Vaginal Cancer Treatment
What is Vaginal Cancer?
Vaginal cancer is a rare cancer that occurs in your vagina — the muscular tube that connects your uterus with your outer genitals. Vaginal cancer most commonly occurs in the cells that line the surface of your vagina, which is sometimes called the birth canal.
While several types of cancer can spread to your vagina from other places in your body, cancer that begins in your vagina (primary vaginal cancer) is rare.
A diagnosis of early-stage vaginal cancer has the best chance for a cure. Vaginal cancer that spreads beyond the vagina is much more difficult to treat.
Read more about : Cervical Cancer Treatment
Before Vaginal Cancer Treatment
Symptoms
Early vaginal cancer may not cause any signs and symptoms. As it progresses, vaginal cancer may cause signs and symptoms such as:
. Unusual vaginal bleeding, for example, after intercourse or after menopause
. Watery vaginal discharge
. A lump or mass in your vagina
. Painful urination
. Frequent urination
. Constipation
. Pelvic pain
When to see a doctor
See your doctor if you have any signs and symptoms related to vaginal cancer, such as abnormal vaginal bleeding. Since vaginal cancer doesn't always cause signs and symptoms, follow your doctor's recommendations about when you should have routine pelvic exams.
Causes
It's not clear what causes vaginal cancer. In general, cancer begins when healthy cells acquire a genetic mutation that turns normal cells into abnormal cells.
Healthy cells grow and multiply at a set rate, eventually dying at a set time. Cancer cells grow and multiply out of control, and they don't die. The accumulating abnormal cells form a mass (tumor).
Cancer cells invade nearby tissues and can break off from an initial tumor to spread elsewhere in the body (metastasize).
Risk factors
Factors that may increase your risk of vaginal cancer include:
. Increasing age. Your risk of vaginal cancer increases as you age. Most people who are diagnosed with vaginal cancer are older than 60.
. Atypical cells in the vagina called vaginal intraepithelial neoplasia. Being diagnosed with vaginal intraepithelial neoplasia (VAIN) increases your risk of vaginal cancer.
With VAIN, cells in the vagina appear different from normal cells, but not different enough to be considered cancer. A small number of those with VAIN will eventually develop vaginal cancer, though doctors aren't sure what causes some cases to develop into cancer and others to remain benign.
VAIN is frequently caused by the sexually transmitted human papillomavirus (HPV), which can cause cervical, vaginal and vulvar cancers, among others. Vaccines that prevent some types of HPV infection are available.
. Exposure to miscarriage prevention drug. If your mother took a drug called diethylstilbestrol (DES) while pregnant in the 1950s you may have an increased risk of a certain type of vaginal cancer called clear cell adenocarcinoma.
Other risk factors that have been linked to an increased risk of vaginal cancer include:
. Multiple sexual partners
. Early age at first intercourse
. Smoking
. HIV infection
Complications
Vaginal cancer may spread (metastasize) to distant areas of your body, such as your lungs, liver and bones.
Prevention
There is no sure way to prevent vaginal cancer. However, you may reduce your risk if you:
. Undergo regular pelvic exams and Pap tests. You can increase the chance that vaginal cancer is discovered early by having routine pelvic exams and Pap tests. When discovered in its earliest stages, vaginal cancer is more likely to be cured. Discuss with your doctor when to begin these tests and how often to repeat them.
. Ask your doctor about the HPV vaccine. Receiving a vaccination to prevent HPV infection may reduce your risk of vaginal cancer and other HPV-related cancers. Ask your doctor whether an HPV vaccine is appropriate for you.
. Don't smoke. If you smoke, quit. If you don't smoke, don't start. Smoking increases the risk of vaginal cancer.
Read more about : Cystoscopy for female
Read more about : Risk factors of cervical cancer
Diagnosis
Screening for vaginal cancer
Vaginal cancer is sometimes found during a routine pelvic exam before signs and symptoms become evident.
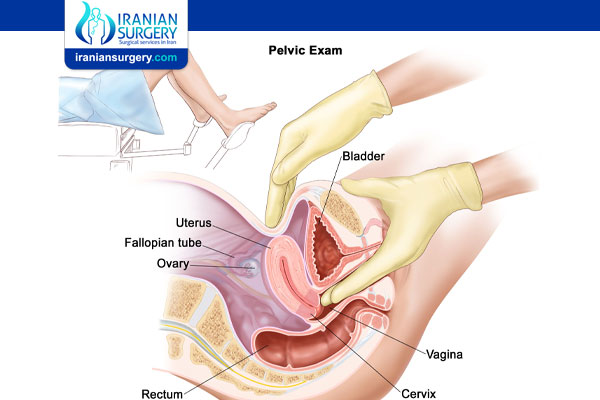
During a pelvic exam, your doctor carefully inspects the outer genitals, and then inserts two fingers of one hand into your vagina and simultaneously presses the other hand on your abdomen to feel your uterus and ovaries. He or she also inserts a device called a speculum into your vagina. The speculum opens your vaginal canal so that your doctor can check your vagina and cervix for abnormalities.
