pancreas cancer treatment
What is Pancreatic Cancer?
Pancreatic cancer begins in the tissues of your pancreas — an organ in your abdomen that lies behind the lower part of your stomach. Your pancreas releases enzymes that aid digestion and produces hormones that help manage your blood sugar.
Several types of growths can occur in the pancreas, including cancerous and noncancerous tumors. The most common type of cancer that forms in the pancreas begins in the cells that line the ducts that carry digestive enzymes out of the pancreas (pancreatic ductal adenocarcinoma).
Pancreatic cancer is seldom detected at its early stages when it's most curable. This is because it often doesn't cause symptoms until after it has spread to other organs.
Read more about : Esophageal cancer treatment
Read more about : Prostate Cancer Treatments Pros and Cons
Read more about : Cancer Treatment
Before Pancreatic Cancer Treatment
Symptoms
Pancreatic cancer often doesn’t show symptoms until it reaches the advanced stages of the disease. For this reason, there typically aren’t any early signs of pancreatic cancer.
Even once the cancer has grown, some of the most common symptoms can be subtle. They include:
. Loss of appetite
. Unintentional weight loss
. Abdominal (stomach) or lower back pain
. Blood clots
. Jaundice (yellow skin and eyes)
. Depression
Pancreatic cancer that spreads may worsen preexisting symptoms. If the cancer spreads, you may experience additional signs and symptoms of advanced pancreatic cancer.
Causes
The cause of pancreatic cancer is unknown. This type of cancer occurs when abnormal cells begin to grow within the pancreas and form tumors.
Normally, healthy cells grow and die in moderate numbers. In the case of cancer, there is an increased amount of abnormal cell production, and these cells eventually take over the healthy cells.
While doctors and researchers don’t know what causes the changes in the cells, they do know some common factors that may increase a person’s risk for developing this type of cancer.
The two most significant risk factors are inherited gene mutations and acquired gene mutations. Genes control the way cells acts, so changes to those genes may lead to cancer.
Pancreatic cancer risk factors
While the cause of this type of cancer is unknown, there are certain risk factors that may increase your chances of developing pancreatic cancer. You may be at an increased risk if you:
. Smoke cigarettes — 30 percent of cancer cases are related to cigarette smoking.
. Are obese
. Don’t exercise regularly
. Eat diets high in fat content
. Drink heavy amounts of alcohol
. Have diabetes
. Work with pesticides and chemicals
. Have chronic inflammation of the pancreas
. Have liver damage
. Are African-American
. Have a family history of pancreatic cancer or certain genetic disorders that have been linked to this type of cancer.
Your DNA has a great influence on your health and the conditions you may develop. You can inherit genes that will increase your risk for pancreatic cancer.
Read more about: cervical cancer risk factors
Diagnosis
If your doctor suspects pancreatic cancer, he or she may have you undergo one or more of the following tests:
. Imaging tests that create pictures of your internal organs. These tests help your doctors visualize your internal organs, including the pancreas. Techniques used to diagnose pancreatic cancer include ultrasound, computerized tomography (CT) scans, magnetic resonance imaging (MRI) and, sometimes, positron emission tomography (PET) scans.
. Using a scope to create ultrasound pictures of your pancreas. An endoscopic ultrasound (EUS) uses an ultrasound device to make images of your pancreas from inside your abdomen. The device is passed through a thin, flexible tube (endoscope) down your esophagus and into your stomach in order to obtain the images.
. Removing a tissue sample for testing (biopsy). A biopsy is a procedure to remove a small sample of tissue for examination under a microscope. Most often the tissue is collected during EUS by passing special tools through the endoscope. Less often, a sample of tissue is collected from the pancreas by inserting a needle through your skin and into your pancreas (fine-needle aspiration).
. Blood test. Your doctor may test your blood for specific proteins (tumor markers) shed by pancreatic cancer cells. One tumor marker test used in pancreatic cancer is called CA19-9. It may be helpful in understanding how the cancer responds to treatment. But the test isn't always reliable because some people with pancreatic cancer don't have elevated CA19-9 levels, making the test less helpful.
If your doctor confirms a diagnosis of pancreatic cancer, he or she tries to determine the extent (stage) of the cancer. Using information from staging tests, your doctor assigns your pancreatic cancer a stage, which helps determine what treatments are most likely to benefit you.
