Rectal Cancer Treatment
 What is Rectal Cancer?
What is Rectal Cancer?
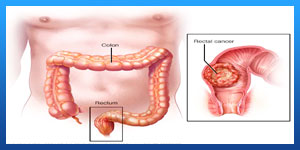
Rectal cancer is a cancer that begins in the rectum. The rectum is the last several inches of the large intestine. It starts at the end of the final segment of your colon and ends when it reaches the short, narrow passage leading to the anus.
Cancer inside the rectum (rectal cancer) and cancer inside the colon (colon cancer) are often referred to together as "colorectal cancer."
While rectal and colon cancers are similar in many ways, their treatments are quite different. This is mainly because the rectum sits in a tight space, barely separated from other organs and structures. The tight space can make surgery to remove rectal cancer complex.
In the past, long-term survival was uncommon for people with rectal cancer, even after extensive treatment. Thanks to treatment advances over the last few decades, rectal cancer survival rates have greatly improved.
Read more about : Esophageal cancer treatment
Read more about : Metastatic myxofibrosarcoma treatment with the best Iranian oncologist surgeon
Before Rectal Cancer Treatment
Signs and Symptoms of Rectal Cancer
Some symptoms of rectal cancer could be due to other conditions. These symptoms include:
. Weakness and fatigue
. Appetite changes
. Weight loss
. Frequent abdominal discomfort, gas, cramps, pain
Other signs and symptoms of rectal cancer include:
. Changes in how often you have bowel movements
. Feeling that your bowel isn’t emptying completely
. Pain when you have a bowel movement
. Diarrhea or constipation
. Dark maroon or bright red blood in stool narrow stool
. Iron deficiency anemia
Read more about : Signs a fissure is healing

When to see a doctor
Make an appointment with your doctor if you have any persistent symptoms that worry you.
Causes
Rectal cancer begins when healthy cells in the rectum develop changes (mutations) in their DNA. A cell's DNA contains the instructions that tell a cell what to do.
The changes tell the cells to grow uncontrollably and to continue living after healthy cells would die. The accumulating cells can form a tumor. With time, the cancer cells can grow to invade and destroy healthy tissue nearby. And cancerous cells can break away and travel (metastasize) to other parts of the body.
For most rectal cancers, it's not clear what causes the mutations that cause the cancer to form.
Inherited gene mutations that increase the risk of colon and rectal cancer
In some families, gene mutations passed from parents to children increase the risk of colorectal cancer. These mutations are involved in only a small percentage of rectal cancers. Some genes linked to colorectal cancer increase the risk of developing the disease, but they don't make it inevitable.
Two well-defined genetic colorectal cancer syndromes are:
. Lynch syndrome. Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), increases the risk of colon cancer and other cancers. People with Lynch syndrome tend to develop colon cancer before age 50.
. Familial adenomatous polyposis (FAP). FAP is a rare disorder that causes thousands of polyps in the lining of your colon and rectum. People with untreated FAP have a significantly increased risk of developing colon or rectal cancer before age 40.
Genetic testing can detect these and other, rarer inherited colorectal cancer syndromes. If you're concerned about your family history of colon cancer, talk to your doctor about whether your family history suggests you have a risk of these conditions.
Risk factors
Factors that may increase the risk of rectal cancer are the same as those that increase the risk of colon cancer. Colorectal cancer risk factors include:
. Older age. Colorectal cancer can be diagnosed at any age, but most people with this type of cancer are older than 50. The rates of colorectal cancer in people younger than 50 have been increasing, but doctors aren't sure why.
. African-American descent. People of African ancestry born in the United States have a greater risk of colorectal cancer than do people of European ancestry.
. A personal history of colorectal cancer or polyps. Your risk of colorectal cancer is higher if you've already had rectal cancer, colon cancer or adenomatous polyps.
. Inflammatory bowel disease. Chronic inflammatory diseases of the colon and rectum, such as ulcerative colitis and Crohn's disease, increase your risk of colorectal cancer.
. Inherited syndromes that increase rectal cancer risk. Genetic syndromes passed through generations of your family can increase your risk of colon and rectal cancer, including FAP and Lynch syndrome.
. Family history of colorectal cancer. You're more likely to develop colorectal cancer if you have a parent, sibling or child with colon or rectal cancer.
. Eating a diet low in vegetables. Colorectal cancer may be associated with a diet low in vegetables and high in red meat, particularly when the meat is charred or well done.
. Too little exercise. If you're inactive, you're more likely to develop colorectal cancer. Getting regular physical activity may reduce your risk of cancer.
. Diabetes. People with poorly controlled type 2 diabetes may have an increased risk of colorectal cancer.
