Parkinson’s disease Treatment
What is Parkinson’s disease?
Parkinson’s disease is a progressive nervous system disorder that affects movement. Symptoms start gradually, sometimes starting with a barely noticeable tremor in just one hand. Tremors are common, but the disorder also commonly causes stiffness or slowing of movement.
In the early stages of Parkinson’s disease, your face may show little or no expression. Your arms may not swing when you walk. Your speech may become soft or slurred. Parkinson’s disease symptoms worsen as your condition progresses over time.
Although Parkinson’s disease can’t be cured, medications might significantly improve your symptoms. Occasionally, your doctor may suggest surgery to regulate certain regions of your brain and improve your symptoms.
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best neurologists and neurosurgeons in Iran. The price of a Deep Brain Stimulation (DBS) surgery in Iran can vary according to each individual’s case and will be determined based on photos and an in-person assessment with the doctor.
For more information about the cost of Deep Brain Stimulation (DBS) surgery in Iran and to schedule an appointment in advance, you can contact Iranian Surgery consultants via WhatsApp number 0098 901 929 0946. This service is completely free.

Before Parkinson’s disease
Symptoms
Parkinson’s disease signs and symptoms can be different for everyone. Early signs may be mild and go unnoticed. Symptoms often begin on one side of your body and usually remain worse on that side, even after symptoms begin to affect both sides.
Parkinson’s signs and symptoms may include:
. Tremor. A tremor, or shaking, usually begins in a limb, often your hand or fingers. You may rub your thumb and forefinger back and forth, known as a pill-rolling tremor. Your hand may tremble when it’s at rest.
. Slowed movement (bradykinesia). Over time, Parkinson’s disease may slow your movement, making simple tasks difficult and time-consuming. Your steps may become shorter when you walk. It may be difficult to get out of a chair. You may drag your feet as you try to walk.
. Rigid muscles. Muscle stiffness may occur in any part of your body. The stiff muscles can be painful and limit your range of motion.
Impaired posture and balance. Your posture may become stooped, or you may have balance problems as a result of Parkinson’s disease.
. Loss of automatic movements. You may have a decreased ability to perform unconscious movements, including blinking, smiling or swinging your arms when you walk.
. Speech changes. You may speak softly, quickly, slur or hesitate before talking. Your speech may be more of a monotone rather than have the usual inflections.
Writing changes. It may become hard to write, and your writing may appear small.
When to see a doctor
See your doctor if you have any of the symptoms associated with Parkinson’s disease — not only to diagnose your condition but also to rule out other causes for your symptoms.
Causes
In Parkinson’s disease, certain nerve cells (neurons) in the brain gradually break down or die. Many of the symptoms are due to a loss of neurons that produce a chemical messenger in your brain called dopamine. When dopamine levels decrease, it causes abnormal brain activity, leading to impaired movement and other symptoms of Parkinson’s disease.
The cause of Parkinson’s disease is unknown, but several factors appear to play a role, including:
. Genes. Researchers have identified specific genetic mutations that can cause Parkinson’s disease. But these are uncommon except in rare cases with many family members affected by Parkinson’s disease.
However, certain gene variations appear to increase the risk of Parkinson’s disease but with a relatively small risk of Parkinson’s disease for each of these genetic markers.
. Environmental triggers. Exposure to certain toxins or environmental factors may increase the risk of later Parkinson’s disease, but the risk is relatively small.
Researchers have also noted that many changes occur in the brains of people with Parkinson’s disease, although it’s not clear why these changes occur. These changes include:
. The presence of Lewy bodies. Clumps of specific substances within brain cells are microscopic markers of Parkinson’s disease. These are called Lewy bodies, and researchers believe these Lewy bodies hold an important clue to the cause of Parkinson’s disease.
. Alpha-synuclein found within Lewy bodies. Although many substances are found within Lewy bodies, scientists believe an important one is the natural and widespread protein called alpha-synuclein (a-synuclein). It’s found in all Lewy bodies in a clumped form that cells can’t break down. This is currently an important focus among Parkinson’s disease researchers.
Risk factors
Risk factors for Parkinson’s disease include:
. Age. Young adults rarely experience Parkinson’s disease. It ordinarily begins in middle or late life, and the risk increases with age. People usually develop the disease around age 60 or older.
. Heredity. Having a close relative with Parkinson’s disease increases the chances that you’ll develop the disease. However, your risks are still small unless you have many relatives in your family with Parkinson’s disease.
