Surgery for spinal stenosis
What is the best treatment for spinal stenosis?
What activities should be avoided with spinal stenosis?
What happens if spinal stenosis is left untreated?
Does spinal stenosis go away?
Spinal stenosis treatment
Treatment for spinal stenosis depends on the location of the stenosis and the severity of your signs and symptoms.
Talk to your doctor about the treatment that's best for your situation. If your symptoms are mild or you aren't experiencing any, your doctor may monitor your condition with regular follow-up appointments. He or she may offer some self-care tips that you can do at home. If these don't help, he or she may recommend medications or physical therapy. Surgery may be an option if other treatments haven't helped.
Read more about : Arachnoid cyst size chart
Read more about : Ovarian cyst size chart
Read more about : Arachnoid Cyst Treatment
Read more about: Spinal Compression Fractures treatment
Medical treatment for spinal stenosis
- Taking non-steroidal anti-inflammatory drugs (NSAIDs) for relief.
- Receiving cortisone injections directly into the spinal column to provide short-term relief.
- Engaging in exercise and physical therapy that focuses on strengthening the back and abdominal muscles as well as stretching.
If the above treatment options do not ease the pain and your ability to engage in everyday activities is inhibited, you should consider spine surgery.
Exercises for spinal stenosis
Getting regular exercise or trying physical therapy can help strengthen muscles in the back, arms, and legs, leading to improved flexibility, balance, and mobility.
The American College of Rheumatology recommend a minimum of three 30-minute exercise sessions per week for people with spinal stenosis.
These sessions should incorporate flexion-based exercises, which involve bending the lower back forward.
Once a person has strengthened their back, they may incorporate other gentle activities, such as walking or swimming, into their routine.
Read more about: Herniated Disk Treatment
Read more about: spinal disc herniation treatment
Surgery for spinal stenosis
If these treatments don't work, your doctor may suggest surgery, especially if:
- You're in a lot of pain
- You have trouble walking
- You can't control your bladder
In fact, your doctor may recommend surgery first if you have severe symptoms. Like other treatments, surgery is not a cure, but it can help with pain and function.
Your doctor may talk to you about these types:
- Laminectomy. This is the most common one. A doctor takes out the bone, spurs, and ligaments that are putting pressure on the nerves.
- Spinal fusion. Doctors sometimes do this along with a laminectomy. It involves joining vertebrae together to reduce movement within the spine.
- Foraminotomy. A doctor expands the portion of the vertebrae where the nerve roots branch out to the rest of the body.
Recovery can be a few days or up to 3 months. Surgery helps many people but there are also risks, such as blood clots.
What is the best treatment for spinal stenosis?
There is no cure for spinal stenosis, but there are treatments to help relieve symptoms. Treatment for spinal stenosis depends on the location of the stenosis and the severity of your signs and symptoms.
- carry the risk of serious side effects, including becoming habit forming.
Physical therapy
It's common for people who have spinal stenosis to become less active, in an effort to reduce pain. But that can lead to muscle weakness, which can result in more pain. A physical therapist can teach you exercises that may help:
- Build up your strength and endurance
- Maintain the flexibility and stability of your spine
- Improve your balance
Steroid injections
Your nerve roots may become irritated and swollen at the spots where they are being pinched. While injecting a steroid medication (corticosteroid) into the space around impingement won't fix the stenosis, it can help reduce the inflammation and relieve some of the pain.
Steroid injections don't work for everyone. And repeated steroid injections can weaken nearby bones and connective tissue, so you can only get these injections a few times a year.
Decompression procedure
With this procedure, needle-like instruments are used to remove a portion of a thickened ligament in the back of the spinal column to increase spinal canal space and remove nerve root impingement. Only patients with lumbar spinal stenosis and a thickened ligament are eligible for this type of decompression.
The procedure is called percutaneous image-guided lumbar decompression (PILD). It has also been called minimally invasive lumbar decompression (MILD), but to avoid confusion with minimally invasive surgical procedures, doctors have adopted the term PILD.
Because PILD is performed without general anesthesia, it may be an option for some people with high surgical risks from other medical problems.
Read more about Do arachnoid cysts require surgery?
Read more about Ovarian cyst size chart
Read more about Breast reduction size chart
Read more about Stages of fissure healing
Read more about Endoscopic Brain Surgery
Read more about What we can do for you in Iranian surgery?
Surgery
Surgery may be considered if other treatments haven't helped or if you're disabled by your symptoms. The goals of surgery include relieving the pressure on your spinal cord or nerve roots by creating more space within the spinal canal. Surgery to decompress the area of stenosis is the most definitive way to try to resolve symptoms of spinal stenosis.
Research shows that spine surgeries result in fewer complications when done by highly experienced surgeons. Don't hesitate to ask about your surgeon's experience with spinal stenosis surgery. If you have any doubts, get a second opinion.
Examples of surgical procedures to treat spinal stenosis include:
- Laminectomy. This procedure removes the back part (lamina) of the affected vertebra. A laminectomy is sometimes called decompression surgery because it eases the pressure on the nerves by creating more space around them.
In some cases, that vertebra may need to be linked to adjoining vertebrae with metal hardware and a bone graft (spinal fusion) to maintain the spine's strength.
- Laminotomy. This procedure removes only a portion of the lamina, typically carving a hole just big enough to relieve the pressure in a particular spot.
- Laminoplasty. This procedure is performed only on the vertebrae in the neck (cervical spine). It opens up the space within the spinal canal by creating a hinge on the lamina. Metal hardware bridges the gap in the opened section of the spine.
- Minimally invasive surgery. This approach to surgery removes bone or lamina in a way that reduces the damage to nearby healthy tissue. This results in less need to do fusions.
