Hysterectomy
What is Hysterectomy?
A hysterectomy is a surgical procedure to remove a woman’s uterus. The uterus, also known as the womb, is where a baby grows when a woman is pregnant. The uterine lining is the source of menstrual blood.
You may need a hysterectomy for many reasons. The Hysterectomy surgery can be used to treat a number of chronic pain conditions as well as certain types of cancer and infections. The extent of a hysterectomy varies depending on the reason for the surgery.
Once you’ve had a hysterectomy surgery, you’ll stop having menstrual periods. You’ll also be unable to get pregnant.
Read more about: What is Hysteroscopy?
Read more about: how to pop a Bartholin cyst yourself?
Read more about: ovarian cyst size chart
Read more about: clitoromegaly surgery pictures
Before Hysterectomy Procedure
Why it's done
Your doctor may suggest a hysterectomy if you have any of the following:
. Chronic pelvic pain
. Uncontrollable vaginal bleeding
. Cancer of the uterus, cervix, or ovaries
. Fibroids, which are benign tumors that grow in the uterus
. Pelvic inflammatory disease, which is a serious infection of the reproductive organs.
. Uterine prolapse, which occurs when the uterus drops through the cervix and protrudes from the vagina.
. Endometriosis, which is a disorder in which the inner lining of the uterus grows outside of the uterine cavity, causing pain and bleeding.
. Adenomyosis, which is a condition in which the inner lining of the uterus grows into the muscles of the uterus.

Side effects and Complications
Side-effects of a hysterectomy
Side-effects are the unwanted, but mostly temporary effects, you may get after having the operation.
Side-effects of a hysterectomy include:
. Pain and discomfort in your lower tummy (for a few days)
. Bleeding from your vagina (for one to two weeks)
. Feeling tired and emotional (many women find this takes a while to pass)
Complications of a hysterectomy
Complications are problems that can occur during or after the operation. Some of the possible complications after a hysterectomy are:
. Heavy (excessive) bleeding
. A wound or urine infection
. Damage to some of the blood vessels or organs in your abdomen – including your bowel, bladder and ureters (the tubes that carry urine from your kidneys to your bladder).
. Developing a blood clot, usually in a vein in the leg (deep vein thrombosis, DVT) or, rarely, in the lungs (pulmonary embolism).
Preparing for a hysterectomy
Before the operation
Your doctor will give you information about how to prepare for your operation. For example, if you smoke, they will ask you to stop. This is because smoking increases your risk of getting a chest and wound infection, which can slow your recovery.
You’ll usually have an appointment for a pre-op check some time before the operation. This health check is to make sure that you’re well enough for the operation to go ahead as planned. It may include some blood and urine tests.
Depending on what type of hysterectomy you have, and how the operation is done, you should prepare to be in hospital for between one and four days. Make sure you arrange for someone to be available to drive you home after your operation.
On the day
It's very important to follow any instructions you’re given about how to prepare for your procedure. These may include when to stop eating and drinking before your operation if you’re having a general anaesthetic. If you have any questions, just ask.
You should be asked to wear compression stockings to help prevent blood clots forming in the veins in your legs. You may need to have an injection of an anti-clotting medicine as well as or instead of wearing compression stockings.
Your nurse or doctor will discuss with you what will happen, including any pain you might have. If you’re unsure about anything, ask. It’s important that you feel fully informed so you’re in a position to give your consent for the operation to go ahead. You’ll be asked to sign a consent form.
Read more about: Cervical cancer treatment
Read more about: Risk factors of cervical cancer
Read more about: Early symptoms of cervical cancer
During Hysterectomy Procedure
Hysterectomy Types
What are the types of Hysterectomy?
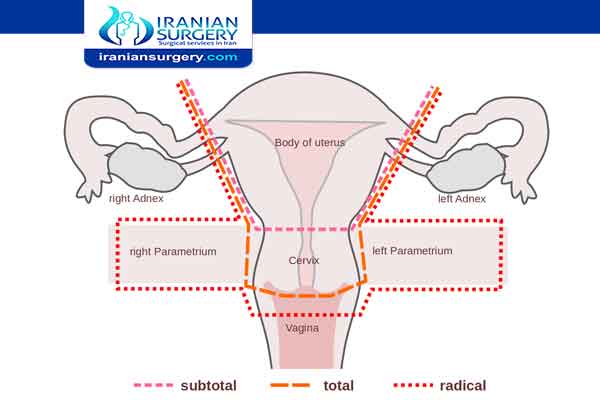
There are several different types of hysterectomy.
. Partial Hysterectomy
During a partial hysterectomy, your doctor removes only a portion of your uterus. They may leave your cervix intact.
. Total Hysterectomy
During a total hysterectomy, your doctor removes the entire uterus, including the cervix. You’ll no longer need to get an annual Pap test if your cervix is removed. However, you should continue to have regular pelvic examinations.
. Hysterectomy and Salpingo-Oophorectomy
During a hysterectomy and salpingo-oophorectomy, your doctor removes the uterus along with one or both of your ovaries and fallopian tubes. You may need hormone replacement therapy if both of your ovaries are removed.
During Procedure
How is a Hysterectomy performed?
A hysterectomy can be performed in several ways. All methods require a general or local anesthetic. A general anesthetic will put you to sleep throughout the procedure so that you don’t feel any pain. A local anesthetic will numb your body below the waistline, but you’ll remain awake during the surgery. This type of anesthetic will sometimes be combined with a sedative, which will help you feel sleepy and relaxed during the procedure.
. Abdominal Hysterectomy
During an abdominal hysterectomy, your doctor removes your uterus through a large cut in your abdomen. The incision may be vertical or horizontal. Both types of incisions tend to heal well and leave little scaring.
