How treatable is colon cancer?
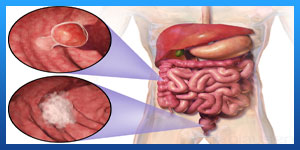
What is Colon Cancer?
Colon cancer is a type of cancer that begins in the large intestine (colon). The colon is the final part of the digestive tract.
Colon cancer typically affects older adults, though it can happen at any age. It usually begins as small, noncancerous (benign) clumps of cells called polyps that form on the inside of the colon. Over time some of these polyps can become colon cancers.
If colon cancer develops, many treatments are available to help control it, including surgery, radiation therapy and drug treatments, such as chemotherapy, targeted therapy and immunotherapy.
Colon cancer is sometimes called colorectal cancer, which is a term that combines colon cancer and rectal cancer, which begins in the rectum.
Read more about : Rectal Cancer Staging
Read more about : What is colorectal cancer?
Read more about : Metastatic myxofibrosarcoma treatment with the best Iranian oncologist surgeon
Read more about : How do hemorrhoids just go away?
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Surgeons to treat your colon cancer in Iran. The price of treating a colon cancer in Iran can vary according to each individual’s case and will be determined by the type of treatment you have and an in-person assessment with the doctor. So if you are looking for the cost of colon cancer treatment in Iran, you can contact us and get free consultation from Iranian surgery.

Before Colon Cancer Treatment
The colon and rectum
To understand colorectal cancer, it helps to know about the normal structure and function of the colon and rectum.
The colon and rectum make up the large intestine (or large bowel), which is part of the digestive system, also called the gastrointestinal (GI) system (see illustration below).
Most of the large intestine is made up of the colon, a muscular tube about 5 feet (1.5 meters) long. The parts of the colon are named by which way the food is traveling through them.
. The first section is called the ascending colon. It starts with a pouch called the cecum, where undigested food is comes in from the small intestine. It continues upward on the right side of the abdomen (belly).
. The second section is called the transverse colon. It goes across the body from the right to the left side.
. The third section is called the descending colon because it descends (travels down) on the left side.
. The fourth section is called the sigmoid colon because of its “S” shape. The sigmoid colon joins the rectum, which then connects to the anus.
The ascending and transverse sections together are called the proximal colon. The descending and sigmoid colon are called the distal colon.
Read more about : Signs a fissure is healing
Read more about : Hemorrhoid Surgery Recovery Time
Read more about : Foods that cure fissures
Read more about : Anal abscess treatment
 How do the colon and rectum work?
How do the colon and rectum work?
The colon absorbs water and salt from the remaining food matter after it goes through the small intestine (small bowel). The waste matter that's left after going through the colon goes into the rectum, the final 6 inches (15cm) of the digestive system. It's stored there until it passes through the anus. Ring-shaped muscles (also called a sphincter) around the anus keep stool from coming out until they relax during a bowel movement.
Symptoms of Colon cancer
Colon cancer often causes no symptoms in the earliest stages. However, symptoms may become more noticeable as it progresses.
These signs and symptoms may include:
. Diarrhea or constipation
. Changes in stool consistency
. Loose, narrow stools
. Blood in the stool, which may or may not be visible
. Abdominal pain, cramping, bloating, or gas
. Continual urges to defecate despite passing stools
. Weakness and fatigue
. Unexplained weight loss
. Irritable bowel syndrome
. Iron deficiency anemia
If the cancer spreads to a new location in the body, such as the liver, it can cause additional symptoms in the new area.
Causes
Doctors aren't certain what causes most colon cancers.
In general, colon cancer begins when healthy cells in the colon develop changes (mutations) in their DNA. A cell's DNA contains a set of instructions that tell a cell what to do.
Healthy cells grow and divide in an orderly way to keep your body functioning normally. But when a cell's DNA is damaged and becomes cancerous, cells continue to divide — even when new cells aren't needed. As the cells accumulate, they form a tumor.
With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body to form deposits there (metastasis).
Read more about : Sleeping position for fissure
Read more about : Foods that cure fissures
Read more about : Anal cancer symptoms
Read more about : Pancreatic cancer
Risk factors
Factors that may increase your risk of colon cancer include:
. Older age. Colon cancer can be diagnosed at any age, but a majority of people with colon cancer are older than 50. The rates of colon cancer in people younger than 50 have been increasing, but doctors aren't sure why.
. African-American race. African-Americans have a greater risk of colon cancer than do people of other races.