. Obesity. Obese people have an increased risk of colorectal cancer when compared with people considered at a healthy weight.
. Smoking. People who smoke may have an increased risk of colorectal cancer.
. Drinking alcohol. Regularly drinking more than three alcoholic beverages a week may increase your risk of colorectal cancer.
. Radiation therapy for previous cancer. Radiation therapy directed at the abdomen to treat previous cancers may increase the risk of colorectal cancer.
Read more about : Anal abscess treatment
Prevention
To reduce your risk of colorectal cancer, consider trying to:
. Talk to your doctor about cancer screening. Colorectal cancer screening reduces the risk of cancer by identifying precancerous polyps in the colon and rectum that could develop into cancer. Ask your doctor when you should begin screening. Most medical organizations recommend starting screening around age 50, or earlier if you have risk factors for colorectal cancer.
Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you.
. Exercise most days of the week. Try to get at least 30 minutes of exercise on most days. If you've been inactive, start slowly and build up gradually to 30 minutes. Also, talk to your doctor before beginning any exercise program.
. Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains contain vitamins, minerals, fiber and antioxidants, which may play a role in cancer prevention. Choose a variety of fruits and vegetables so that you get an array of vitamins and nutrients.
. Maintain a healthy weight. If you're at a healthy weight, maintain it by exercising regularly and choosing a healthy diet. If you're overweight, work to lose weight slowly by increasing exercise and reducing the number of calories you eat.
. Stop smoking. If you smoke, stop. If you're having trouble quitting, talk to your doctor about options. Medications and counseling may help.
. Drink alcohol in moderation, if at all. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.

Diagnosis
Tests to diagnose rectal cancer
Rectal cancer can be found during a screening test for colorectal cancer. Or it may be suspected based on your symptoms. Tests and procedures used to confirm the diagnosis include:
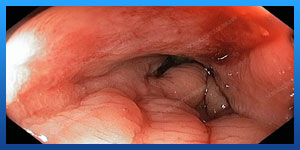
. Using a scope to examine the inside of your colon and rectum (colonoscopy). Colonoscopy uses a long, flexible tube (colonoscope) attached to a video camera and monitor to view your colon and rectum. If cancer is found in your rectum, your doctor may recommend examining your colon in order to look for additional suspicious areas.
. Removing a sample of tissue for testing (biopsy). If any suspicious areas are found, your doctor can pass surgical tools through the colonoscope to take tissue samples (biopsies) for analysis and remove polyps.
The tissue sample is sent to a lab to be examined by doctors who specialize in analyzing blood and body tissues (pathologists). Tests can determine whether the cells are cancer, whether they're aggressive and which genes in the cancer cells are abnormal. Your doctor uses this information to understand your prognosis and determine your treatment options.
Tests to look for rectal cancer spread
Once you're diagnosed with rectal cancer, the next step is to determine the cancer's extent (stage). The stage of your cancer helps determine your prognosis and your treatment options.
Read more about : Cancer treatment in Iran
Staging tests include:
. Complete blood count (CBC). This test reports the numbers of different types of cells in your blood. A CBC shows whether your red blood cell count is low (anemia), which suggests that a tumor is causing blood loss. A high level of white blood cells is a sign of infection, which is a risk if a rectal tumor grows through the wall of the rectum.
. Blood tests to measure organ function. A chemistry panel is a blood test to measures levels of different chemicals in the blood. Abnormal levels of some of these chemicals may suggest that cancer has spread to the liver. High levels of other chemicals may indicate problems with other organs, such as the kidneys.
. Carcinoembryonic antigen (CEA). Cancers sometimes produce substances called tumor markers that can be detected in blood. One such marker, carcinoembryonic antigen (CEA), may be higher than usual in people with colorectal cancer. CEA testing is particularly useful in monitoring your response to treatment.
. CT scan of the chest. This imaging test helps determine whether rectal cancer has spread to other organs, such as the liver and lungs.
. MRI of the pelvis. An MRI provides a detailed image of the muscles, organs and other tissues surrounding a tumor in the rectum. An MRI also shows the lymph nodes near the rectum and different layers of tissue in the rectal wall.
Your doctor uses information from these tests to assign your cancer a stage. The stages of rectal cancer are indicated by Roman numerals that range from 0 to IV. The lowest stage indicates cancer that is limited to the lining of the inside of the rectum. By stage IV, the cancer is considered advanced and has spread (metastasized) to other areas of the body.
During Rectal Cancer Treatment
Types of rectal cancer
Most people who are diagnosed with rectal cancer have a type called adenocarcinoma. There are other rarer tumor types too. These other types of rectal cancer may be treated differently than adenocarcinoma.