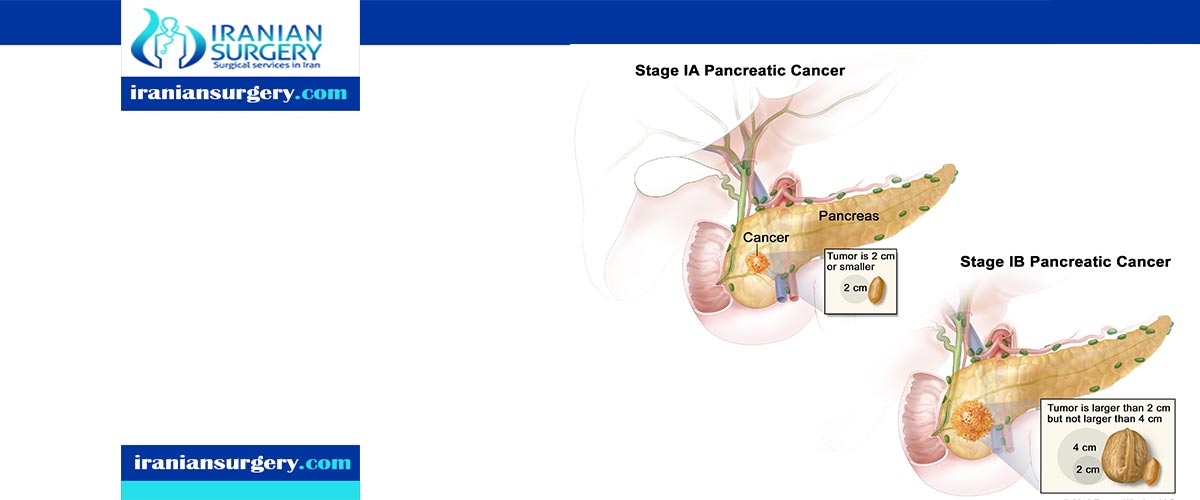
The stages of pancreatic cancer are indicated by Roman numerals ranging from 0 to IV. The lowest stages indicate that the cancer is confined to the pancreas. By stage IV, the cancer has spread to other parts of the body.
The cancer staging system continues to evolve and is becoming more complex as doctors improve cancer diagnosis and treatment.
Don't hesitate to ask your doctor about his or her experience with diagnosing pancreatic cancer. If you have any doubts, get a second opinion.
Complications
As pancreatic cancer progresses, it can cause complications such as:
. Weight loss. A number of factors may cause weight loss in people with pancreatic cancer. Weight loss might happen as the cancer consumes the body's energy. Nausea and vomiting caused by cancer treatments or a tumor pressing on your stomach may make it difficult to eat. Or your body may have difficulty processing nutrients from food because your pancreas isn't making enough digestive juices.
. Jaundice. Pancreatic cancer that blocks the liver's bile duct can cause jaundice. Signs include yellow skin and eyes, dark-colored urine, and pale-colored stools. Jaundice usually occurs without abdominal pain.
Your doctor may recommend that a plastic or metal tube (stent) be placed inside the bile duct to hold it open. This is done with the help of a procedure called endoscopic retrograde cholangiopancreatography (ERCP). During ERCP an endoscope is passed down your throat, through your stomach and into the upper part of your small intestine. A dye is then injected into the pancreatic and bile ducts through a small hollow tube (catheter) that's passed through the endoscope. Finally, images are taken of the ducts.
. Pain. A growing tumor may press on nerves in your abdomen, causing pain that can become severe. Pain medications can help you feel more comfortable. Treatments, such as radiation and chemotherapy, might help slow tumor growth and provide some pain relief.
In severe cases, your doctor might recommend a procedure to inject alcohol into the nerves that control pain in your abdomen (celiac plexus block). This procedure stops the nerves from sending pain signals to your brain.
. Bowel obstruction. Pancreatic cancer that grows into or presses on the first part of the small intestine (duodenum) can block the flow of digested food from your stomach into your intestines.
Your doctor may recommend that a tube (stent) be placed in your small intestine to hold it open. In some situations, it might help to have surgery to place a temporary feeding tube or to attach your stomach to a lower point in your intestines that isn't blocked by cancer.
Read more about: Bone cancer causes
Prevention
You may reduce your risk of pancreatic cancer if you:
. Stop smoking. If you smoke, try to stop. Talk to your doctor about strategies to help you stop, including support groups, medications and nicotine replacement therapy. If you don't smoke, don't start.