While fusions are a useful way to stabilize the spine and reduce pain, by avoiding them you can reduce potential risks, such as post-surgical pain and inflammation and disease in nearby sections of the spine. In addition to reducing the need for spinal fusion, a minimally invasive approach to surgery has been shown to result in a shorter recovery time.
In most cases, these space-creating operations help reduce spinal stenosis symptoms. But some people's symptoms stay the same or get worse after surgery. Other surgical risks include infection, a tear in the membrane that covers the spinal cord, a blood clot in a leg vein and neurological deterioration.
Potential future treatments
Clinical trials are underway to test the use of stem cells to treat degenerative spinal disease, an approach sometimes called regenerative medicine. Genomic medicine trials are also being done, which could result in new gene therapies for spinal stenosis.
Alternative medicine
Integrative medicine and alternative therapies may be used with conventional treatments to help you cope with spinal stenosis pain. Examples include:
- Massage therapy
- Chiropractic treatment
- Acupuncture
Read more about: Spinal cord injury
What activities should be avoided with spinal stenosis?
Spinal stenosis exercise to avoid #1 – The Cobra
sciatica exercises for sciatica pain relief
Why this is a spinal stenosis exercise to avoid:
Nine times out of ten, people with spinal stenosis find that walking and standing are painful. Both of these activities are what we call extension exercises. They cause the spine to move in a way called extension, which simply means leaning backwards. Extension movements cause the bony surfaces in the spine to move towards each other and close down narrow spaces even more.
Because of this, they make narrowing within the spine worse. You might find that if you try this action, your pain gets worse immediately, or directly after.
Therefore, lying on your front and pushing up, like in The Cobra exercise, is a spinal stenosis exercise to avoid.
Spinal stenosis exercise to avoid #2 – Standing Extension
sciatica exercises for sciatica pain relief sciatica exercises pictures
Why this is a spinal stenosis exercise to avoid:
This might be the worst exercise someone with spinal stenosis could possibly choose. By leaning back in standing, you’ve got both the weight of the body and the extension movement causing compression on the already narrowed areas in the spine.
If you have spinal stenosis, make sure you don’t use this extension movement in standing.
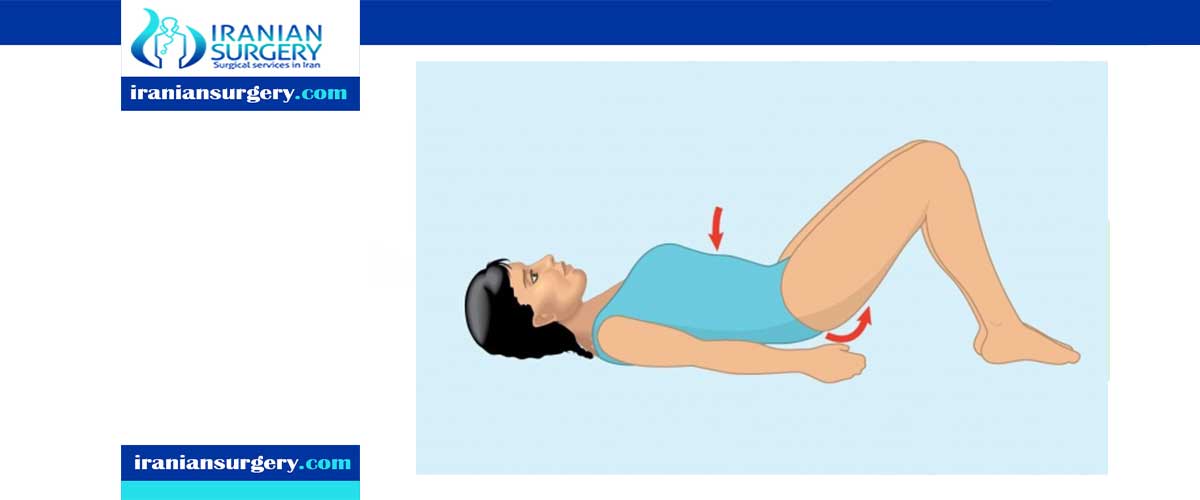
Spinal stenosis exercise to avoid #3 – The Bridge
spinal stenosis exercise to avoid, spinal stenosis treatment
Why this is a spinal stenosis exercise to avoid:
While the bridge is a great exercise for strengthening the gluteals and may be a good exercise for some people with sciatica, the bridge is certainly a spinal stenosis exercise to avoid.
Can you see in the second picture how by bringing the hips off the floor, the spine goes into extension? This movement will cause pain in the lower back as the bony spaces close up. There are far better alternatives for people with spinal stenosis.
Spinal stenosis exercise to avoid #4 – Hip Extension
spinal stenosis exercise to avoid, spinal stenosis treatment
Why this is a spinal stenosis exercise to avoid:
Even though this is a hip exercise, you can see how by lifting a leg off the floor in this position, our spines go into extension. This extension movement will cause pain in the back and leg in someone with this condition and is therefore a spinal stenosis exercise to avoid.
The problem with this exercise is that it is often prescribed for people with hip arthritis, which is common with spinal stenosis.
What happens if spinal stenosis is left untreated?
It can lead to significant and permanent nerve damage including paralysis and death. Symptoms may affect your gait and balance, dexterity, grip strength and bowel or bladder function.
Read more about: Spinal Surgery
Does spinal stenosis go away?
untreated severe spinal stenosis may progress and cause permanent: Numbness. Weakness. Balance problems, if you are living with lumbar spinal stenosis, stop hoping it will just go away. Spinal stenosis is a progressive condition, but symptoms can be improved with the right exercises. It's important to do these exercises and not just use anti-inflammatory medications alone.
10 common questions about spinal stenosis treatment
[kkstarratings]