. Adenocarcinoma
The vast majority of rectal cancer is adenocarcinoma. This is a cancer of the cells that line the inside surface of the rectum.
. Carcinoid Tumors
Carcinoid tumors start in hormone-producing cells in the intestines.
. Gastrointestinal Stromal Tumors
Gastrointestinal stromal tumors can be a type of soft tissue sarcoma that can be found anywhere in the gastrointestinal tract but is rare in the rectum. These tumors can also be other types of sarcoma that start in the blood vessels or connective tissue of the colon.
. Lymphoma
Lymphoma is a cancer of the immune system. It more commonly starts in the lymph nodes but can start in the rectum.
Rectal Cancer Stages
No matter where it starts, cancer can spread, or metastasize, through tissue, the lymph system, or the bloodstream to reach other parts of the body.
Staging cancer indicates how far the cancer has progressed, which can help your doctor decide the best treatment.
 The following stages are used for rectal cancer:
The following stages are used for rectal cancer:
Stage 0 (Carcinoma in Situ)
In stage 0 rectal cancer, abnormal cells are found in the mucosa (innermost layer) of the rectum wall. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ.
Stage I
In stage I rectal cancer, cancer has formed in the mucosa (innermost layer) of the rectum wall and has spread to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the rectum wall.
Stage II
Stage II rectal cancer is divided into stages IIA, IIB, and IIC.
. Stage IIA: Cancer has spread through the muscle layer of the rectum wall to the serosa (outermost layer) of the rectum wall.
. Stage IIB: Cancer has spread through the serosa (outermost layer) of the rectum wall to the tissue that lines the organs in the abdomen (visceral peritoneum).
. Stage IIC: Cancer has spread through the serosa (outermost layer) of the rectum wall to nearby organs.
Stage III
Stage III rectal cancer is divided into stages IIIA, IIIB, and IIIC.
In stage IIIA, cancer has spread:
. Through the mucosa (innermost layer) of the rectum wall to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the rectum wall. Cancer has spread to one to three nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes; or
. Through the mucosa (innermost layer) of the rectum wall to the submucosa (layer of tissue next to the mucosa). Cancer has spread to four to six nearby lymph nodes.
In stage IIIB, cancer has spread:
. Through the muscle layer of the rectum wall to the serosa (outermost layer) of the rectum wall or has spread through the serosa to the tissue that lines the organs in the abdomen (visceral peritoneum). Cancer has spread to one to three nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes; or
. To the muscle layer or to the serosa (outermost layer) of the rectum wall. Cancer has spread to four to six nearby lymph nodes; or
. Through the mucosa (innermost layer) of the rectum wall to the submucosa (layer of tissue next to the mucosa) or to the muscle layer of the rectum wall. Cancer has spread to seven or more nearby lymph nodes.
In stage IIIC, cancer has spread:
. Through the serosa (outermost layer) of the rectum wall to the tissue that lines the organs in the abdomen (visceral peritoneum). Cancer has spread to four to six nearby lymph nodes; or
. Through the muscle layer of the rectum wall to the serosa (outermost layer) of the rectum wall or has spread through the serosa to the tissue that lines the organs in the abdomen (visceral peritoneum). Cancer has spread to seven or more nearby lymph nodes; or
. Through the serosa (outermost layer) of the rectum wall to nearby organs. Cancer has spread to one or more nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes.
Stage IV
Stage IV rectal cancer is divided into stages IVA, IVB, and IVC.
. Stage IVA: Cancer has spread to one area or organ that is not near the rectum, such as the liver, lung, ovary, or a distant lymph node.
. Stage IVB: Cancer has spread to more than one area or organ that is not near the rectum, such as the liver, lung, ovary, or a distant lymph node.
. Stage IVC: Cancer has spread to the tissue that lines the wall of the abdomen and may have spread to other areas or organs.
Treatment
Rectal cancer treatment often involves a combination of therapies. When possible, surgery is used to cut away the cancer cells. Other treatments, such as chemotherapy and radiation therapy, may be used after surgery to kill any cancer cells that remain and reduce the risk that cancer will return.
If surgeons are concerned that the cancer can't be removed completely without hurting nearby organs and structures, your doctor may recommend a combination of chemotherapy and radiation therapy as your initial treatment. These combined treatments may shrink the cancer and make it easier to remove during an operation.
Surgery
Rectal cancer is often treated with surgery to remove the cancer cells. Which operation is best for you depends on your particular situation, such as the location and stage of your cancer, how aggressive the cancer cells are, your overall health, and your preferences.
