Balloon Valvuloplasty Surgery
Balloon Valvuloplasty
What is Balloon valvuloplasty?
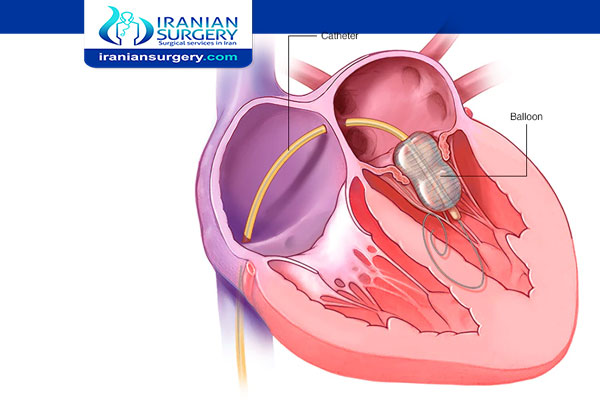
A valvuloplasty, also known as balloon valvuloplasty or balloon valvotomy, is a minimally invasive procedure to repair a heart valve that has a narrowed opening.
The procedure is performed with a thin tube (catheter) that has a small deflated balloon at its tip (balloon-tipped catheter). The catheter is advanced up to the heart and into the opening of the narrowed heart valve. The balloon is inflated to stretch the valve open and relieve the valve obstruction. The procedure is performed in a cardiac catheterization laboratory that has a special x-ray machine and an x-ray monitor.
It is performed on children and adults who have a narrowed heart valve, a condition called stenosis. The goal of the procedure is to improve valve function and blood flow by enlarging the valve opening. It is sometimes used to avoid or delay open heart surgery and valve replacement.
There are four valves in the heart—the aortic valve, pulmonary valve, mitral valve, and tricuspid valve—each at the exit of one of the heart's four chambers. These valves open and close to regulate the blood flow from one chamber to the next and are vital to the efficient functioning of the heart and circulatory system. Narrowing of these valves can be corrected by open heart surgery or at times with balloon valvuloplasty when medical treatment has not corrected or relieved the related problems.
Valvular stenosis can be a congenital defect (develops in the fetus and is present at birth) or can be acquired, that is to stem from other conditions such as rheumatic fever or calcium build up on the valve. Symptoms of valve stenosis may include heart failure, chest pain (angina), irregular heart beat (arrhythmia), or fainting spells (syncope).
Read more about : Heart attack causes
Read more about : Angiogram procedure
Read more about : Echocardiogram
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Cardiac Surgeons and hospitals in Iran. The price of a balloon valvuloplasty surgery in Iran can vary according to each individual’s case and will be determined based on an in-person assessment with the doctor. So if you are looking for the cost of balloon valvuloplasty surgery in Iran, you can contact us and get free consultation from Iranian surgery.

Before Balloon Valvuloplasty
Why it's done
Doctors will examine you and determine if valvuloplasty or another treatment is right for your valve condition.
Your doctor may recommend valvuloplasty if:
. You have severe valve narrowing and are having symptoms
. You have narrowing of the mitral valve (mitral valve stenosis), even if you don't have symptoms.
. You have a narrowed tricuspid or pulmonary valve
. You or your child has a narrowed aortic valve (aortic valve stenosis)
However, the aortic valve tends to narrow again in adults who've had a valvuloplasty, so the procedure is usually done if you are too sick for surgery or are waiting for a valve replacement.
Read more about : Heart pacemaker surgery
Read more about : Closed heart surgery
Read more about : Heart Bypass Surgery
Read more about : Open heart surgery
Before Procedure
How do I get ready for a valvuloplasty?
. Your doctor will explain the procedure to you and ask if you have any questions.
. You will be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if something is unclear.
. Tell your doctor if you have ever had a reaction to any contrast dye, or if you are allergic to iodine.
. Tell your doctor if you are sensitive to or are allergic to any medicines, latex, tape, or anesthetic agents (local and general).
. You will need to fast for a certain period before the procedure. Your doctor will tell you how long to fast, usually overnight.
. If you are pregnant or think you could be, tell your doctor.
. Tell your doctor if you have any body piercings on your chest or abdomen.
. Tell your doctor of all medicines (prescription and over-the-counter) and herbal supplements that you are taking.
. Tell your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medicines, aspirin, or other medicines that affect blood clotting. You may need to stop some of these medicines before the procedure.
. Your doctor may request a blood test before the procedure to determine how long it takes your blood to clot. Other blood tests may be done as well.
. Tell your doctor if you have a pacemaker.
. You may receive a sedative before the procedure to help you relax.
. Based on your medical condition, your doctor may request other specific preparation.
. Plan for your care and recovery after the operation. Allow for time to rest and try to find people to help you with your day-to-day duties.
. If you need a minor pain reliever in the week before surgery, choose acetaminophen rather than aspirin, ibuprofen, or naproxen. This helps avoid extra bleeding during surgery. If you are taking daily aspirin for a medical condition, ask your provider if you need to stop taking it before your surgery.