. Sex. Men are more likely to develop Parkinson’s disease than are women.
. Exposure to toxins. Ongoing exposure to herbicides and pesticides may slightly increase your risk of Parkinson’s disease.
Read more about : Deep Brain Stimulation for Parkinson’s disease
Complications
Parkinson’s disease is often accompanied by these additional problems, which may be treatable:
. Thinking difficulties. You may experience cognitive problems (dementia) and thinking difficulties. These usually occur in the later stages of Parkinson’s disease. Such cognitive problems aren’t very responsive to medications.
. Depression and emotional changes. You may experience depression, sometimes in the very early stages. Receiving treatment for depression can make it easier to handle the other challenges of Parkinson’s disease.
You may also experience other emotional changes, such as fear, anxiety or loss of motivation. Doctors may give you medications to treat these symptoms.
. Swallowing problems. You may develop difficulties with swallowing as your condition progresses. Saliva may accumulate in your mouth due to slowed swallowing, leading to drooling.
. Chewing and eating problems. Late-stage Parkinson’s disease affects the muscles in your mouth, making chewing difficult. This can lead to choking and poor nutrition.
. Sleep problems and sleep disorders. People with Parkinson’s disease often have sleep problems, including waking up frequently throughout the night, waking up early or falling asleep during the day.
People may also experience rapid eye movement sleep behavior disorder, which involves acting out your dreams. Medications may help your sleep problems.
. Bladder problems. Parkinson’s disease may cause bladder problems, including being unable to control urine or having difficulty urinating.
. Constipation. Many people with Parkinson’s disease develop constipation, mainly due to a slower digestive tract.
You may also experience:
. Blood pressure changes. You may feel dizzy or lightheaded when you stand due to a sudden drop in blood pressure (orthostatic hypotension).
. Smell dysfunction. You may experience problems with your sense of smell. You may have difficulty identifying certain odors or the difference between odors.
. Fatigue. Many people with Parkinson’s disease lose energy and experience fatigue, especially later in the day. The cause isn’t always known.
. Pain. Some people with Parkinson’s disease experience pain, either in specific areas of their bodies or throughout their bodies.
. Sexual dysfunction. Some people with Parkinson’s disease notice a decrease in sexual desire or performance.
Read more about Herniated Disk Treatment
Diagnosis
No specific test exists to diagnose Parkinson’s disease. Your doctor trained in nervous system conditions (neurologist) will diagnose Parkinson’s disease based on your medical history, a review of your signs and symptoms, and a neurological and physical examination.
Your doctor may suggest a specific single-photon emission computerized tomography (SPECT) scan called a dopamine transporter scan (DaTscan). Although this can help support the suspicion that you have Parkinson’s disease, it is your symptoms and neurologic examination that ultimately determine the correct diagnosis. Most people do not require a DaTscan.
Your doctor may order lab tests, such as blood tests, to rule out other conditions that may be causing your symptoms.
Imaging tests — such as an MRI, ultrasound of the brain, and PET scans — also may be used to help rule out other disorders. Imaging tests aren’t particularly helpful for diagnosing Parkinson’s disease.
In addition to your examination, your doctor may give you carbidopa-levodopa (Rytary, Sinemet, others), a Parkinson’s disease medication. You must be given a sufficient dose to show the benefit, as low doses for a day or two aren’t reliable. Significant improvement with this medication will often confirm your diagnosis of Parkinson’s disease.
Sometimes it takes time to diagnose Parkinson’s disease. Doctors may recommend regular follow-up appointments with neurologists trained in movement disorders to evaluate your condition and symptoms over time and diagnose Parkinson’s disease.
Prevention
Because the cause of Parkinson’s is unknown, proven ways to prevent the disease also remain a mystery.
Some research has shown that regular aerobic exercise might reduce the risk of Parkinson’s disease.
Some other research has shown that people who consume caffeine — which is found in coffee, tea and cola — get Parkinson’s disease less often than those who don’t drink it. Green tea is also related to a reduced risk of developing Parkinson’s disease. However, it is still not known whether caffeine actually protects against getting Parkinson’s, or is related in some other way. Currently there is not enough evidence to suggest drinking caffeinated beverages to protect against Parkinson’s.
Risks and Complications of deep brain stimulation (DBS)
Although deep brain stimulation is minimally invasive and considered safe, any type of surgery has the risk of complications. Also, the brain stimulation itself can cause side effects.