. A personal history of colorectal cancer or polyps. If you've already had colon cancer or noncancerous colon polyps, you have a greater risk of colon cancer in the future.
. Inflammatory intestinal conditions. Chronic inflammatory diseases of the colon, such as ulcerative colitis and Crohn's disease, can increase your risk of colon cancer.
. Inherited syndromes that increase colon cancer risk. Some gene mutations passed through generations of your family can increase your risk of colon cancer significantly. Only a small percentage of colon cancers are linked to inherited genes. The most common inherited syndromes that increase colon cancer risk are familial adenomatous polyposis (FAP) and Lynch syndrome, which is also known as hereditary nonpolyposis colorectal cancer (HNPCC).
. Family history of colon cancer. You're more likely to develop colon cancer if you have a blood relative who has had the disease. If more than one family member has colon cancer or rectal cancer, your risk is even greater.
. Low-fiber, high-fat diet. Colon cancer and rectal cancer may be associated with a typical Western diet, which is low in fiber and high in fat and calories. Research in this area has had mixed results. Some studies have found an increased risk of colon cancer in people who eat diets high in red meat and processed meat.
. A sedentary lifestyle. People who are inactive are more likely to develop colon cancer. Getting regular physical activity may reduce your risk of colon cancer.
. Diabetes. People with diabetes or insulin resistance have an increased risk of colon cancer.
. Obesity. People who are obese have an increased risk of colon cancer and an increased risk of dying of colon cancer when compared with people considered normal weight.
. Smoking. People who smoke may have an increased risk of colon cancer.
. Alcohol. Heavy use of alcohol increases your risk of colon cancer.
. Radiation therapy for cancer. Radiation therapy directed at the abdomen to treat previous cancers increases the risk of colon cancer.
Read more about : Prostate Cancer Treatments Pros and Cons
Read more about : Cancer Treatment
Read more about : Orchiectomy surgery for prostate cancer
Diagnosis
Screening for colon cancer
Doctors recommend certain screening tests for healthy people with no signs or symptoms in order to look for signs of colon cancer or noncancerous colon polyps. Finding colon cancer at its earliest stage provides the greatest chance for a cure. Screening has been shown to reduce your risk of dying of colon cancer.
Doctors generally recommend that people with an average risk of colon cancer begin screening around age 50. But people with an increased risk, such as those with a family history of colon cancer or African-American heritage, should consider screening sooner.
Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you. If a colonoscopy is used for screening, polyps can be removed during the procedure before they turn into cancer.
Diagnosing colon cancer
If your signs and symptoms indicate that you could have colon cancer, your doctor may recommend one or more tests and procedures, including:
. Using a scope to examine the inside of your colon (colonoscopy). Colonoscopy uses a long, flexible and slender tube attached to a video camera and monitor to view your entire colon and rectum. If any suspicious areas are found, your doctor can pass surgical tools through the tube to take tissue samples (biopsies) for analysis and remove polyps.
. Blood tests. No blood test can tell you if you have colon cancer. But your doctor may test your blood for clues about your overall health, such as kidney and liver function tests.
Your doctor may also test your blood for a chemical sometimes produced by colon cancers (carcinoembryonic antigen, or CEA). Tracked over time, the level of CEA in your blood may help your doctor understand your prognosis and whether your cancer is responding to treatment.
Determining the extent of the cancer
If you've been diagnosed with colon cancer, your doctor may recommend tests to determine the extent (stage) of your cancer. Staging helps determine what treatments are most appropriate for you.
Staging tests may include imaging procedures such as abdominal, pelvic and chest CT scans. In many cases, the stage of your cancer may not be fully determined until after colon cancer surgery.
The stages of colon cancer are indicated by Roman numerals that range from 0 to IV, with the lowest stages indicating cancer that is limited to the lining of the inside of the colon. By stage IV, the cancer is considered advanced and has spread (metastasized) to other areas of the body.
Prevention
Screening colon cancer
Doctors recommend that people with an average risk of colon cancer consider colon cancer screening around age 50. But people with an increased risk, such as those with a family history of colon cancer, should consider screening sooner.
Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you.
Lifestyle changes to reduce your risk of colon cancer
You can take steps to reduce your risk of colon cancer by making changes in your everyday life. Take steps to:
. Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains contain vitamins, minerals, fiber and antioxidants, which may play a role in cancer prevention. Choose a variety of fruits and vegetables so that you get an array of vitamins and nutrients.
. Drink alcohol in moderation, if at all. If you choose to drink alcohol, limit the amount of alcohol you drink to no more than one drink a day for women and two for men.