Operations used to treat rectal cancer include:
. Removing very small cancers from the inside of the rectum. Very small rectal cancers may be removed using a colonoscope or another specialized type of scope inserted through the anus (transanal local excision). Surgical tools can be passed through the scope to cut away the cancer and some of the healthy tissue around it.
This procedure might be an option if your cancer is small and unlikely to spread to nearby lymph nodes. If a lab analysis finds that your cancer cells are aggressive or more likely to spread to the lymph nodes, your doctor may recommend additional surgery.
. Removing all or part of the rectum. Larger rectal cancers that are far enough away from the anal canal might be removed in a procedure (low anterior resection) that removes all or part of the rectum. Nearby tissue and lymph nodes are also removed. This procedure preserves the anus so that waste can leave the body normally.
How the procedure is performed depends on the cancer's location. If cancer affects the upper portion of the rectum, that part of the rectum is removed and then the colon is attached to the remaining rectum (colorectal anastomosis). All of the rectum may be removed if the cancer is located in the lower portion of the rectum. Then the colon is shaped into a pouch and attached to the anus (coloanal anastomosis).
. Removing the rectum and anus. For rectal cancers that are located near the anus, it might not be possible to remove the cancer completely without damaging the muscles that control bowel movements. In these situations, surgeons may recommend an operation called abdominoperineal resection (APR) to remove the rectum, anus and some of the colon, as well as nearby tissue and lymph nodes.
The surgeon creates an opening in the abdomen and attaches the remaining colon (colostomy). Waste leaves your body through the opening and collects in a bag that attaches to your abdomen.
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells. For rectal cancer, chemotherapy might be recommended after surgery to kill any cancer cells that might remain.
Chemotherapy combined with radiation therapy might also be used before an operation to shrink a large cancer so that it's easier to remove with surgery.
Chemotherapy can also be used to relieve symptoms of rectal cancer that can't be removed with surgery or that has spread to other areas of the body.
Radiation therapy
Radiation therapy uses powerful energy sources, such as X-rays and protons, to kill cancer cells. In people with rectal cancer, radiation therapy is often combined with chemotherapy that makes the cancer cells more likely to be damaged by the radiation. It can be used after surgery to kill any cancer cells that might remain. Or it can be used before surgery to shrink a cancer and make it easier to remove.
When surgery isn't an option, radiation therapy might be used to relieve symptoms, such as pain.
Combined chemotherapy and radiation therapy
Combining chemotherapy and radiation therapy (chemoradiotherapy) makes cancer cells more vulnerable to radiation. The combination is often used for larger rectal cancers and those that have a higher risk of returning after surgery.
Chemoradiotherapy may be recommended:
. Before surgery. Chemoradiotherapy may help shrink the cancer enough to make a less invasive surgery possible. The combined treatment may increase the chance that your operation will leave the anal area intact so waste can leave the body normally after surgery.
. After surgery. If surgery was your first treatment, your doctor may recommend chemoradiotherapy afterward if there's an increased risk that your cancer may return.
. As the primary treatment. Your doctor may recommend chemoradiotherapy to control the growth of cancer if your rectal cancer is advanced or if surgery isn't an option.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Targeted drugs are usually combined with chemotherapy. Targeted drugs are typically reserved for people with advanced rectal cancer.
Immunotherapy
Immunotherapy is a drug treatment that uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy is usually reserved for advanced rectal cancer.
Supportive (palliative) care
Palliative care is focused on providing relief from pain and other symptoms of a severe illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
After Rectal Cancer Treatment
When you wake up after surgery, you will have some pain and will need pain medicines for a few days. For the first couple of days, you may not be able to eat or you may be allowed limited liquids, as the rectum needs some time to recover. Most people are able to eat solid food again in a few days.
Rarely, the new connections between the ends of the colon may not hold together and may leak. This can quickly cause severe belly pain, fever, and the belly to feel very hard. A smaller leak may cause you to not pass stool, have no desire to eat, and not do well or recover after surgery. A leak can lead to infection, and more surgery may be needed to fix it. It’s also possible that the incision (cut) in the abdomen (belly) might open up, becoming an open wound that may need special care as it heals.
After the surgery, you might develop scar tissue in your abdomen (belly) that can cause organs or tissues to stick together. These are called adhesions. Normally your intestines freely slide around inside your belly. In rare cases, adhesions can cause the bowels to twist up and can even block the bowel. This causes pain and swelling in the belly that's often worse after eating. Further surgery may be needed to remove the scar tissue.
Sources:
https://www.cancer.org/cancer/colon-rectal-cancer/treating/by-stage-rectum.
https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/rectal-cancer
https://www.hopkinsmedicine.org/health/conditions-and-diseases/colon-cancer/rectal-cancer-treatment