Complications of DBS fall into three categories: surgery complications, hardware (device and wires) complications, and stimulation-related complications.
. Surgery risks
Deep brain stimulation involves creating small holes in the skull to implant the electrodes, and surgery to implant the device that contains the batteries under the skin in the chest. Complications of surgery may include:
. Misplacement of lead
. Bleeding in the brain
. Stroke
. Infection
. Breathing problems
. Nausea
. Heart problems
. Seizure
. Possible side effects after surgery
Side effects associated with deep brain stimulation may include:
. Seizure
. Infection
. Headache
. Confusion
. Difficulty concentrating
. Stroke
. Temporary pain and swelling at the implantation site
A few weeks after the surgery, the device will be turned on and the process of finding the best settings for you begins. Some settings may cause side effects, but these often improve with further adjustments of your device.
Because there have been infrequent reports that the DBS therapy affects the movements needed for swimming, the Food and Drug Administration recommends consulting with your doctor and taking water safety precautions before swimming.
Read more about : What is Deep Brain Stimulation Used for?
. Possible side effects of stimulation
. Numbness or tingling sensations
. Muscle tightness of the face or arm
. Speech problems
. Balance problems
. Lightheadedness
. Vision problems, such as double vision
. Unwanted mood changes, such as anger and depression
. Hardware complications
Hardware complications include movement of the leads, lead failure, failure of any part of the DBS system, pain over the pulse generator device, battery failure, infection around the device and the device breaking through the skin as the thickness of skin and fat layer change as one ages.
During Parkinson’s disease
Stages of Parkinson’s disease
What are the stages of Parkinson’s?
Parkinson’s disease is broken into five stages. Each stage presents changing or new symptoms that a person is likely to encounter.
Dividing the disease into stages helps doctors and caregivers understand and address some of the challenges a person is experiencing as the disease progresses.
Stage 1
During the initial stages of Parkinson’s disease, the symptoms are typically not severe. A person can perform everyday tasks with minimal issues, so many of the signs and symptoms of stage 1 can be missed.
Some signs and symptoms of this stage include changes in:
. Posture
. Facial expressions
. Walking
In addition, a person may experience mild tremors on one side of the body. A doctor might prescribe medication at this stage that will help control the symptoms.
Stage 2
Tremors, trembling, and stiffness affect both sides of the body in stage 2 of the disease and are much more noticeable.
The increased stiffness is often enough to delay tasks. A person may find it difficult to maintain independent living, according to their age and other factors.
Walking, speech, and posture problems are often more noticeable in stage 2 of Parkinson’s.
Stage 3
Stage 3 or mid-stage Parkinson’s disease is characterized by an increase in symptoms. A person will experience most or all of the symptoms of stage 2, plus:
. Problems with balance
. Slow movements
. Slow reflexes
A person with stage 3 Parkinson’s must be aware of the increased likelihood of falling due to coordination issues. Dressing and other self-care tasks may become more difficult.
Treatment at this stage often involves both medication and occupational or physical therapy. Some people respond favorably to treatment, while others may not experience much improvement.
Stage 4
During stage 4 Parkinson’s, daily activities may be challenging or even impossible. It is likely that a person will require some form of daily care, as independent living is not usually possible.
People at this stage may be able to stand on their own but may need a walker or other assistive device to walk.
Stage 5
Stage 5 is the last and most debilitating stage of Parkinson’s disease. A person will not be able to stand or move around due to stiffness. Depending on their age and health, they may be bedridden or use a wheelchair for mobility.
Unlike earlier stages, a person will need constant nursing aides. Aides will help the person do daily activities and prevent dangerous situations or accidents from occurring.
In stage 5, a person may also experience:
. Hallucinations
. Delusions
. Dementia
. Poor response to medication
. Confusion
Treatment
Parkinson’s disease can’t be cured, but medications can help control your symptoms, often dramatically. In some more advanced cases, surgery may be advised.
Your doctor may also recommend lifestyle changes, especially ongoing aerobic exercise. In some cases, physical therapy that focuses on balance and stretching also is important. A speech-language pathologist may help improve your speech problems.
Medications
Medications may help you manage problems with walking, movement and tremor. These medications increase or substitute for dopamine.
People with Parkinson’s disease have low brain dopamine concentrations. However, dopamine can’t be given directly, as it can’t enter your brain.