. Stop smoking. Talk to your doctor about ways to quit that may work for you.
. Exercise most days of the week. Try to get at least 30 minutes of exercise on most days. If you've been inactive, start slowly and build up gradually to 30 minutes. Also, talk to your doctor before starting any exercise program.
. Maintain a healthy weight. If you are at a healthy weight, work to maintain your weight by combining a healthy diet with daily exercise. If you need to lose weight, ask your doctor about healthy ways to achieve your goal. Aim to lose weight slowly by increasing the amount of exercise you get and reducing the number of calories you eat.
Colon cancer prevention for people with a high risk
Some medications have been found to reduce the risk of precancerous polyps or colon cancer. For instance, some evidence links a reduced risk of polyps and colon cancer to regular use of aspirin or aspirin-like drugs. But it's not clear what dose and what length of time would be needed to reduce the risk of colon cancer. Taking aspirin daily has some risks, including gastrointestinal bleeding and ulcers.
These options are generally reserved for people with a high risk of colon cancer. There isn't enough evidence to recommend these medications to people who have an average risk of colon cancer.
If you have an increased risk of colon cancer, discuss your risk factors with your doctor to determine whether preventive medications are safe for you.
During Colon Cancer Treatment
Colon Cancer Stages
There are different ways of assigning a stage to cancer. The stages indicate how far a cancer has spread and the size of any tumors.
In colon cancer, the stages develop as follows:
. Stage 0: Also known as carcinoma in situ, at this point, the cancer is in a very early stage. It has not grown farther than the inner layer of the colon and will usually be easy to treat.
. Stage 1: The cancer has grown into the next layer of tissue but has not reached the lymph nodes or any other organs.
. Stage 2: The cancer has reached the outer layers of the colon, but it has not spread beyond the colon.
. Stage 3: The cancer has grown through the outer layers of the colon, and it has reached one to three lymph nodes. It has not spread to distant sites, however.
. Stage 4: The cancer has reached other tissues beyond the wall of the colon. As stage 4 progresses, colon cancer reaches distant parts of the body.
Treatment
Which treatments are most likely to help you depends on your particular situation, including the location of your cancer, its stage and your other health concerns. Treatment for colon cancer usually involves surgery to remove the cancer. Other treatments, such as radiation therapy and chemotherapy, might also be recommended.
Surgery for early-stage colon cancer
If your colon cancer is very small, your doctor may recommend a minimally invasive approach to surgery, such as:
. Removing polyps during a colonoscopy (polypectomy). If your cancer is small, localized, completely contained within a polyp and in a very early stage, your doctor may be able to remove it completely during a colonoscopy.
. Endoscopic mucosal resection. Larger polyps might be removed during colonoscopy using special tools to remove the polyp and a small amount of the inner lining of the colon in a procedure called an endoscopic mucosal resection.
. Minimally invasive surgery (laparoscopic surgery). Polyps that can't be removed during a colonoscopy may be removed using laparoscopic surgery. In this procedure, your surgeon performs the operation through several small incisions in your abdominal wall, inserting instruments with attached cameras that display your colon on a video monitor. The surgeon may also take samples from lymph nodes in the area where the cancer is located.
Surgery for more advanced colon cancer
If the cancer has grown into or through your colon, your surgeon may recommend:
. Partial colectomy. During this procedure, the surgeon removes the part of your colon that contains the cancer, along with a margin of normal tissue on either side of the cancer. Your surgeon is often able to reconnect the healthy portions of your colon or rectum. This procedure can commonly be done by a minimally invasive approach (laparoscopy).
. Surgery to create a way for waste to leave your body. When it's not possible to reconnect the healthy portions of your colon or rectum, you may need an ostomy. This involves creating an opening in the wall of your abdomen from a portion of the remaining bowel for the elimination of stool into a bag that fits securely over the opening.
Sometimes the ostomy is only temporary, allowing your colon or rectum time to heal after surgery. In some cases, however, the colostomy may be permanent.
. Lymph node removal. Nearby lymph nodes are usually also removed during colon cancer surgery and tested for cancer.
Surgery for advanced cancer
If your cancer is very advanced or your overall health very poor, your surgeon may recommend an operation to relieve a blockage of your colon or other conditions in order to improve your symptoms. This surgery isn't done to cure cancer, but instead to relieve signs and symptoms, such as a blockage, bleeding or pain.
