Colon cancer
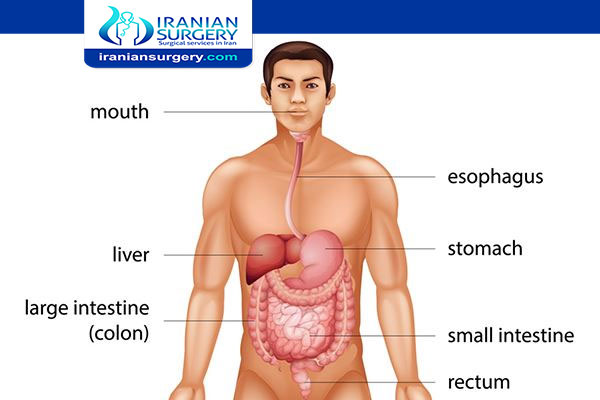
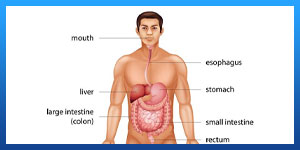
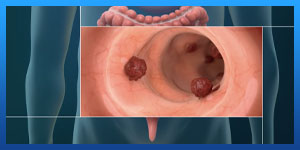
Colon cancer is cancer of the large intestine (colon), which is the final part of your digestive tract. Most cases of colon cancer begin as small, noncancerous (benign) clumps of cells called adenomatous polyps. Over time some of these polyps can become colon cancers.
Polyps may be small and produce few, if any, symptoms. For this reason, doctors recommend regular screening tests to help prevent colon cancer by identifying and removing polyps before they turn into cancer.
Read more about: How you can Prevented from Colorectal Cancer?
Read more about: Colorectal Cancer Recovery
Read more about : Metastatic myxofibrosarcoma treatment with the best Iranian oncologist surgeon
Symptoms
Signs and symptoms of colon cancer include:
- A change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool, that lasts longer than four weeks
- Rectal bleeding or blood in your stool
- Persistent abdominal discomfort, such as cramps, gas or pain
- A feeling that your bowel doesn't empty completely
- Weakness or fatigue
- Unexplained weight loss
Many people with colon cancer experience no symptoms in the early stages of the disease. When symptoms appear, they'll likely vary, depending on the cancer's size and location in your large intestine.
When to see a doctor
If you notice any symptoms of colon cancer, such as blood in your stool or an ongoing change in bowel habits, do not hesitate to make an appointment with your doctor.
Talk to your doctor about when you should begin screening for colon cancer. Guidelines generally recommend that colon cancer screenings begin at age 50. Your doctor may recommend more frequent or earlier screening if you have other risk factors, such as a family history of the disease.
Read more about: Anal fissure surgery
Read more about: Anal cancer treatment
Read more about: Anal abscess treatment
Causes
In most cases, it's not clear what causes colon cancer. Doctors know that colon cancer occurs when healthy cells in the colon develop errors in their genetic blueprint, the DNA.
Healthy cells grow and divide in an orderly way to keep your body functioning normally. But when a cell's DNA is damaged and becomes cancerous, cells continue to divide — even when new cells aren't needed. As the cells accumulate, they form a tumor.
With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body to form deposits there (metastasis).
Inherited gene mutations that increase the risk of colon cancer
Inherited gene mutations that increase the risk of colon cancer can be passed through families, but these inherited genes are linked to only a small percentage of colon cancers. Inherited gene mutations don't make cancer inevitable, but they can increase an individual's risk of cancer significantly.
The most common forms of inherited colon cancer syndromes are:
- Hereditary nonpolyposis colorectal cancer (HNPCC). HNPCC, also called Lynch syndrome, increases the risk of colon cancer and other cancers. People with HNPCC tend to develop colon cancer before age 50.
- Familial adenomatous polyposis (FAP). FAP is a rare disorder that causes you to develop thousands of polyps in the lining of your colon and rectum. People with untreated FAP have a greatly increased risk of developing colon cancer before age 40.
FAP, HNPCC and other, rarer inherited colon cancer syndromes can be detected through genetic testing. If you're concerned about your family's history of colon cancer, talk to your doctor about whether your family history suggests you have a risk of these conditions.
Read more about: Colorectal Cancer Pathophysiology
Read more about: Colorectal Cancer Recovery
Association between diet and increased colon cancer risk
Studies of large groups of people have shown an association between a typical Western diet and an increased risk of colon cancer. A typical Western diet is high in fat and low in fiber.
