Transplanted testicles
Can you donate a testicle?
Pros and Cons of Orchiectomy
No testicular transplant has been performed in the world so far but Technically testicle transplant is possible, but it is against Iranian rules and regulation which means that you are not able to have testicle transplant in Iran.
Read more about : Side effects of having one testicle removed
Read more about : What is an orchiectomy?
Read more about : Penile implant
Read more about : Testicular Cancer Treatment
Read more about: Orchiectomy surgery for prostate cancer
Read more about: Hair transplant
Pros and Cons of Orchiectomy
What are the advantages of Orchiectomy?
First, it is a single, simple, surgical procedure with a very low risk of problems and 100 percent efficacy.
Second, it can be carried out in ways which are not physically evident. In other words, it is possible to carry out what is known as a subcapsular orchiectomy, in which the cores of the two testes are removed while the capsules remain in the scrotum. This means that the man still appears to be an “intact” male.
What are the disadvantages of orchiectomy?
The major disadvantage appears to be the psychological one associated with “loss of manhood.” For many men this loss appears to be all but unbearable. Interestingly, the loss of “manhood” is not usually a problem for the partners of most prostate cancer patients when compared to the possibility of loss of life. However, the male association between his theoretical ability to be able to have sexual intercourse and his sense of self-worth appears to be astonishingly strong, regardless of the truth about his actual level of sexual activity and/or capability.
The other disadvantage is that the procedure is not reversible. However, since cases of complete remission of advanced prostate cancer are almost completely unheard of and certainly not well documented, it would appear that the need for reversing this operation is about as close to zero as one can get!
Risks and side effects of orchiectomy
As with any surgery, there are risks and possible side effects. These can be:
. Reaction to anesthesia.
. Bleeding.
. Infection.
. Blood clots.
. Loss of fertility.
. Erectile dysfunction.
. Loss of feeling in the groin and/or genitals.
. Low libido (sex drive).
. Hot flashes, mood swings, depression.
. Loss of muscle mass.
. Osteoporosis.
. Breast enlargement (gynecomastia).
. Weight gain.
. Fatigue.
. Fever over 100°F (37.8°C).
. Inability to urinate.
. Hematoma, which is blood in the scrotum and usually looks like a large purple spot.
. Change in self-image.
Transgender women who undergo an orchiectomy are also likely to experience a number of positive side effects, including:
. A drastic decrease in testosterone, which may allow you to reduce your dose of feminizing hormones
. Reduced gender dysphoria as you take a step closer to matching your physical appearance with your gender identity.
Transplanted testicles
Transplanted testicles will always make the donor's sperm. A veteran of the US Armed Forces has a new penis and scrotum after the most extensive penis transplant yet, Johns Hopkins Hospital announced this week.
Can you get testicle transplant?
Technically a testicle transplant is possible, Cooney a plastic and reconstructive surgery professor at the Johns Hopkins University School of Medicine says, and would allow recipients to forego hormone replacement therapy. But the problem is that the transplanted organ could produce the donor’s genetic offspring. And without the deceased donor’s consent, that poses an ethical complication that Johns Hopkins wanted to avoid from the outset. “If you were to transplant testicles, that would effectively be making the donor not only a donor of body parts, but also a donor of sperm,” says Jeffrey Kahn, director of the Johns Hopkins Berman Institute of Bioethics. “It’s effectively a sperm donation without consent and that shouldn’t happen.”
Read more about Iranian surgery
Transplanted testicles will always make the donor’s sperm.
A veteran of the US Armed Forces has a new penis and scrotum after the most extensive penis transplant yet, Johns Hopkins Hospital announced this week. Not included in the transplant? Testicles because the testicles would continue to make the donor’s sperm in the transplant recipient’s body.
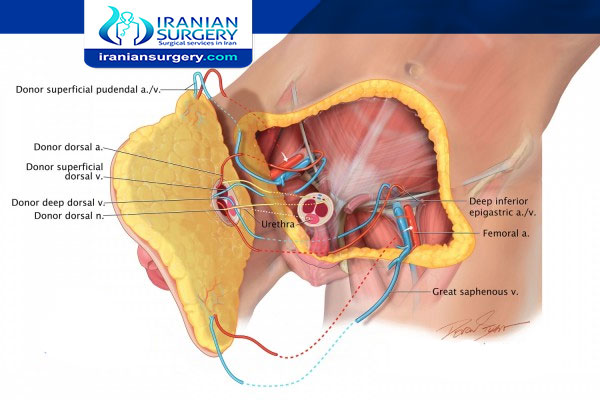
The patient, who asked Johns Hopkins not to reveal his name, suffered a devastating injury to his penis, testicles, part of his lower abdomen, and his legs in Afghanistan when an improvised explosive device blew up, The New York Times reports. A team of 11 surgeons replaced the injured flesh of his genitals and lower abdomen with tissue from a deceased donor during a 14-hour surgery at the end of March, and the patient is recovering well, according to a news briefing on Monday. But the transplant didn’t include testicles something that the Johns Hopkins team decided early on was off the table, says Damon Cooney, a plastic and reconstructive surgery professor at the Johns Hopkins University School of Medicine.
While Cooney couldn’t discuss the particulars of the situation due to confidentiality, he said that generally people who lose their testicles opt to take testosterone to replace the hormones and receive testicular prostheses to restore the appearance. Technically a testicle transplant is possible, Cooney says, and would allow recipients to forego hormone replacement therapy.
But the problem is that the transplanted organ could produce the donor’s genetic offspring. And without the deceased donor’s consent, that poses an ethical complication that Johns Hopkins wanted to avoid from the outset. “If you were to transplant testicles, that would effectively be making the donor not only a donor of body parts, but also a donor of sperm,” says Jeffrey Kahn, director of the Johns Hopkins Berman Institute of Bioethics. “It’s effectively a sperm donation without consent and that shouldn’t happen.”
Read more about Penis transplantation
To understand how that’s possible, it helps to know a little bit about the testicle’s plumbing. Early during an embryo’s development, the germ cells which are basically the cellular grandparents or great grandparents of sperm travel to the nascent gonads. These germ cells then divide to form stem cells that can produce more of themselves, and more of the cells that, through a series of divisions, make sperm. So, even if those testicles are transplanted into a new body, they’ll continue making sperm that carry the donor’s DNA, Michael Eisenberg, a urologist at Stanford University, explains.
“If someone using donated testicles was able to conceive a child, the genetic material would be from the donor,” Cooney says. “You can see why that raises ethical questions.”
Making sure that donors’ expectations align with reality is another reason why testicle transplants are off the table, at least for now. Most people who think of organ donation “think of donating their own tissues,” Cooney says. “They don’t think of donating genetic material that can be used to pass on genes to the next generation.”
Read m
ore about One testicle fertility
The American Society for Reproductive Medicine has clear guidelines about this, explains Valarie Blake, an associate professor of law at West Virginia University. “They basically say don’t take reproductive material from a cadaver unless you have their consent,” she says. If the donor didn’t spell out permission in writing while still alive, the ASRM says that only the surviving spouse or partner can request that the sperm or eggs be harvested after death.
So without the donor’s permission during life, taking his testicles would have been especially appalling, Kahn says. “You’ve made that dead person a sperm donor without their knowing about it, so they could not have consented to it,” he says. “You’d cross a line: it’s not just restoring function sexual and urinary function you’ve granted a person the ability to reproduce, but with someone else’s gonads.



1 Comment
I have only 1 testicle and am considering getting a prosthetic one. Is this a good idea?