. Follow your provider's instructions about not smoking before and after the procedure. Smokers heal more slowly after surgery. They are also more likely to have breathing problems during surgery. For these reasons, if you are a smoker, you should quit at least 2 weeks before the procedure. It is best to quit 6 to 8 weeks before surgery.
. Do not eat or drink anything after midnight and the morning before the procedure. Shower and wash your hair with a special anti-infective soap the night before the procedure.
. Follow any other instructions your healthcare provider gives you.
Read more about : How to pop a bartholin cyst yourself?
Read more about : Virgin tightening surgery before and after
Risks
What are the risks for valvuloplasty?
Possible risks of valvuloplasty include:
. Bleeding at the catheter insertion site
. Blood clot or damage to the blood vessel at the insertion site
. Significant blood loss that may require blood transfusion
. Infection at the catheter insertion site
. Abnormal heart rhythms
. Kidney failure
. Stroke
. New or worsening valve regurgitation (leakage)
. Rupture of the valve, requiring open-heart surgery
. The repaired valve may not work as well as planned, or the repair may not last.
. This operation may need to be repeated or you may need to have the valve replaced.
. Depending on your age and the condition of your heart and valve, there is about a 2% to 10% risk of death from this operation.
If you are pregnant or think you could be, tell your healthcare provider due to risk of injury to the fetus from a valvuloplasty. Radiation exposure during pregnancy may lead to birth defects. Also tell your provider if you are lactating, or breastfeeding.
There is a risk of allergic reaction to the dye. If you are allergic or sensitive to medicines, contrast dyes, iodine, or latex should, tell your doctor. If you have kidney failure or other kidney problems, tell your doctor.
Some people may find lying still on the procedure table for the length of the procedure may cause some discomfort or pain.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor before the procedure.
Read more about : Stages of fissure healing
Read more about : General surgery
During Balloon Valvuloplasty
During the procedure
What happens during a valvuloplasty?
A valvuloplasty may be done as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor’s practices.
Generally, a valvuloplasty follows this process:
- Remove any jewelry or other objects that may interfere with the procedure. You may wear your dentures or hearing aids if you use either of these.
- Change into a hospital gown and empty your bladder before the procedure.
- A healthcare professional will start an intravenous (IV) line in your hand or arm to inject medicine or give IV fluids, if needed.
- If there is excessive hair at the catheter insertion site (groin area), it may be shaved off.
- A healthcare professional will connect you to an electrocardiogram (ECG) to monitor and records the electrical activity of the heart. Your vital signs (heart rate, blood pressure, breathing rate, and oxygenation level) will be monitored during the procedure.
- There will be several monitor screens in the room, showing your vital signs, the images of the catheter being moved through the body into the heart, and the structures of the heart as your doctor injects the dye.
- You will get a sedative medicine in your IV before the procedure to help you relax. However, you will likely remain awake during the procedure
- A healthcare professional will check and mark your pulses below the injection site and compare them to pulses after the procedure.
- A local anesthetic will be injected into the skin at the insertion site. You may feel some stinging at the site for a few seconds after the local anesthetic is injected or you will be given a general anesthetic. The drug will relax your muscles and put you in a deep sleep, and keep you from feeling pain during the operation.
- Once the local anesthetic has taken effect, your doctor will insert a sheath, or introducer, into the blood vessel. This is a plastic tube through which the catheter will be inserted into the blood vessel and advanced into the heart.
- Your doctor will insert the valvuloplasty catheter through the sheath into the blood vessel and to the heart.
- Once the catheter is in place, your doctor will inject contrast dye through the catheter into the valve to look at the area. You may feel some effects when the contrast dye is injected into the IV line. These effects include a flushing sensation, a salty or metallic taste in the mouth, or a brief headache. These effects usually last for a few moments.
- Tell the doctor if you feel any breathing difficulties, sweating, numbness, itching, chills, nausea or vomiting, or heart palpitations.
- The doctor will watch the contrast dye injection on a monitor. He or she may ask you to take a deep breath and hold it for a few seconds.
- Once the balloon is in place and has been inflated, you may notice some dizziness or even brief chest discomfort. This should subside when the balloon is deflated. However, if you notice any severe discomfort or pain, such as chest pain, neck or jaw pain, back pain, arm pain, shortness of breath, or breathing difficulty, tell your doctor.
- Your doctor may inflate and deflate the balloon several times to open the valve.
- Once the valve is opened sufficiently, your doctor will remove the catheter. He or she may close the catheter insertion site with a closure device that uses collagen to seal the opening in the artery, by the use of sutures, or by applying manual pressure over the area to keep the blood vessel from bleeding. Your doctor will determine which method is appropriate for your condition.
- If your doctor uses a closure device, he or she will apply a sterile dressing to the site. If manual pressure is used, the doctor (or an assistant) will hold pressure on the insertion site so that a clot will form. Once the bleeding has stopped, a very tight bandage will be placed on the site.
