How do I prepare for a cystocele and rectocele repair?
Rectocele symptoms
How long does it take to recover from Rectocele and Cystocele surgery?
What are the benefits of this procedure?
What are the risks associated with this procedure?
Is Rectocele repair major surgery?
Can you have both Cystocele and Rectocele?
Can a Cystocele cause bowel problem?
Cystocele and rectocele repair surgery
A cystocele is when part of the bladder wall bulges into the vagina. The bulge happens through a defect in the wall between the bladder and vagina. A rectocele is when part of the wall of the rectum bulges into the vagina. The bulge happens through a defect in the wall between the rectum and vagina. These form because of a problem with the fascia, ligaments, and muscles of the pelvis.
Cystocele and rectocele can cause problems going to the bathroom such as frequent urination, urine leakage, and difficulty urinating. Pain during sex may also occur. This surgery is done to help relieve these symptoms.
Most often, this type of surgery is not done until all other treatments have been tried. Other treatments may include muscle exercises and the insertion of a supportive device called a pessary. If you have tried these treatments and have had no relief, your doctor may suggest surgical repair.
A cystocele and rectocele repair are an operation that lifts and tightens the tissue around the bladder and rectum so these organs no longer push against the vagina. This procedure is also known as an Anterior and Posterior Repair.
The procedure should allow easy, effective, and complete urination and better bowel control. It helps to be more active. You might be able to resume your normal level of activity without leaking urine. Bulging and pressure sensations in the vagina will be relieved.
Perineoplasty (also perineorrhaphy) denotes the plastic surgery procedures used to correct clinical conditions (damage, defect, deformity) of the vagina and the anus. Among the vagino-anal conditions resolved by perineoplasty are vaginal looseness, vaginal itching, damaged perineum, incontinence, genital warts, dyspareunia, intraoital stenosis, vaginismus, vulvar vestibulitis, and decreased sexual sensation. Depending upon the vagino-anal condition to be treated, there are two variants of the perineoplasty procedure: the first, to tighten the perineal muscles and the vagina; the second, to loosen the perineal muscles.
Read more about : Cervical cancer treatment
Read more about : Risk factors of cervical cancer
Read more about : Cystoscopy for female
When is it used?
Surgery is done to relieve bulging into the vagina that may be caused by a cystocele and rectocele. Surgery is usually used only after you have tried other treatments such as:
Doing muscle-strengthening exercises, called Kegel exercises.
Placing a pessary in the vagina (a device that supports the vaginal walls). A pessary does not help a rectocele problem, but it can help with a cystocele.
Ask your doctor about these other treatment choices.
Cystocele risk factors
Risk factors for a cystocele include:
- Vaginal births, which may involve straining the muscles of the floor of the pelvis.
- Family history.
- Obesity.
- Intense physical activity, including lifting heavy objects.
- Hysterectomy.
- Constipation and/or repeated muscle straining during bowel movements.
- Frequent coughing.
- Aging and a drop in the hormone estrogen. Estrogen helps keep muscles around the vagina strong, but women produce less estrogen as they enter menopause (the end of menstrual periods).
Read more about: Cystocele and rectocele repair with hysterectomy
Read more about: Pessary for cystocele and rectocele
Rectocele symptoms
A small rectocele may cause no symptoms.
In mild cases of rectocele, the individual may notice pressure within the vagina, or they may feel that their bowels are not completely empty after using the bathroom.
In moderate cases, an attempt to evacuate can push the stool into the rectocele rather than out through the anus.
There may be pain and discomfort during evacuation. There is a higher chance of having constipation, and there may be pain during sexual intercourse.
Some say it feels as if “something is falling out” or down within the pelvis.
In severe cases, there may be fecal incontinence, and sometimes the bulge may prolapse through the mouth (opening) of the vagina, or through the anus.
How do I prepare for a cystocele and rectocele repair?
Plan for your care and recovery after the operation. Allow for time to rest and try to find people to help you with your day-to-day duties.
Follow instructions provided by your doctor. You may be asked to take an enema or medicine to clean out your bowel the day before surgery. Eat a light meal, such as soup or salad, the night before the procedure. Do not eat or drink anything after midnight or the morning before the procedure. Do not even drink coffee, tea or water.
During the surgery
You are given a regional or general anesthetic. A regional anesthetic numbs part of your body while you remain awake. A general anesthetic relaxes your muscles, makes you feel as if you are in a deep sleep, and prevents you from feeling pain.
The doctor will make two cuts in the wall of the vagina, exposing the tissue between the vagina and the bladder and the tissue between the vagina and the rectum. The doctor will try to support these organs by bringing tissue around them. He or she will remove any tissue from the vaginal wall that has stretched from aging or pregnancy. If incontinence is a significant symptom, the doctor may also perform an elevation or suspension procedure on the bladder. Cuts in the vagina will be sewn closed.
The doctor may place a catheter (a tube for urine passage) in your bladder and lead it out through a cut made in your lower abdominal wall. This makes urinating easier during recovery and decreases the pressure inside the bladder.