. Vaginal Hysterectomy
During a vaginal hysterectomy, your uterus is removed through a small incision made inside the vagina. There are no external cuts, so there won’t be any visible scars.
. Laparoscopic Hysterectomy
During a laparoscopic hysterectomy, your doctor uses a tiny instrument called a laparoscope. A laparoscope is a long, thin tube with a high-intensity light and a high-resolution camera at the front. The instrument is inserted through incisions in the abdomen. Three or four small incisions are made instead of one large incision. Once the surgeon can see your uterus, they’ll cut the uterus into small pieces and remove one piece at a time.
Alternatives to hysterectomy
For conditions like fibroids and endometriosis, there are alternative treatments. For example, your doctor may suggest medicines or hormone treatments. If you have fibroids and you want to have children, you might be able to have a procedure called a myomectomy. This is when the fibroids are taken out and your womb is left intact. Hysterectomy is usually offered when other treatments have been tried, but haven’t worked.
If you have cancer of your ovary or womb, then hysterectomy is likely to be offered as the first choice of treatment.
Whatever your situation, talk to your doctor about the treatment choices available to you.
After Hysterectomy Procedure
Aftercare for hysterectomy
You’ll need to rest until the effects of your anaesthetic have worn off. You might find that you're not so coordinated or that it's difficult to think clearly. This should pass within 24 hours.
You’re likely to have some pain and discomfort in your lower abdomen for a few days after your operation. If you’ve had a laparoscopic hysterectomy you may have some pain in your shoulder too. Ask your nurse for painkillers if you need them.
You may have a catheter in for about 24 hours after your operation. This drains urine through a tube and into a bag. Once you’re able to get up and go to the toilet easily, your nurse will take it out. If you have problems peeing, it may stay in for a few days.
You’ll probably have some bleeding from your vagina for up to two weeks after your operation. Wear a sanitary pad, rather than using a tampon, until any bleeding stops.
You should be able to have a shower the day after your operation, but avoid having a bath for five days after your surgery.
If you’ve had a vaginal hysterectomy, you won’t have any wounds on the outside of your body. Any stitches inside your vagina may come out on their own after a few days or weeks – this is normal.
If you’ve had an abdominal or laparoscopic hysterectomy, you may have stitches or staples which need to be removed. Your nurse will tell you who will do this – often the practice nurse at your GP surgery.
Before you go home, your nurse will advise you about caring for your wounds and may arrange a date for a follow-up appointment.
Recovering from a hysterectomy
Recovery after a hysterectomy is different for every woman. You should build up your activity slowly and gradually and it can take up to eight weeks before things are back to normal for you. Don’t lift anything heavy or do any strenuous housework (like vacuuming) for three to four weeks after having a hysterectomy.
You should be given some painkillers to take home with you. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.
Your doctor may suggest that you do pelvic floor exercises as part of your recovery. Your pelvic floor muscles help to hold your abdominal organs in the right place and keep your bladder and bowel closed. You doctor or nurse will tell you what you need to do and how often.
Going back to work
If you’ve had a vaginal or laparoscopic hysterectomy, you should be able to go back to work between two and six weeks after your operation. If you’ve had an abdominal hysterectomy, this will probably take a little longer. When you go back to work will depend on your job and how well you feel.
Driving
If you’ve had a vaginal or laparoscopic hysterectomy, it can take two to four weeks before you feel comfortable enough, and are safe enough, to drive. If you’ve had an abdominal hysterectomy, this may take longer. You should check with your motor insurance provider in case they have specific conditions for driving after surgery.
Read more about : Treatment For Breast Cancer Stage 1
Read more about : Stage 2 breast cancer treatment timeline
When can I have sex after a hysterectomy?
It’s best to wait four to six weeks after your surgery before you start having sex. This allows your body to heal properly.
If you find sex uncomfortable and your vagina is dry, using a vaginal lubricant usually helps.
When to seek medical help
Contact the hospital or your GP if you develop any of the following symptoms when you’re at home.
. The symptoms of a urine infection – needing to pee urgently and often, pain or discomfort when you’re peeing and smelly or cloudy pee.
. Heavy or smelly bleeding from your vagina, feeling unwell or having a temperature (fever). These could mean you have an infection at the top of the vagina.
. Sore, red skin around your scars from a wound infection.
. Abdominal pain that’s severe or getting worse, along with being sick, a fever and not feeling like eating. This could be a symptom of damage to your bladder or bowel from the operation.
Life after a hysterectomy
A hysterectomy permanently changes some aspects of your life. For instance:
. You'll no longer have menstrual periods.
. Most of the time, you'll get relief from the symptoms that made your surgery necessary.
. You won't be able to become pregnant.
. If you're premenopausal, having your ovaries removed along with a hysterectomy starts menopause.
. If you have a hysterectomy before menopause and you keep your ovaries, you may experience menopause at a younger than average age.
. If you have a partial hysterectomy, your cervix remains in place, so you're still at risk of cervical cancer. You need regular Pap tests to screen for cervical cancer.
Other parts of your life will likely return to normal or perhaps improve once you've recovered from your hysterectomy. For example:
. If you had a good sex life before a hysterectomy, chances are you'll maintain it afterward. Some women even experience more sexual pleasure after a hysterectomy. This may be due to relief from the chronic pain or heavy bleeding that was caused by a uterine problem.
. The relief of symptoms may greatly enhance your quality of life. You may have an improved sense of well-being and a chance to get on with your life.
On the other hand, you may feel a sense of loss after hysterectomy. Premenopausal women who must have a hysterectomy to treat gynecologic cancer may experience grief and possibly depression over the loss of fertility. If sadness or negative feelings begin to interfere with your enjoyment of everyday life, talk with your doctor.