. Maintain a healthy weight. If you are at a healthy weight, work to maintain it. If you need to lose weight, aim for a slow, steady weight loss — 1 to 2 pounds (0.5 to 1 kilogram) a week. Combine daily exercise with a diet rich in vegetables, fruit and whole grains with smaller portions to help you lose weight.
. Choose a healthy diet. A diet full of colorful fruits and vegetables and whole grains may help reduce your risk of cancer.
Consider meeting with a genetic counselor if you have a family history of pancreatic cancer. He or she can review your family health history with you and determine whether you might benefit from a genetic test to understand your risk of pancreatic cancer or other cancers.
When to see a doctor
Symptoms of pancreatic cancer often do not appear until the later stages. If you experience jaundice or any other unusual symptoms, you should see a doctor.
If someone in the family has already had pancreatic cancer, or if you have any of the risk factors and are concerned about the possibility of developing it, you should also speak to a doctor. They may suggest screening.
During Pancreatic Cancer Treatment
Pancreatic cancer stages
When pancreatic cancer is discovered, doctors will likely perform additional tests to understand if or where the cancer has spread. Imaging tests, such as a PET scan, help doctors identify the presence of cancerous growths. Blood tests may also be used.
With these tests, doctors are attempting to establish the cancer’s stage. Staging helps explain how advanced the cancer is. It also helps doctors determine treatment options.
Once a diagnosis has been made, your doctor will assign a stage based on the test results:
. Stage 1: tumors exist in the pancreas only
. Stage 2: tumors have spread to nearby abdominal tissues or lymph nodes
. Stage 3: the cancer has spread to major blood vessels and lymph nodes
. Stage 4: tumors have spread to other organs, such as the liver
. Pancreatic cancer stage 4
Stage 4 pancreatic cancer has spread beyond the original site to distant sites, like other organs, the brain, or bones.
Pancreatic cancer is often diagnosed at this late stage because it rarely causes symptoms until it has spread to other sites. Symptoms you might experience at this advanced stage include:
. Pain in the upper abdomen
. Pain in the back
. Fatigue
. Jaundice (yellowing of the skin)
. A loss of appetite
. Weight loss
. Depression
Stage 4 pancreatic cancer cannot be cured, but treatments can relieve symptoms and prevent complications from the cancer. These treatments can include:
. Chemotherapy
. Palliative pain treatments
. Bile duct bypass surgery
. Bile duct stent
. Gastric bypass surgery
The five-year survival rate for stage 4 pancreatic cancer is 3 percent.
. Pancreatic cancer stage 3
Stage 3 pancreatic cancer is a tumor in the pancreas and possibly nearby sites, such as lymph nodes or blood vessels. Pancreatic cancer at this stage has not spread to distant sites.
Pancreatic cancer is called a silent cancer because it is often not diagnosed until it has reached an advanced stage. If you have symptoms of stage 3 pancreatic cancer, you may experience:
. Pain in the back
. Pain or tenderness in the upper abdomen
. A loss of appetite
. Weight loss
. Fatigue
. Depression
Stage 3 pancreatic cancer is difficult to cure, but treatments can help prevent the spread of the cancer and ease symptoms caused by the tumor. These treatments may include:
. Surgery to remove a portion of the pancreas (Whipple procedure)
. Anti-cancer drugs
. Radiation therapy
The five-year survival rate for stage 3 pancreatic cancer is 3 to 12 percent.
The majority of people with this stage of the cancer will have a recurrence. That’s likely due to the fact that micrometastases, or small areas of undetectable cancer growth, have spread beyond the pancreas as the time of detection.
. Pancreatic cancer stage 2
Stage 2 pancreatic cancer is cancer that remains in the pancreas and may have spread to a few nearby lymph nodes. It has not spread to nearby tissues or blood vessels, and it has not spread to sites elsewhere in the body.
Pancreatic cancer is difficult to detect in the early stages, including stage 2. That’s because it’s unlikely to cause detectable symptoms. If you do have symptoms at this early stage, you may experience:
. Jaundice
. Changes in urine color
. Pain or tenderness in the upper abdomen
. Weight loss
. Loss of appetite
. Fatigue
Treatment may include:
. Surgery
. Radiation
. Chemotherapy
. Targeted drug therapies
Your doctor may use a combination of these approaches to help shrink the tumor and prevent possible metastases. The five-year survival rate for people with stage 2 pancreatic cancer is around 30 percent.
Read more about : Herniated disk treatment
Read more about : Cycling after knee arthroscopy
Types pancreatic cancer
There are two different types of pancreatic cancer, depending on whether it affects the exocrine or endocrine functions. They have different risk factors, causes, symptoms, diagnostic tests, treatments, and outlook.