You may have significant improvement of your symptoms after beginning Parkinson’s disease treatment. Over time, however, the benefits of drugs frequently diminish or become less consistent. You can usually still control your symptoms fairly well.
Medications your doctor may prescribe include:
. Carbidopa-levodopa. Levodopa, the most effective Parkinson’s disease medication, is a natural chemical that passes into your brain and is converted to dopamine.
Levodopa is combined with carbidopa (Lodosyn), which protects levodopa from early conversion to dopamine outside your brain. This prevents or lessens side effects such as nausea.
Side effects may include nausea or lightheadedness (orthostatic hypotension).
After years, as your disease progresses, the benefit from levodopa may become less stable, with a tendency to wax and wane (“wearing off”).
Also, you may experience involuntary movements (dyskinesia) after taking higher doses of levodopa. Your doctor may lessen your dose or adjust the times of your doses to control these effects.
. Inhaled carbidopa-levodopa. Inbrija is a new brand-name drug delivering carbidopa-levodopa in an inhaled form. It may be helpful in managing symptoms that arise when oral medications suddenly stop working during the day.
. Carbidopa-levodopa infusion. Duopa is a brand-name medication made up of carbidopa and levodopa. However, it’s administered through a feeding tube that delivers the medication in a gel form directly to the small intestine.
Duopa is for patients with more-advanced Parkinson’s who still respond to carbidopa-levodopa, but who have a lot of fluctuations in their response. Because Duopa is continually infused, blood levels of the two drugs remain constant.
Placement of the tube requires a small surgical procedure. Risks associated with having the tube include the tube falling out or infections at the infusion site.
. Dopamine agonists. Unlike levodopa, dopamine agonists don’t change into dopamine. Instead, they mimic dopamine effects in your brain.
They aren’t as effective as levodopa in treating your symptoms. However, they last longer and may be used with levodopa to smooth the sometimes off-and-on effect of levodopa.
Dopamine agonists include pramipexole (Mirapex), ropinirole (Requip) and rotigotine (Neupro, given as a patch). Apomorphine (Apokyn) is a short-acting injectable dopamine agonist used for quick relief.
Some of the side effects of dopamine agonists are similar to the side effects of carbidopa-levodopa. But they can also include hallucinations, sleepiness and compulsive behaviors such as hypersexuality, gambling and eating. If you’re taking these medications and you behave in a way that’s out of character for you, talk to your doctor.
. MAO B inhibitors. These medications include selegiline (Zelapar), rasagiline (Azilect) and safinamide (Xadago). They help prevent the breakdown of brain dopamine by inhibiting the brain enzyme monoamine oxidase B (MAO B). This enzyme metabolizes brain dopamine. Selegiline given with levodopa may help prevent wearing-off.
Side effects of MAO B inhibitors may include headaches, nausea or insomnia. When added to carbidopa-levodopa, these medications increase the risk of hallucinations.
These medications are not often used in combination with most antidepressants or certain narcotics due to potentially serious but rare reactions. Check with your doctor before taking any additional medications with an MAO B inhibitor.
. Catechol O-methyltransferase (COMT) inhibitors. Entacapone (Comtan) and opicapone (Ongentys) are the primary medications from this class. This medication mildly prolongs the effect of levodopa therapy by blocking an enzyme that breaks down dopamine.
Side effects, including an increased risk of involuntary movements (dyskinesia), mainly result from an enhanced levodopa effect. Other side effects include diarrhea, nausea or vomiting.
Tolcapone (Tasmar) is another COMT inhibitor that is rarely prescribed due to a risk of serious liver damage and liver failure.
. Anticholinergics. These medications were used for many years to help control the tremor associated with Parkinson’s disease. Several anticholinergic medications are available, including benztropine (Cogentin) or trihexyphenidyl.
However, their modest benefits are often offset by side effects such as impaired memory, confusion, hallucinations, constipation, dry mouth and impaired urination.
. Amantadine. Doctors may prescribe amantadine alone to provide short-term relief of symptoms of mild, early-stage Parkinson’s disease. It may also be given with carbidopa-levodopa therapy during the later stages of Parkinson’s disease to control involuntary movements (dyskinesia) induced by carbidopa-levodopa.
Side effects may include a purple mottling of the skin, ankle swelling or hallucinations.