- Your doctor may decide not to remove the sheath, or introducer, from the insertion site for about 4 to 6 hours. This allows the effects of blood-thinning medicine to wear off. You will need to lie flat during this time. If you become uncomfortable in this position, your nurse may give you medicine to make you more comfortable.
- Next, you will be taken to the recovery area. NOTE: If the insertion was in the groin, you will not be allowed to bend your leg for several hours. To help you remember to keep your leg straight, the knee of the affected leg may be covered with a sheet and the ends tucked under the mattress on both sides of the bed to form a type of loose restraint.
Read more about : Rectal bleeding
Read more about : Sleeping position for fissure?
Read more about : Ovarian cyst size chart
After Balloon Valvuloplasty
What happens after the procedure?
You may stay in the hospital for 3 to 7 days, depending on your condition. You will be in an intensive care unit (ICU) or intermediate care unit for several days for observation and monitoring. An electrocardiogram (ECG) will record the rhythm of your heart.
You will have respiratory therapy to prevent any complications in your lungs, such as a collapsed lung, infection, or pneumonia. A nurse or therapist will give the therapy every few hours. It is very important to cooperate and ask for pain medicine if you need it. Therapy may include:
. Deep breathing exercises
. Coughing while holding a pillow against your chest to protect your breastbone
. Chest percussion, which is a gentle slapping on the back to help loosen lung secretions that may have collected your lungs after surgery.
. Moving your legs to lower the chance of blood clots
While in the ICU, you may have the following tubes in your body to help in recovery:
. A breathing tube connected to a ventilator to help you breathe
. A tube through your nose down to your stomach to drain out natural fluids that may cause discomfort when you are not eating.
. A bladder catheter to empty your bladder
. IV tubes in your arms or possibly near your collarbone for fluids, nutrition, and medicines.
. Chest tubes to drain blood from your chest cavity and to help detect any excessive bleeding in your chest.
. An arterial line in your forearm to measure the pressure of the blood flowing through the arteries.
When you have recovered enough, your tubes will be removed and you will go to an intermediate care unit until you are ready to leave the hospital. You will have physical therapy that includes walking around the hospital and other activities. You will be taught how to move your upper arms without hurting your breastbone, and you will keep having respiratory therapy. Occupational therapy will help you learn how to take it easy when you do your daily activities.
Ask your healthcare provider if you should take antibiotics before you have dental work or procedures that involve the rectum, bladder, or vagina. Damaged valves are more likely to become infected by bacteria. Infection of the valve can damage it more and may destroy it. Antibiotics can prevent this.
In the hospital
. You will remain flat in bed for several hours after the procedure. A nurse will monitor your vital signs, the insertion site, and circulation and sensation in the affected leg or arm.
. Tell your nurse right away if you feel any chest pain or tightness, or any other pain, as well as any feelings of warmth, bleeding, or pain at the insertion site in your leg or arm.
. Bed rest may vary from 2 to 6 hours depending on your specific condition. If your doctor placed a closure device, your bed rest may be of shorter duration.
. In some cases, the sheath or introducer may be left in the insertion site. If so, your period of bed rest will be longer. After the sheath is removed, you may be given a light meal.
. You may be given medicine for pain or discomfort related to the insertion site or having to lie flat and still for a prolonged period.
. You will be encouraged to drink water and other fluids to help flush the contrast dye from your body.
. You may feel the urge to urinate often because of the effects of the contrast dye and increased fluids. You will need to use a bedpan or urinal while on bed rest so that you don't bend your affected leg or arm.
. You may resume your usual diet after the procedure, unless your doctor decides otherwise.
. After the specified period of bed rest, you may get out of bed. The nurse will help you the first time you get up, and may check your blood pressure while you are lying in bed, sitting, and standing. Move slowly when getting up from the bed to avoid any dizziness from the long period of bed rest.
At home
. Once at home, watch the insertion site for bleeding, unusual pain, swelling, and discoloration or temperature change at or near the injection site. A small bruise is normal. If you notice a constant or large amount of blood at the site that cannot be contained with a small dressing, call your doctor.
. If your doctor used a closure device for your insertion site, you will be given specific information about how to take care of the insertion site. There will be a small knot, or lump, under the skin at the injection site. This is normal. The knot should gradually disappear over a few weeks.
. It will be important to keep the insertion site clean and dry. Your doctor will give you specific bathing instructions.
. Your doctor may advise you not to participate in any strenuous activities. Your doctor will tell you when you can return to work and resume normal activities.
Tell your doctor to report any of the following:
. Fever or chills
. Increased pain, redness, swelling, or bleeding or other drainage from the insertion site.
. Coolness, numbness or tingling, or other changes in the affected extremity.
. Chest pain or pressure, nausea or vomiting, profuse sweating, dizziness, or fainting.
. Decreased urination
. Swelling of the extremities or abdomen
. Weight gain of over 3 pounds in one day
Your doctor may give you other instructions after the procedure, depending on your particular situation.