Your doctor may also do a Pap test. Pap tests are usually used to screen for cervical cancer, but sometimes vaginal cancer cells can be detected on a Pap test.
How often you undergo these screenings depends on your risk factors for cancer and whether you've had abnormal Pap tests in the past. Talk to your doctor about how often you should have these health screenings.
Tests to diagnose vaginal cancer
Your doctor may conduct a pelvic exam and Pap test to check for abnormalities that may indicate vaginal cancer. Based on those findings, your doctor may conduct other procedures to determine whether you have vaginal cancer, such as:
. Inspecting the vagina with a magnifying instrument. Colposcopy is an examination of your vagina with a special lighted magnifying instrument called a colposcope. Colposcopy allows your doctor to magnify the surface of your vagina to see any areas of abnormal cells.
. Removing a sample of vaginal tissue for testing. Biopsy is a procedure to remove a sample of suspicious tissue to test for cancer cells. Your doctor may take a biopsy of tissue during a colposcopy exam. Your doctor sends the tissue sample to a laboratory for testing.
Staging
Once your doctor diagnoses vaginal cancer, steps will be taken to determine the extent of the cancer — a process called staging. The stage of your cancer helps your doctor decide what treatments are appropriate for you. In order to determine the stage of your cancer, your doctor may use:
. Imaging tests. Your doctor may order imaging tests to determine whether cancer has spread. Imaging tests may include X-rays, computerized tomography (CT) scans, magnetic resonance imaging (MRI) or positron emission tomography (PET).
. Tiny cameras to see inside your body. Procedures that use tiny cameras to see inside your body may help your doctor determine whether cancer has spread to certain areas. Cameras help your doctor see inside your bladder (cystoscopy) and your rectum (proctoscopy).
During Vaginal Cancer Treatment
Vaginal cancer stages
Vaginal cancer stages tell you how far the cancer has spread. There are four main stages, plus one precancerous stage of vaginal cancer:
. Vaginal intraepithelial neoplasia (VAIN). VAIN is a type of precancer. There are abnormal cells in the vaginal lining, but they’re not growing or spreading yet. VAIN isn’t cancer.
. Stage 1. Cancer is only in the vaginal wall.
. Stage 2. Cancer has spread to the tissue next to the vagina but hasn’t yet spread to the pelvic wall.
. Stage 3. Cancer has spread further into the pelvis and pelvic wall. It might’ve also spread to nearby lymph nodes.
. Stage 4. Stage 4 is divided into two substages:
. In stage 4A, cancer has spread to the bladder, rectum, or both.
. In stage 4B, cancer has spread further throughout the body to organs, such as the lungs, liver, or more distant lymph nodes.
Types of vaginal cancer
Vaginal cancer is divided into different types based on the type of cell where the cancer began. Vaginal cancer types include:
. Vaginal squamous cell carcinoma, which begins in the thin, flat cells (squamous cells) that line the surface of the vagina, and is the most common type.
. Vaginal adenocarcinoma, which begins in the glandular cells on the surface of your vagina.
. Vaginal melanoma, which develops in the pigment-producing cells (melanocytes) of your vagina.
. Vaginal sarcoma, which develops in the connective tissue cells or muscles cells in the walls of your vagina.
Treatment
Your treatment options for vaginal cancer depend on several factors, including the type of vaginal cancer you have and its stage. You and your doctor work together to determine what treatments are best for you based on your goals of treatment and the side effects you're willing to endure. Treatment for vaginal cancer typically includes surgery and radiation.
Surgery
Types of surgery that may be used to treat vaginal cancer include:
. Removal of small tumors or lesions. Cancer limited to the surface of your vagina may be cut away, along with a small margin of surrounding healthy tissue to ensure that all of the cancer cells have been removed.
. Removal of the vagina (vaginectomy). Removing part of your vagina (partial vaginectomy) or your entire vagina (radical vaginectomy) may be necessary to remove all of the cancer. Depending on the extent of your cancer, your surgeon may recommend surgery to remove your uterus and ovaries (hysterectomy) and nearby lymph nodes (lymphadenectomy) at the same time as your vaginectomy.
. Removal of the majority of the pelvic organs (pelvic exenteration). This extensive surgery may be an option if cancer has spread throughout your pelvic area or if your vaginal cancer has recurred.
During pelvic exenteration, the surgeon may remove many of the organs in your pelvic area, including your bladder, ovaries, uterus, vagina, rectum and the lower portion of your colon. Openings are created in your abdomen to allow urine (urostomy) and waste (colostomy) to exit your body and collect in ostomy bags.
If your vagina is completely removed, you may choose to undergo surgery to construct a new vagina. Surgeons use pieces of skin, sections of intestine or flaps of muscle from other areas of your body to form a new vagina.
With some adjustments, a reconstructed vagina allows you to have vaginal intercourse. However, a reconstructed vagina isn't the same as your own vagina. For instance, a reconstructed vagina lacks natural lubrication and creates a different sensation when touched due to changes in surrounding nerves.
