When can I return to physical activities and sports?
Talk to your provider before resuming intense physical activity. Even if your pain and other symptoms have improved, your vertebrae need time to heal.
Your provider will monitor your treatment progress. As you start to have less pain and more flexibility, you’ll be able to return to your regular activities gradually. People recovering from spondylolysis usually need at least a few weeks (and up to a few months) of treatment before they can resume intense physical activities like playing sports and working out.
When should I see my healthcare provider?
The sooner you see a healthcare provider, the faster they can diagnose and treat spondylolysis. Visit a healthcare provider as soon as you notice low back pain that lasts more than a few days or is severe enough that it makes it hard or impossible to participate in your usual routine.
When should I go to the emergency room?
Go to the emergency room if you experience a trauma like a fall or car accident. Go to the ER if you lose feeling or can’t move a part of your body.
What is the difference between spondylolysis and spondylolisthesis?
Spondylolysis and spondylolisthesis are related conditions that affect your spine.
. Spondylolisthesis is when one vertebra slips out of place over the vertebra below it in your spine.
. Spondylolysis is a common cause of spondylolisthesis, because the crack (called a pars fracture) in a vertebra can cause it to slip out of place and become spondylolisthesis.
What is the difference between spondylolysis and spondylosis?
Spondylolysis and spondylosis have similar sounding names and are both conditions that affect your spine. They both also cause symptoms like pain and stiffness.
Spondylolysis is a specific injury — having a pars fracture in the pars-interarticularis in your spine.
Spondylosis is a general term that applies to any age-related breakdown (degeneration) in your spine.
Will spondylolysis go away on its own?
Pars fractures involved in spondylolysis usually heal over time. But a healthcare provider should still diagnose and treat them. Visit a provider if you’re experiencing lower back pain that lasts more than a few days or is severe enough to affect your daily routine. They’ll suggest treatments that will make sure your vertebrae heal safely and as fast as possible.
Source:
. https://my.clevelandclinic.org/health/diseases/10303-spondylolysis