. Exocrine pancreatic cancer
Tumors that affect the exocrine functions are the most common type.
They can be malignant or benign. Benign tumors or cysts are called cystadenomas. Most pancreatic tumors are malignant, or cancerous.
Different types of pancreatic cancers can affect the exocrine functions.
Types of tumor include:
. Adenocarcinomas, which typically start in gland cells in the ducts of the pancreas
. Acinar cell carcinoma, which starts in the pancreatic enzyme cells
. Ampullary cancer, which starts where the bile duct and pancreatic duct meet the duodenum of the small intestine.
. Adenosquamous carcinomas
. Squamous cell carcinomas
. Giant cell carcinomas
. Endocrine pancreatic cancer
Tumors that affect the endocrine functions of the pancreas are called neuroendocrine or islet-cell tumors. These are fairly uncommon.
The name comes from the type of hormone-producing cell where the cancer starts.
They include:
. Insulinomas (insulin)
. Glucagonomas (glucagon)
. Gastrinomas (gastrin)
. Somatostatinomas (somatostatin)
. VIPomas (vasoactive intestinal peptide or VIP)
Functioning islet cell tumors continue to make hormones. Non-functioning ones do not. Most of these tumors are benign, but non-functioning tumors are more likely to be malignant, islet-cell carcinomas.
Treatment
Treatment for pancreatic cancer depends on the stage and location of the cancer as well as on your overall health and personal preferences. For most people, the first goal of pancreatic cancer treatment is to eliminate the cancer, when possible. When that isn't an option, the focus may be on improving your quality of life and limiting the cancer from growing or causing more harm.
Treatment may include surgery, radiation, chemotherapy or a combination of these. When pancreatic cancer is advanced and these treatments aren't likely to offer a benefit, your doctor will focus on symptom relief (palliative care) to keep you as comfortable as possible for as long as possible.
- Surgery
Operations used in people with pancreatic cancer include:
. Surgery for tumors in the pancreatic head. If your cancer is located in the head of the pancreas, you may consider an operation called a Whipple procedure (pancreaticoduodenectomy).
The Whipple procedure is a technically difficult operation to remove the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder, part of the bile duct and nearby lymph nodes. In some situations, part of the stomach and colon may be removed as well. Your surgeon reconnects the remaining parts of your pancreas, stomach and intestines to allow you to digest food.
. Surgery for tumors in the pancreatic body and tail. Surgery to remove the left side (body and tail) of the pancreas is called distal pancreatectomy. Your surgeon may also need to remove your spleen.
. Surgery to remove the entire pancreas. In some people, the entire pancreas may need to be removed. This is called total pancreatectomy. You can live relatively normally without a pancreas but do need lifelong insulin and enzyme replacement.
. Surgery for tumors affecting nearby blood vessels. Many people with advanced pancreatic cancer aren't considered eligible for the Whipple procedure or other pancreatic surgeries if their tumors involve nearby blood vessels. At highly specialized and experienced medical centers, surgeons may offer pancreatic surgery operations that include removing and reconstructing affected blood vessels.
Each of these surgeries carries the risk of bleeding and infection. After surgery some people experience nausea and vomiting if the stomach has difficulty emptying (delayed gastric emptying). Expect a long recovery after any of these procedures. You'll spend several days in the hospital and then recover for several weeks at home.
Extensive research shows pancreatic cancer surgery tends to cause fewer complications when done by highly experienced surgeons at centers that do many of these operations. Don't hesitate to ask about your surgeon's and hospital's experience with pancreatic cancer surgery. If you have any doubts, get a second opinion.
- Chemotherapy
Chemotherapy uses drugs to help kill cancer cells. These drugs can be injected into a vein or taken orally. You may receive one chemotherapy drug or a combination of them.
Chemotherapy can also be combined with radiation therapy (chemoradiation). Chemoradiation is typically used to treat cancer that hasn't spread beyond the pancreas to other organs. At specialized medical centers, this combination may be used before surgery to help shrink the tumor. Sometimes it is used after surgery to reduce the risk that pancreatic cancer may recur.
In people with advanced pancreatic cancer and cancer that has spread to other parts of the body, chemotherapy may be used to control cancer growth, relieve symptoms and prolong survival.
