Cervical Cerclage
What is Cervical Cerclage?
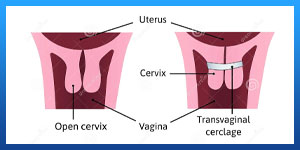
Cervical cerclage refers to a variety of procedures that use sutures or synthetic tape to reinforce the cervix during pregnancy in women with a history of a short cervix. The cervix is the lower part of the uterus that opens to the vagina.
Cervical cerclage can be done through the vagina (transvaginal cervical cerclage) or, less commonly, through the abdomen (transabdominal cervical cerclage).
Your health care provider might recommend cervical cerclage if your cervix is at risk of opening before your baby is ready to be born or, in some cases, if your cervix begins to open too early. However, cervical cerclage isn’t appropriate for everyone. It can cause serious side effects and doesn’t always work. Some women who have a cerclage placed for a short cervix might experience preterm labor. Understand the risks of cervical cerclage and whether the procedure might benefit you and your baby.
Read more about : C-Section (Cesarean Section) Recovery
Read more about : Clitoromegaly surgery pictures
Read more about : how to pop a bartholin cyst yourself?
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Surgeons in Iran. The price of a cervical cerclage procedure in Iran can vary according to each individual’s case and will be determined based on an in-person assessment with the doctor. So if you are looking for the cost of cervical cerclage procedure in Iran, you can contact us and get free consultation from Iranian surgery.
Before Cervical Cerclage Procedure
Why it’s done
Before pregnancy, the cervix is closed, long and firm. During pregnancy, the cervix gradually softens, decreases in length (effaces) and opens (dilates) in preparation for birth. If you have an incompetent or short cervix, however, your cervix might begin to open too soon. As a result, you could experience pregnancy loss or give birth prematurely.
Your health care provider might recommend cervical cerclage during pregnancy to prevent premature birth if you have:
. A history of second trimester pregnancy loss related to painless cervical dilation in the absence of labor or placental abruption (history-indicated cervical cerclage).
. Prior cerclage due to painless cervical dilation in the second trimester
. Painless cervical dilation diagnosed during the second trimester
. A short cervical length (less than 25 millimeters) before 24 weeks of pregnancy, in a singleton pregnancy.
Cervical cerclage isn’t appropriate for everyone at risk of premature birth. Your health care provider might not recommend a cervical cerclage if you have:
. Active vaginal bleeding
. Active preterm labor
. An intrauterine infection
. Preterm premature rupture of membranes — when the fluid-filled membrane that surrounds and cushions the baby during pregnancy (amniotic sac) leaks or breaks before week 37 of pregnancy.
. Twin or higher order pregnancy
. A fetal anomaly incompatible with life
. Prolapsed fetal membranes — a condition in which the amniotic sac protrudes through the opening of the cervix.
Read more about : Cervical cancer treatment
Read more about : Risk factors of cervical cancer
Read more about : Early symptoms of Cervical cancer
What are the benefits of cervical cerclage?
Cervical cerclage prevents miscarriage or preterm delivery or labour. The success rate of this procedure is about to 85% to 90%. This procedure is effective if there is truly a weak cervix, however the diagnosis of this can be inaccurate.
Risks
What are the risks of cervical cerclage?
Risks associated with cervical cerclage include:
. Inflammation of the fetal membranes due to a bacterial infection
. Vaginal bleeding
. A tear in the cervix (cervical laceration)
. Preterm premature rupture of the membranes — when the fluid-filled membrane that surrounds and cushions the baby during pregnancy (amniotic sac) leaks or breaks before week 37 of pregnancy.
. Suture displacement
When should I contact my doctor?
After receiving a cervical cerclage, contact your health care provider immediately if you have leakage of fluid from your vagina, a sign of preterm premature rupture of membranes. Your health care provider will recommend removing the cervical cerclage early if you have preterm premature rupture of membranes or if you have symptoms that suggest a uterine infection.
How you prepare
Before cervical cerclage, your health care provider will do an ultrasound to check your baby’s vital signs and rule out any major birth defects. Your health care provider might take a swab of your cervical secretions or do amniocentesis — a procedure in which a sample of amniotic fluid is removed from the uterus — to check for infection. If you have an infection, a cerclage won’t be placed.
Ideally, a history-indicated cervical cerclage is done between weeks 12 and 14 of pregnancy. However, cervical cerclage can be done up until week 23 of pregnancy if a pelvic exam or ultrasound shows that your cervix is beginning to open. Cervical cerclage is typically avoided after week 24 of pregnancy due to the risk of rupturing the amniotic sac and triggering premature birth.
Read more about 2nd iui success rate
Read more about Virgin tightening surgery before and after
Read more about Ovarian cyst size chart
During Cervical Cerclage Procedure
What you can expect
Cervical cerclage is typically done as an outpatient procedure at a hospital or surgery center under regional or general anesthesia. Most cervical cerclage procedures are done through the vagina.
Cervical cerclage might be done through the abdomen if transvaginal cerclage is unsuccessful or anatomically difficult due to an extremely short, lacerated or scarred cervix.
During the procedure
During transvaginal cervical cerclage, your health care provider will insert a speculum into your vagina and grasp your cervix with ring forceps. He or she might use ultrasound for guidance. Your health care provider will likely use the McDonald operation or the Shirodkar operation. Data suggests no significant difference in outcomes between the two methods.