Radiation therapy
Radiation therapy uses high-powered energy beams, such as X-rays, to kill cancer cells. Radiation can be delivered two ways:
. External radiation. External beam radiation is directed at your entire abdomen or just your pelvis, depending on the extent of your cancer. During external beam radiation, you're positioned on a table and a large radiation machine is maneuvered around you in order to target the treatment area. Most women with vaginal cancer receive external beam radiation.
. Internal radiation. During internal radiation (brachytherapy), radioactive devices — seeds, wires, cylinders or other materials — are placed in your vagina or the surrounding tissue. After a set amount of time, the devices may be removed. Those with very early-stage vaginal cancer may receive internal radiation only. Others may receive internal radiation after undergoing external radiation.
Radiation therapy kills quickly growing cancer cells, but it may also damage nearby healthy cells, causing side effects. Side effects of radiation depend on the radiation's intensity and where it's aimed.
Other options
If surgery and radiation can't control your cancer, you may be offered other treatments, including:
. Chemotherapy. Chemotherapy uses chemicals to kill cancer cells. It isn't clear whether chemotherapy is useful for treating vaginal cancer. For this reason, chemotherapy generally isn't used on its own to treat vaginal cancer. Chemotherapy may be used during radiation therapy to enhance the effectiveness of radiation.
. Clinical trials. Clinical trials are experiments to test new treatment methods. While a clinical trial gives you a chance to try the latest treatment advances, a cure isn't guaranteed. Discuss available clinical trials with your doctor to better understand your options, or contact the National Cancer Institute or the American Cancer Society to find out what clinical trials might be available to you.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
After Vaginal Cancer Treatment
What to expect after surgery
. Recovery time
Your recovery time will depend on your age, the type of surgery you had and your general health. If only a small amount of tissue is removed, the wound will heal quickly and you can go home in a day or two. If your lymph nodes are removed or the surgery is more extensive, recovery will take longer. You may spend up to a week in hospital.
. Having pain relief
After an operation it is common to feel some pain, but this can be controlled. You will be given pain medicine as a tablet, through a drip into a vein (intravenously), through a drip into a space around the spinal cord (epidural), or through a button you press to give yourself a measured dose of pain relief (patient-controlled analgesia or PCA). After you go home, you can continue taking pain-relieving tablets as needed.
. Bowel issues
Strong pain medicines and long periods in bed can make bowel motions difficult to pass (constipation). Avoid straining when having a bowel movement. Talk to your treatment team about taking laxatives if needed.
. Stitches
Your doctor will tell you how soon you can sit up and walk after surgery. With vaginal surgery, the stitches are all on the inside and will dissolve on their own. You need to avoid straining with bowel movements or lifting heavy objects.
. Vaginal bleeding
You can expect some light vaginal bleeding, which should stop within two weeks. Use a pad instead of tampons.
Infection is a risk – report any fever, redness, pain, swelling, heavy bleeding, wound discharge or unusual smell to your surgeon or nurse.
. Tubes and drains
You may have a tube called a catheter to drain urine from your bladder. This helps keep your wound clean and dry. It will be removed before you leave hospital. There may also be a surgical drain to draw fluid away from the wound. You may go home with the drain in place if there is still fluid coming out. Community nurses can help you manage the care of the drain at home until it is removed.
. What to wear
While you are in bed, you may need to wear compression stockings and have blood-thinning injections to prevent blood clots forming in your legs. Wear loose-fitting clothing and avoid underwear so your wound can air.
Do not put anything into your vagina after surgery until your doctor says the area is healed (usually 6–8 weeks). This includes using tampons and having sex.
Taking care of yourself at home after surgery
When you return home from hospital after surgery for vaginal cancer, there will be a period of recovery and adjustment.
. Rest
You will need to take things easy and get plenty of rest in the first week. Avoid sitting for long periods of time if it is uncomfortable, or try sitting on a pillow or doughnut cushion.
. Exercise
Check with your gynaecological oncologist or nurse about when you can start doing your regular activities. You may not be able to lift anything heavy, but gentle exercise such as walking can help speed up recovery. Because of the risk of infection, avoid swimming until your doctor says you can.
. Emotions
If you have lost part of your genital area, you may feel a sense of loss and grief. It may help to talk about how you are feeling with someone you trust.
. Sex
Sexual intercourse needs to be avoided for about 6–8 weeks after surgery. Ask your doctor when you can have sexual intercourse again, and explore other ways you and your partner can be intimate. You may feel concerned about the impact on your sex life after surgery.
. Using the toilet
If the opening to your urethra is affected, you may find that going to the toilet is different. The urine stream might spray in different directions or go to one side.
. Driving
You will need to avoid driving after the surgery until your wounds have healed and you are no longer in pain. Discuss this issue with your doctor.
Outlook for people with vaginal cancer
Overall, the American Cancer Society estimates vaginal cancer has a five-year survival rate of 47 percent. Survival rates differ greatly by stage. For stage 1 cancers, there’s a five-year survival rate of 75 percent. Stage 4 has a survival rate of 15 to 50 percent. Survival rates also depend on how far the cancer has spread and where it has spread to.
Certain factors can affect survival rate, too. For example, women over 60 have lower survival rates. Women with symptomatic vaginal cancer upon diagnosis and those with tumors in the middle or the lower third of the vagina also have lower survival rates.