- Radiation therapy
Radiation therapy uses high-energy beams, such as those made from X-rays and protons, to destroy cancer cells. You may receive radiation treatments before or after cancer surgery, often in combination with chemotherapy. Or your doctor may recommend a combination of radiation and chemotherapy treatments when your cancer can't be treated surgically.
Radiation therapy usually comes from a machine that moves around you, directing radiation to specific points on your body (external beam radiation). In specialized medical centers, radiation therapy may be delivered during surgery (intraoperative radiation).
Traditional radiation therapy uses X-rays to treat cancer, but a newer form of radiation using protons is available at some medical centers. In certain situations, proton therapy can be used to treat pancreatic cancer and it may offer fewer side effects compared with standard radiation therapy.
- Clinical trials
Clinical trials are studies to test new treatments, such as systemic therapy, and new approaches to surgery or radiation therapy. If the treatment being studied proves to be safer and more effective than current treatments, it can become the new standard of care.
Clinical trials for pancreatic cancer might give you a chance to try new targeted therapy, chemotherapy drugs, immunotherapy treatments or vaccines.
Clinical trials can't guarantee a cure, and they might have serious or unexpected side effects. On the other hand, cancer clinical trials are closely monitored to ensure they're conducted as safely as possible. And they offer access to treatments that wouldn't otherwise be available to you.
Talk to your doctor about what clinical trials might be appropriate for you.
- Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care is not the same as hospice care or end-of-life care. Palliative care is provided by teams of doctors, nurses, social workers and other specially trained professionals. These teams aim to improve the quality of life for people with cancer and their families.
Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing medical care. It's often used while undergoing aggressive treatments, such as surgery, chemotherapy and radiation therapy.
When palliative care is used along with other appropriate treatments — even soon after the diagnosis — people with cancer may feel better and live longer.
After Pancreatic Cancer Treatment
Pancreatic cancer prognosis
The survival rates for pancreatic cancer have been improving in recent decades. Research and new treatments are expanding the average five-year survival rate for people diagnosed with pancreatic cancer.
However, the disease is still considered difficult to cure. Because pancreatic cancer typically does not cause symptoms until the cancer is in advanced stages, the likelihood the cancer has spread, or metastasized, is high. That make it hard to treat or eliminate the cancer.
Combining alternative measures with traditional medical treatments may help to improve your quality of life. Yoga, meditation, and light exercise might promote a sense of well-being and make you feel better during treatment.
Pancreatic cancer survival rate
A survival rate is a percentage of how many people with the same type and stage of a cancer are still alive after a specific amount of time. This number doesn’t indicate how long people may live. Instead, it helps gauge how successful treatment for a cancer might be.
Many survival rates are given as a five-year percentage. It’s important to keep in mind that survival rates are not definitive. If you have questions about these numbers, talk with your doctor.
The five-year survival rate for localized pancreatic cancer is 34 percent. Localized pancreatic cancer is stages 0, 1, and 2.
The five-year survival rate for regional pancreatic cancer that has spread to nearby structures or lymph nodes is 12 percent. Stages 2B and 3 fall into this category.
Distant pancreatic cancer, or stage 4 cancer that has spread to other sites like the lungs, liver, or bones, has a 3 percent survival rate.
Pancreatic cancer life expectancy
Pancreatic cancer is one of the most deadly forms of cancer — unfortunately, many patients don’t receive a diagnosis until it has spread outside of the pancreas. The five-year survival rate for all stages of pancreatic cancer is 9 percent.
Following all of your doctor’s recommendations can help improve your chances of recovery and survival. You may also consider:
. Pancreatic enzyme supplements to improve digestion
. Pain medications
. Regular follow-up care, even if the cancer is successfully removed
Is complimentary or alternative medicine effective in pancreatic cancer treatment?
Complimentary or alternative medicine is of unclear benefit in pancreatic cancer treatment. No specific complimentary or alternative therapy has been proven beneficial, but many adjunctive treatments have been tried. Compounds such as curcumin, the principle ingredient in turmeric, have shown efficacy in nonhuman research and are being tested in clinical trials in pancreatic cancer.
Given the modest benefit derived from chemotherapy and radiation in this disease, alternative approaches in the treatment of pancreatic cancer in conjunction with (rather than instead of) standard treatment is warranted.
Read more about side effects of having only one testicle
Sources:
https://www.cancer.net/cancer-types/pancreatic-cancer/types-treatment
https://www.cancer.org/cancer/pancreatic-cancer
https://www.mayoclinic.org/diseases-conditions/pancreatic-cancer/diagnosis-treatment/drc-20355427