Orchiectomy Procedure
Orchiectomy Surgery Procedure
What Is Orchiectomy?
If you've been diagnosed with testicular cancer, your doctor has probably talked to you about orchiectomy, surgery to remove one or both testicles. Testicles, or testes, are the male sex organs that make sperm and the hormone testosterone.
Read more about: Orchiectomy surgery for prostate cancer
Read more about: Vaginoplasty Surgery
Read more about: Gender Reassignment Surgery (Male To Female)
Read more about: Varicocelectomy Surgery
Read more about : Kidney transplant in Iran success story in Iran
Read more about : Cancer treatment success story in Iran
Read more about : Sex reassignment surgery success story
Why orchiectomy is done?
It's usually needed to treat testicular cancer. But it can also help if a testicle is damaged by infection or injury. Sometimes it's part of prostate cancer treatment.
If doctors suspect testicular cancer, they will likely order an ultrasound test first to check for non-cancer causes. Blood tests may also be ordered to help diagnose testicular cancer.
Rather than doing a biopsy of the testes, which can trigger cancer spread, doctors almost always do what’s called a radical inguinal orchiectomy. It's called "radical" because it removes the spermatic cord along with the testicle and tumor. The cord has blood and lymph vessels that could let the cancer spread to other parts of the body.
In a simple orchiectomy, the doctor only removes one or both testicles. This surgery can ease symptoms, prevent problems from prostate cancer, and treat male breast cancer.
An orchiectomy may be used to treat some cases of:
- Testicular and/or prostate cancer.
- Male breast cancer.
- Cancer prevention in men with an undescended testicle after puberty.
- Severe trauma.
- Male-to-female gender reassignment surgery.
Read more about: Orchiectomy surgery time
Different types of orchiectomy:
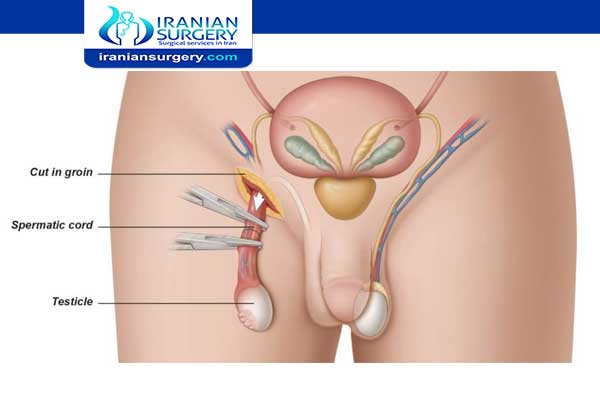
- Radical Inguinal Orchiectomy: The testicle and spermatic cord are removed through an incision made in the groin. At times, a prosthetic saline-filled testicular implant can be inserted.
- Simple Orchiectomy: During a simple orchiectomy, the testicle is removed through the scrotum. As in a radical inguinal orchiectomy, a prosthetic testicle can be inserted. In both simple and radical orchiectomy, a single testicle can be removed, or both testicles, which is called bilateral orchiectomy.
- Subcapsular Orchiectomy: During a subcapsular orchiectomy, the glandular tissue lining the testicles is removed, leaving the testicles in place.
Read more about: Orchiectomy surgery in Iran
Who’s a good candidate for Orchiectomy?
Your doctor may do this surgery to treat breast cancer or prostate cancer. Without the testicles, your body can’t make as much testosterone. Testosterone is a hormone that can cause prostate or breast cancer to spread more quickly. Without testosterone, the cancer may grow at a slower rate, and some symptoms, such as bone pain, may be more bearable.
Your doctor may recommend orchiectomy if you’re in generally good health, and if the cancer cells have not spread beyond your testicles or far beyond your prostate gland.
You may want to do an orchiectomy if you’re transitioning from male to female and want to reduce how much testosterone your body makes.
Read more about: Testicular Biopsy in Iran
Before Orchiectomy
How do I prepare for this procedure?
Before an orchiectomy, your doctor may take blood samples to make sure you’re healthy enough for surgery and to test for any indicators of cancer.