Read more about: Cystocele and rectocele recovery time
Read more about: Rectocele repair complications
After the surgery
You may stay in the hospital anywhere from 2 to 6 days. The catheter may remain in your bladder 2 to 6 days or until your bladder starts working normally again. You may be constipated during this time.
During the first 4 weeks after the operation, there may be some smelly, sometimes bloody drainage from your vagina.
After you leave the hospital, avoid all heavy activity such as lifting for the first 6 to 8 weeks. Then gradually increase your activity during the next 4 weeks.
Ask what other steps you should take and schedule checkups with the doctor 2 and 4 weeks after the operation.
How long does it take to recover from Rectocele and Cystocele surgery?
You can expect to feel better and stronger each day, although you may get tired quickly and need pain medicine for a week or two. You may need about 4 to 6 weeks to fully recover from open surgery and 1 to 2 weeks to recover from laparoscopic surgery or vaginal surgery.
It is important to avoid heavy lifting while you are recovering, so that your incision can heal.
This care sheet gives you a general idea about how long it will take for you to recover. But each person recovers at a different pace. Follow the steps below to get better as quickly as possible.
What are the benefits of this procedure?
This procedure should allow easy, effective and complete urination and better bowel control. It should help you to be more active. You might be able to resume your normal level of activity without leaking urine. Bulging and pressure sensations in the vagina also will be relieved.
Read more about: Differences between a cystocele and a rectocele
Read more about: Cystocele and rectocele symptoms
What are the risks associated with this procedure?
There are some risks when you have general anesthesia. Discuss these risks with your doctor.
The regional anesthetic may not numb the area quite enough and you may feel some minor discomfort.
There may be damage to the bladder and rectum. If damage occurs and the doctor is aware of it, he or she will try to correct it during the operation.
There may be infection or bleeding. You should ask your doctor how these risks apply to you.
Read more about: Vitrectomy surgery
Read more about: Rectocele Repair Surgery
When should I call the doctor?
Call the doctor immediately if:
The catheter becomes plugged and makes it hard to urinate.
You develop a fever.
You have heavy bleeding from your vagina.
Is Rectocele repair major surgery?
You may stay in the hospital anywhere from 2 to 6 days. The catheter may remain in your bladder 2 to 6 days or until your bladder starts working normally again. Rectocele repair is a major surgery. A doctor will often suggest it only after other treatments have failed to correct your problem.
Can you have both Cystocele and Rectocele?
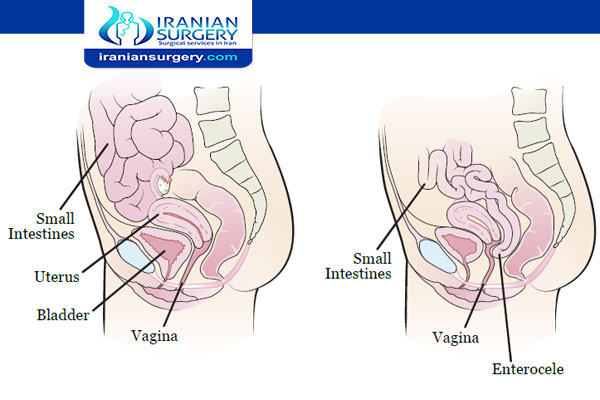
Anterior and posterior vaginal wall prolapse involve protrusion of an organ into the vaginal canal. Anterior vaginal wall prolapse is commonly referred to as cystocele or urethrocele (when the bladder or urethra is involved). Posterior vaginal wall prolapse is commonly referred to as enterocele (when the small intestine and peritoneum are involved) and rectocele (when the rectum is involved). Symptoms include pelvic or vaginal fullness or pressure. Diagnosis is clinical. Treatment includes conservative management with observation, pessaries, pelvic muscle exercises, and sometimes surgery.
Cystocele, urethrocele, enterocele, and rectocele are particularly likely to occur together. Urethrocele is virtually always accompanied by cystocele (cystourethrocele).
Cystocele and cystourethrocele commonly develop when the pubocervical vesical fascia is weakened. Enterocele usually occurs after a hysterectomy. Weakness in the pubocervical fascia and rectovaginal fascia allows the apex of the vagina, which contains the peritoneum and small bowel, to descend. Rectocele results from disruption of the levator ani muscles.
Read more about: Cystocele surgery
Read more about: Cystocele and rectocele recovery time
Can a Cystocele cause bowel problem?
The rectum may also press into the vagina. This problem is called a rectocele. It can cause trouble with bowel movements. For example, you may have bowel movements less often or you may have leaking of bowel movements. Urinary problems such as slow stream, a feeling of incomplete bladder emptying, frequency, urgency and stress urinary incontinence. Bowel problems such as difficulty moving the bowel or a feeling of not emptying properly. Discomfort during sexual intercourse.
Read more about: Cystocele and rectocele at the same time
Read more about: Bartholin cyst surgery


2 Comments
I don’t know anything about causes of cystocele,pls explaine more about it and thank youuu
Symptoms of a cystocele include urine leakage and incomplete emptying of the bladder. Causes of cystocele include muscle straining during childbirth, straining from heavy lifting, repeated straining during bowel movements, and menopause.