Read more about : Arachnoid cyst size chart
Surgical procedures
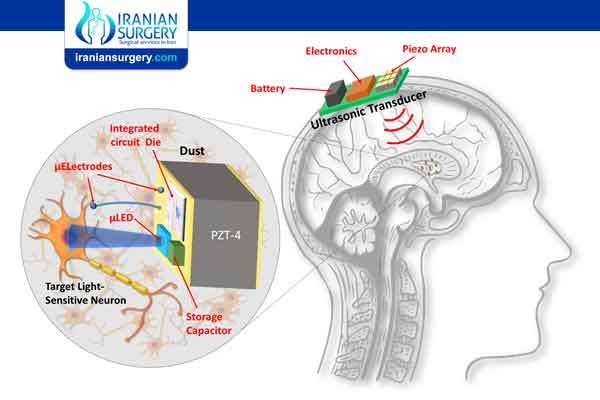
. Deep brain stimulation. In deep brain stimulation (DBS), surgeons implant electrodes into a specific part of your brain. The electrodes are connected to a generator implanted in your chest near your collarbone that sends electrical pulses to your brain and may reduce your Parkinson’s disease symptoms.
Your doctor may adjust your settings as necessary to treat your condition. Surgery involves risks, including infections, strokes or brain hemorrhage. Some people experience problems with the DBS system or have complications due to stimulation, and your doctor may need to adjust or replace some parts of the system.
Deep brain stimulation is most often offered to people with advanced Parkinson’s disease who have unstable medication (levodopa) responses. DBS can stabilize medication fluctuations, reduce or halt involuntary movements (dyskinesia), reduce tremor, reduce rigidity, and improve slowing of movement.
DBS is effective in controlling erratic and fluctuating responses to levodopa or for controlling dyskinesia that doesn’t improve with medication adjustments.
However, DBS isn’t helpful for problems that don’t respond to levodopa therapy apart from a tremor. A tremor may be controlled by DBS even if the tremor isn’t very responsive to levodopa.
Although DBS may provide sustained benefit for Parkinson’s symptoms, it doesn’t keep Parkinson’s disease from progressing.
After Parkinson’s disease
After Deep Brain Stimulation Surgery
The average hospital stay following implantation of the DBS leads is 1 to 2 days. Most patients are able to return home on the same day that their battery is placed.
A few weeks after surgery, the pulse generator in your chest is activated in your doctor’s office. The doctor can easily program your pulse generator from outside your body using a special remote control. The amount of stimulation is customized to your condition, and may take as long as four to six months to find the optimal setting.
Stimulation may be constant, 24 hours a day, or your doctor may advise you to turn your pulse generator off at night and back on in the morning, depending on your condition. You can turn stimulation on and off with a special remote control that you’ll take home with you. In some cases, your doctor may program the pulse generator to let you make minor adjustments at home.
The battery life of your generator varies with usage and settings. When the battery needs to be replaced, your surgeon will replace the generator during an outpatient procedure.
Recovery
. Your stitches or staples will be removed 10 to 14 days after surgery.
. Each of the 4 pin sites should be kept covered with band aids until they are dry. These should be changed every day as necessary.
. You will be able to wash your head with a damp cloth, avoiding the surgical area.
. You may only shampoo your hair the day after your stitches or staples are removed, but only very gently.
. You should not scratch or irritate the wound areas.
. You should not engage in light activities for 2 weeks after surgery. This includes housework and sexual activity.
. You should not engage in heavy activities for 4 to 6 weeks after surgery. This includes jogging, swimming, or any physical education classes. Anything strenuous should be avoided to allow your surgical wound to heal properly. If you have any questions about activities, call your doctor before performing them.
. You should not lift more than 5 lbs. for at least 2 weeks.
. You should not raise your arms above your shoulders or over bend or stretch your neck.
. Depending on the type of work you do, you may return to work within 4 to 6 weeks.
Is Parkinson’s disease fatal?
Parkinson’s disease itself doesn’t cause death. However, symptoms related to Parkinson’s can be fatal. For example, injuries that occur because of a fall or problems associated with dementia can be fatal.
Some people with Parkinson’s experience difficulty swallowing. This can lead to aspiration pneumonia. This condition is caused when foods, or other foreign objects, are inhaled into the lungs.

13 Responses
Can Parkinson’s be cured?
Not yet. However, many PD symptoms can be treated and researchers are making advances in understanding the disease, its causes and how to best treat it
Is there a special MS diet?