When people move from areas where the typical diet is low in fat and high in fiber to areas where the typical Western diet is most common, the risk of colon cancer in these people increases significantly. It's not clear why this occurs, but researchers are studying whether a high-fat, low-fiber diet affects the microbes that live in the colon or causes underlying inflammation that may contribute to cancer risk. This is an area of active investigation and research is ongoing.
Risk factors
Factors that may increase your risk of colon cancer include:
- Older age. The great majority of people diagnosed with colon cancer are older than 50. Colon cancer can occur in younger people, but it occurs much less frequently.
- African-American race. African-Americans have a greater risk of colon cancer than do people of other races.
- A personal history of colorectal cancer or polyps. If you've already had colon cancer or adenomatous polyps, you have a greater risk of colon cancer in the future.
- Inflammatory intestinal conditions. Chronic inflammatory diseases of the colon, such as ulcerative colitis and Crohn's disease, can increase your risk of colon cancer.
- Inherited syndromes that increase colon cancer risk. Genetic syndromes passed through generations of your family can increase your risk of colon cancer. These syndromes include familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer, which is also known as Lynch syndrome.
- Family history of colon cancer. You're more likely to develop colon cancer if you have a parent, sibling or child with the disease. If more than one family member has colon cancer or rectal cancer, your risk is even greater.
- Low-fiber, high-fat diet. Colon cancer and rectal cancer may be associated with a diet low in fiber and high in fat and calories. Research in this area has had mixed results. Some studies have found an increased risk of colon cancer in people who eat diets high in red meat and processed meat.
- A sedentary lifestyle. If you're inactive, you're more likely to develop colon cancer. Getting regular physical activity may reduce your risk of colon cancer.
- Diabetes. People with diabetes and insulin resistance have an increased risk of colon cancer.
- Obesity. People who are obese have an increased risk of colon cancer and an increased risk of dying of colon cancer when compared with people considered normal weight.
- Smoking. People who smoke may have an increased risk of colon cancer.
- Alcohol. Heavy use of alcohol increases your risk of colon cancer.
- Radiation therapy for cancer. Radiation therapy directed at the abdomen to treat previous cancers increases the risk of colon and rectal cancer.
Read more about: Does colorectal cancer occur in old people?
Read more about: colorectal cancer risk factors
Prevention
Get screened for colon cancer
People with an average risk of colon cancer can consider screening beginning at age 50. But people with an increased risk, such as those with a family history of colon cancer, should consider screening sooner.
Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you.
Make lifestyle changes to reduce your risk
You can take steps to reduce your risk of colon cancer by making changes in your everyday life. Take steps to:
- Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains contain vitamins, minerals, fiber and antioxidants, which may play a role in cancer prevention. Choose a variety of fruits and vegetables so that you get an array of vitamins and nutrients.
- Drink alcohol in moderation, if at all. If you choose to drink alcohol, limit the amount of alcohol you drink to no more than one drink a day for women and two for men.
- Stop smoking. Talk to your doctor about ways to quit that may work for you.
- Exercise most days of the week. Try to get at least 30 minutes of exercise on most days. If you've been inactive, start slowly and build up gradually to 30 minutes. Also, talk to your doctor before starting any exercise program.
- Maintain a healthy weight. If you are at a healthy weight, work to maintain your weight by combining a healthy diet with daily exercise. If you need to lose weight, ask your doctor about healthy ways to achieve your goal. Aim to lose weight slowly by increasing the amount of exercise you get and reducing the number of calories you eat.
Colon cancer prevention for people with a high risk
Some medications have been found to reduce the risk of precancerous polyps or colon cancer. However, not enough evidence exists to recommend these medications to people who have an average risk of colon cancer. These options are generally reserved for people with a high risk of colon cancer.
For instance, some evidence links a reduced risk of polyps and colon cancer to regular use of aspirin or aspirin-like drugs. But it's not clear what dose and what length of time would be needed to reduce the risk of colon cancer. Taking aspirin daily has some risks, including gastrointestinal bleeding and ulcers, so doctors typically don't recommend this as a prevention strategy unless you have an increased risk of colon cancer.
Reference:
https://www.mayoclinic.org/diseases-conditions/colon-cancer/symptoms-causes/syc-20353669
[kkstarratings]