In specific cases where the cancer has spread only to the liver or lung but your overall health is otherwise good, your doctor may recommend surgery or other localized treatments to remove the cancer. Chemotherapy may be used before or after this type of procedure. This approach provides a chance to be free of cancer over the long term.
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells. Chemotherapy for colon cancer is usually given after surgery if the cancer is larger or has spread to the lymph nodes. In this way, chemotherapy may kill any cancer cells that remain in the body and help reduce the risk of cancer recurrence.
Chemotherapy might also be used before an operation to shrink a large cancer so that it's easier to remove with surgery.
Chemotherapy can also be used to relieve symptoms of colon cancer that can't be removed with surgery or that has spread to other areas of the body. Sometimes it's combined with radiation therapy.
Radiation therapy
Radiation therapy uses powerful energy sources, such as X-rays and protons, to kill cancer cells. It might be used to shrink a large cancer before an operation so that it can be removed more easily.
When surgery isn't an option, radiation therapy might be used to relieve symptoms, such as pain. Sometimes radiation is combined with chemotherapy.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Targeted drugs are usually combined with chemotherapy. Targeted drugs are typically reserved for people with advanced colon cancer.
Immunotherapy
Immunotherapy is a drug treatment that uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that blind the immune system cells from recognizing the cancer cells. Immunotherapy works by interfering with that process.
Immunotherapy is usually reserved for advanced colon cancer. Your doctor might have your cancer cells tested to see if they're likely to respond to this treatment.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care is provided by a team of doctors, nurses and other specially trained professionals that work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care.
Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Read more about : prostate biopsy anesthesia
Read more about : Bladder cancer symptoms in Men and women
Read more about : What should not eat in fissure?
Read more about : Genaral surgery
After Colon Cancer Treatment
Living as a Colon Cancer Survivor
For many people with colon cancer, treatment can remove or destroy the cancer. The end of treatment can be both stressful and exciting. You may be relieved to finish treatment, but find it hard not to worry about cancer coming back. This is very common if you’ve had cancer.
For other people, colorectal cancer may never go away completely. Some people may get regular treatment with chemotherapy, radiation therapy, or other treatments to try to control the cancer for as long as possible. Learning to live with cancer that does not go away can be difficult and very stressful.
Ask your doctor for a survivorship care plan
Talk with your doctor about developing a survivorship care plan for you. This plan might include:
. A suggested schedule for follow-up exams and tests
. A list of possible late- or long-term side effects from your treatment, including what to watch for and when you should contact your doctor
. A schedule for other tests you might need in the future, such as early detection (screening) tests for other types of cancer
. Suggestions for things you can do that might improve your health, including possibly lowering your chances of the cancer coming back, such as diet and physical activity changes
. Reminders to keep your appointments with your primary care provider (PCP) who will monitor your general health care, including your cancer screening tests.
What’s the survival rate for people with colon cancer?
Having a colon cancer diagnosis can be worrying, but this type of cancer is extremely treatable, especially when caught early.
The 5-year survival rate for all stages of colon cancer is estimated to be 63 percent based on data from 2009 to 2015. For rectal cancer, the 5-year survival rate is 67 percent.
The 5-year survival rate reflects the percentage of people who survived at least 5 years after diagnosis.
Treatment measures have also come a long way for more advanced cases of colon cancer.
According to the University of Texas Southwestern Medical Center, in 2015, the average survival time for stage 4 colon cancer was around 30 months. In the 1990s, the average was 6 to 8 months.
At the same time, doctors are now seeing colorectal cancer in younger people. Some of this may be due to unhealthy lifestyle choices.
According to the ACS, while colon cancer deaths declined in older adults, deaths in people younger than 50 years old increased between 2008 and 2017.
Managing long-term side effects
Most side effects go away after treatment ends, but some may continue and need special care to manage. For example, if you have a colostomy or ileostomy, you may worry about doing everyday activities. Whether your ostomy is temporary or permanent, a health care professional trained to help people with colostomies and ileostomies (called an enterostomal therapist) can teach you how to care for it.
Some people with colon cancer may have long lasting trouble with chronic diarrhea, going to the bathroom frequently, or not being able to hold their stool. Some may also have problems with numbness or tingling in their fingers and toes (peripheral neuropathy) from chemo they received.
If the cancer comes back
If the cancer does recur at some point, your treatment options will depend on where the cancer is, what treatments you’ve had before, and your overall health.
Could I get a second cancer after colon cancer treatment?
People who’ve had colon cancer can still get other cancers, In fact, colon cancer survivors are at higher risk for getting another colon cancer, as well as some other types of cancer.