There is no specific dietary recommendation for MS. For someone without MS, certain aspects of how you eat have been shown to reduce the risk of MS. Specific diets have been shown to improve certain symptoms in those with MS.
Decreasing Risk
Studies that examine patterns in health across specific populations demonstrate that a “Westernized” diet (high in fat, salt, sugar, and processed food, and low in vegetables) is associated with increased MS risk. Moreover, obesity is a risk factor for developing MS, possibly because it contributes to chronic inflammation. These facts, taken together, indicate that diet may be a factor in developing MS, but it remains to be seen whether diet can play a role in stopping the disease.
Improving Symptoms
While no diet regimen has been shown to slow, stop, or reverse the damage caused by MS, specific diets have shown some benefit for symptom management in clinical trials.
Among those diets that have shown positive trial results, the most noted effect was a reduction in fatigue. Participants also improved their general health, including weight and blood lipid levels. Among these diets studied specifically for MS, there are some differences and similarities.
How is Parkinson’s inherited?is it about genetic mutation?
Studies show that some cases of Parkinson’s disease are caused by geneticmutations. Hereditary causes of this disease are rare. Only 15 percent of those who have Parkinson’s disease have a family history of it. … Research suggests that a combination of genetic and environmental factors may cause Parkinson’s disease
Is there any drug for Parkinson to introduce to me?
Dear user,your Gp or your specialist is aim to find the best treatment for you as an individual.
After my PD diagnosis, I started out taking only Azilect, then Mirapex and sinemet as the disease progressed but didn’t help much. In July last year, I started on PARKINSON DISEASE TREATMENT PROTOCOL from Herbal Health Point (ww w. herbalhealthpoint. c om). Few months into the treatment, I made a significant recovery. After I completed the recommended treatment plan, almost all my symptoms were gone, had wonderful improvement with my movement and tremors . Its been 6 months since I completed the treatment, I live a better life
In February last year, I was diagnosed of PARKINSON DISEASE. I started out taking only Azilect, then Mirapex and sinemet as the disease progressed but didn’t help much. In July, I started on PARKINSON DISEASE TREATMENT PROTOCOL from Herbal Health Point (ww w. herbalhealthpoint. c om). One month into the treatment, I made a significant recovery. After I completed the recommended treatment, almost all my symptoms were gone, wonderful improvement with my movement and tremors .
I am 65 years old, I was diagnosed of Parkinson’s disease at the age of 59. I had severe calf pain, muscle pain, slurred speech, frequent falls, loss of balance, difficulty getting up from sitting position. i was on Carbidopa and Pramipexole for two years, as the disease progressed my symptoms worsened, with my neurologist guidance i started on natural PARKINSON’S DISEASE TREATMENT from Rich Herbal garden w w w. richherbalgardens. c o m The treatment worked very effectively for my Parkinson’s, most of my severe symptoms simply vanished within the first 3 months on the treatment, i feel better now than I have felt in years and i can feel my strength again. My neurologist was very open when looking at alternative medicines and procedures, this alternative Parkinson’s disease treatment is indeed a breakthrough.
After was running around from doctor to doctor before we finally get rid of her PD ,at age 74 my mother noticed that her handwriting was getting smaller and I was writing faster as well. She also noticed a small tremor in her left hand. The doctor went over her different symptoms and he suspected she either had a small stroke or the beginnings of Parkinson ‘s disease. After finding a neurologist and some testing she was diagnosed with the beginning stages of Parkinson’s disease. That was 3 years ago. She take Sinimet four times a day to control the symptoms, which include falling, imbalance, gait problems, swallowing difficulties, and slurring of speech,This year, our family doctor started her on totalcureherbsfoundation com PD Herbal mixture, over 3 months into treatment she improved me dramatically. At the end of the full treatment course, the disease is totally under control. No case of dementia, hallucination, weakness, muscle pain or tremors.PD or any other disease natural organic remedies are always work on acidity treatment, if we maintain diet plan and use total cure herbs foundation then we get fast relief from this problem.
I was introduced to HERBAL HEALTH POINT and their effective PD treatment protocol in February last year. I immediately started on the herbal treatment, it relieved my symptoms significantly. Go to ww w. herbalhealthpoint. c om. First month on the treatment, my tremors and muscle spasm mysterious stopped, had improvement walking. Since treatment, I have been symptom free and life is really good