During the McDonald operation, your health care provider will use a needle to put stitches around the outside of your cervix. Next, he or she will tie the ends of the sutures to close your cervix.
During the Shirodkar operation, your health care provider will use ring forceps to pull your cervix toward him or her while pulling back the side walls of your vagina. Next, he or she will make small incisions in your cervix where it meets your vaginal tissue. Then, he or she will pass a needle with tape through the incisions and tie your cervix closed. Your health care provider might use stitches to reposition vaginal tissue affected by the incisions.
During transabdominal cervical cerclage, your health care provider will make an abdominal incision. He or she might elevate your uterus to gain better access to your cervix. Next, your health care provider will use a needle to place tape around the narrow passage connecting the lower part of your uterus to your cervix and tie your cervix closed. Then he or she will set your uterus back into place and close the incision. The procedure also can be done laparoscopically.
Cervical cerclage removal
A transvaginal cervical cerclage is typically removed at around week 37 of pregnancy — or at the start of preterm labor.
A McDonald cerclage can usually be removed in a health care provider’s office without anesthetic, while a Shirodkar cerclage might need to be removed in a hospital or surgery center. After having a transvaginal cervical cerclage removed, you’ll typically be able to resume your usual activities as you wait for labor to begin naturally.
If you expect to have a C-section and plan to have children in the future, you might choose to leave a Shirodkar cerclage in place throughout your pregnancy and after the baby is born. However, it’s possible that the cerclage could affect your future fertility. Consult your health care provider about your options.
If you had a transabdominal cervical cerclage, you’ll need to have another abdominal incision to remove the cerclage. As a result, a C-section is typically recommended. Your baby will be delivered through an incision made above the cerclage. During the C-section, you can choose to have the cerclage removed or leave it in place for future pregnancies.
Alternatives to Cervical Cerclage
Depending on the condition, a woman may have some alternative therapies available to her to avoid or delay premature labour instead of cervical cerclage. These include:
. Bed rest after cervical cerclage is prescribed so that there is less pressure on the cervix.
. There are drugs that are designed to stop or delay labor (Ritrodrine, terbutaline, and magnesium sulfate).
. Antibiotics may be prescribed to prevent preterm delivery.
Read more about : ovarian cyst size chart
Read more about : clitoromegaly surgery pictures
Read more about : amoxicillin for bartholin cyst
After Cervical Cerclage Procedure
After the procedure
After cervical cerclage, your health care provider will do an ultrasound to check your baby’s well-being.
You might experience some spotting, cramps and painful urination for a few days. Acetaminophen (Tylenol, others) is recommended for pain or discomfort. If your health care provider used stitches to reposition vaginal tissue affected by incisions in your cervix, you might notice passage of the material in two to three weeks as the stitches dissolve.
If you had history-indicated cervical cerclage, you’ll likely be able to go home after you recover from the anesthetic. As a precaution, your health care provider might recommend avoiding sex for a few weeks or more, depending on the reason for the cerclage.
If you had cervical cerclage because your cervix had already begun to open or an ultrasound showed that your cervix is short, you might need to remain in the hospital for observation. As a precaution, your health care provider might recommend limiting physical activity and sex until delivery.
Your health care provider will continue to monitor you closely for signs or symptoms of preterm labor.
Cervical Cerclage Aftercare
It is important that you recover well after the cervical stitches have been placed. Your doctor may keep you under observation for few hours to ensure that you do not go into premature labour, post which you will be allowed to go home with restrictions and guidelines to be followed. The process of recovery after cervical cerclage include medication, reduced or no physical activity, abstinence from sex, regular weekly or bi-weekly visits to the doctor.
. Constipation: After the cerclage has been placed, do not try to push the bowel movement too hard. You may want to make changes in your diet, like have high-fiber foods and more fluids. If required you may use over-the-counter stool softener medicines too.
. Rest: Ample rest will be required post the cerclage procedure.
. Vaginal care: The vaginal area should be carefully washed with soap and water. You should avoid placing anything inside your vagina during this time.
Results
The effectiveness of cervical cerclage is a topic of debate.
Research suggests that cervical cerclage reduces the risk of premature birth in women with proven cervical insufficiency. However, the timing of cervical cerclage can also affect the outcome. Emergency cervical cerclage done in the presence of advanced cervical change and prolapsed membranes has a poorer outcome.
Success Rate of Cerclage Stitch
Performing a cerclage stitch of a combination of procedures cannot assure a successful full-term pregnancy. The doctors at the most reduce the risk for you and your baby. Cerclages work best when they are placed early in pregnancy. The success rate for cervical cerclages is between 85%-90%. The success rate is calculated by assessing the number of pregnancies delivered closer to the term with the procedure. Emergency cerclage has the lowest success rate.
Pregnancy after a Cerclage
There is no evidence that future pregnancies will be affected if you have had a cerclage before. However, in most cases, the doctor prefers putting a cerclage as a preventive measure if you have had one in your previous pregnancy.
10% of pregnancies end in preterm delivery (delivery before 37th week). Premature birth is a cause of serious health problems, like respiratory issues, regulating body temperature and infections. According to statistics, preterm delivery causes more than 85% long-term disabilities and 75% death among newborns.
A weak cervix may pose a threat to the safety of your pregnancy. The Cervical Cerclage procedure will add a stitch of precaution to avoid any mishaps during the course of pregnancy.