This is an outpatient procedure that takes 30-60 minutes. Your doctor may use either local anesthesia to numb the area or general anesthesia. General anesthesia has more risks but lets you remain unconscious during the surgery.
Before the appointment, be sure that you have a ride home. Take a few days off work and be ready to limit your amount of physical activity after the surgery. Tell your doctor about any medications or dietary supplements that you’re taking.
Read more about: Transplanted testicles
What are the risks associated with an orchiectomy?
As with any surgery, there are risks and possible side effects. These can be:
- Reaction to anesthesia. (Anesthesia is the medication you are given to help you sleep through the surgery, not remember it and to manage pain. Reactions can include wheezing, rash, swelling and low blood pressure.)
- Blood clots.
- Loss of fertility.
- Erectile dysfunction.
- Loss of feeling in the groin and/or genitals.
- Low libido (sex drive).
- Hot flashes, mood swings, depression.
- Loss of muscle mass.
- Breast enlargement (gynecomastia).
- Weight gain.
- Change in self-image.
Is orchiectomy a major surgery?
Orchiectomy surgery is relatively low-risk, and complications are uncommon. But orchiectomy carries all the risks of any major surgery, including: Reactions to anaesthesia or medicines. Infection. You can usually go home later that day but might need to stay in hospital overnight. Your groin and scrotum may be uncomfortable for a week or so and you might need to take mild painkillers. You have your stitches taken out after about a week. Most men can go back to normal activities, including work, after 2 weeks.
Read more about: How is a prosthetic testicle attached
During Orchiectomy surgery
Orchiectomy procedure steps
First, your surgeon will lift your penis and tape it to your abdomen. Then, they’ll make an incision either on your scrotum or the area right above your pubic bone on your lower abdomen. One or both testicles are then cut out from the surrounding tissues and vessels, and removed through the incision.
Your surgeon will use clamps to prevent your spermatic cords from gushing blood. They may put in a prosthetic testicle to replace the one that’s removed. Then, they’ll wash the area with a saline solution and sew the incision shut.
Read more about: One testicle fertility
After Orchiectomy
Orchiectomy recovery
Recovery from an orchiectomy may include a short stay in the hospital, depending on the extent of the procedure you have had. You will be taught incisional care before being discharged from the hospital.
Your medical team will discuss with you the medications you will be taking (blood clot and infection prevention, pain management, nausea management, and constipation prevention.
Your provider will tell you what you should and should not do when you go home. This will often include:
- Wear a scrotal support and use ice packs as directed.
- Take pain medication as prescribed.
- Avoid straining with bowel movements and try to prevent constipation.
- Use a donut cushion when sitting for comfort.
- Do not lift anything heavy until instructed by your provider.
- No sports, jogging or running until you are told it is safe to do so.
Read more about: Prosthetic testicle recovery
How painful is an orchiectomy?
You may have some mild to moderate pain for several days after surgery. You can expect to feel better each day, your groin and scrotum may be uncomfortable for a week or so and you might need to take mild painkillers. You have your stitches taken out after about a week. Most men can go back to normal activities, including work, after 2 weeks.
Read more about: Side effects of having one testicle removed
Does orchiectomy cause impotence?
Contrary to popular belief, removing one testicle does not decrease a male’s sexual drive. A single testicle is sufficient for both fertility and proper hormone production. In addition, removing one testicle does not cause impotence (the loss of the ability to have an erection). However, removing both testicles may affect one’s sex life. Some males choose to have a gel-filled prosthesis implanted in the scrotum to replace the missing testicle, but the majority of males find this to be unnecessary.
Read more about: Disadvantages of having one testicle
What happens after an orchiectomy?
You should be able to do most of your normal activities after 2 to 3 weeks, except for those that require a lot of physical effort. It is important to avoid straining with bowel movements and doing heavy lifting while you are recovering.
If both your testicles were removed, you may start to notice changes in your body several weeks after surgery due to not having male hormones. The most obvious changes may be hot flashes and sweating. You may lose your sex drive, gain weight, or not be able to get an erection. These changes can be upsetting. Talk to your doctor about treatments that might help with these.
Read more about: Does having one testicle affect testosterone
10 common question about Orchiectomy Surgery Procedure
[kkstarratings]


