What are stem cells and why are they important?
How do stem cells work?
What are the 2 major types of stem cells?
What are stem cells used for?
How do you obtain stem cells?
What are the 5 different types of stem cells?
What are the four different types of stem cells?
A stem cell or bone marrow transplant replaces damaged blood cells with healthy ones. It can be used to treat conditions affecting the blood cells, such as leukaemia and lymphoma.
Stem cells are special cells produced by bone marrow (a spongy tissue found in the centre of some bones) that can turn into different types of blood cells.
The 3 main types of blood cell they can become are:
red blood cells – which carry oxygen around the body
white blood cells – which help fight infection
platelets – which help stop bleeding
A stem cell transplant involves destroying any unhealthy blood cells and replacing them with stem cells removed from the blood or bone marrow.
Read more about : What are the signs of a transplanted kidney being rejected?
Read more about : Heart transplant in Iran
Read more about : Pancreatic cancer
Read more about : Prostate Cancer Treatments Pros and Cons
What are stem cells and why are they important?
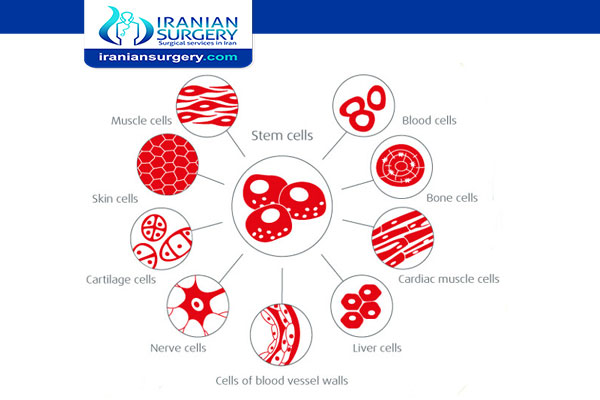
Stem cells are cells that have the potential to develop into many different or specialized cell types. Stem cells can be thought of as primitive, "unspecialized" cells that are able to divide and become specialized cells of the body such as liver cells, muscle cells, blood cells, and other cells with specific functions. Stem cells are referred to as "undifferentiated" cells because they have not yet committed to a developmental path that will form a specific tissue or organ. The process of changing into a specific cell type is known as differentiation. In some areas of the body, stem cells divide regularly to renew and repair the existing tissue. The bone marrow and gastrointestinal tract are examples of areas in which stem cells function to renew and repair tissue.
Stem cell therapies benefits
- Reverse inflammation
- Regulate the immune system
- Re-establish cell-to-cell communication
- Replace damaged cells
- Regenerate normal blood flow
Read more about: Blood transfusion
Read more about: Teeth cleaning in iran
Read more about: Stomach Cancer Surgery
How do stem cells work?
Treatment with stem cells involves the injection of a stem cell rich biocompatible matrix into a targeted area where inflammation or damaged tissue is leading to symptoms affecting daily quality of life. There is no risk of rejection or reaction when using the body’s own stem cells, which almost immediately begin to seek out and address cell damage that has been the result of a certain condition, disease or injury. Your stem cells are “attracted” to inflammation, cell damage and scar tissue and will work to reverse these issues, providing natural healing that is permanent.
An important distinction needs to be made between the stem cells we use for treatment and the controversial use of embryonic stem cells. Therapies being developed today are based on the harvest and targeted injection of a patient’s own stem cells. This is accomplished by extracting stem cells from a patient’s fat tissue, where they are often stored but not used.
Read more about: Nose surgery in Iran
Read more about: abdominoplasty in iran
Read more about: IUI Process In Iran
What are the 2 major types of stem cells?
Stem cells are divided into 2 main forms. They are embryonic stem cells and adult stem cells.
Embryonic stem cells. The embryonic stem cells used in research today come from unused embryos. These result from an in vitro fertilization procedure. They are donated to science. These embryonic stem cells are pluripotent. This means that they can turn into more than one type of cell.
Adult stem cells. There are 2 types of adult stem cells. One type comes from fully developed tissues such as the brain, skin, and bone marrow. There are only small numbers of stem cells in these tissues. They are more likely to generate only certain types of cells. For example, a stem cell that comes from the liver will only make more liver cells.
The second type is induced pluripotent stem cells. These are adult stem cells that have been changed in a lab to be more like embryonic stem cells. Scientists first reported that human stem cells could be changed in this way in 2006. Induced pluripotent stem cells don't seem to be different from embryonic stem cells, but scientists have not yet found one that can develop every kind of cell and tissue.
Read more about: Squamous cell carcinoma
Read more about: Liposuction in Iran
Read more about: GIFT Infertility In Iran
What are stem cells used for?
In stem cell transplants, stem cells replace cells damaged by chemotherapy or disease or serve as a way for the donor's immune system to fight some types of cancer and blood-related diseases, such as leukemia, lymphoma, neuroblastoma and multiple myeloma. These transplants use adult stem cells or umbilical cord blood.
Researchers are testing adult stem cells to treat other conditions, including a number of degenerative diseases such as heart failure. Transplants can also be carried out to replace blood cells that are damaged or destroyed as a result of intensive cancer treatment.
Conditions that stem cell transplants can be used to treat include:
severe aplastic anaemia (bone marrow failure)
leukaemia – a type of cancer affecting white blood cells
lymphoma – another type of cancer affecting white blood cells
myeloma – cancer affecting cells called plasma cells
certain blood, immune system and metabolic disorders – examples include sickle cell anaemia, thalassaemia, severe combined immunodeficiency (SCID) and Hurler syndrome.
Read more about: Strabismus surgery in iran
Read more about: breast lift(Mastopexy)
How do you obtain stem cells?
1) From the body itself:
Adult stem cells can be isolated from the body in different ways, depending on the tissue. Blood stem cells, for example, can be taken from a donor’s bone marrow, from blood in the umbilical cord when a baby is born, or from a person’s circulating blood. Mesenchymal stem cells, which can make bone, cartilage, fat, fibrous connective tissue, and cells that support the formation of blood can also be isolated from bone marrow. Neural stem cells (which form the brain’s three major cell types) have been isolated from the brain and spinal cord.
2) From amniotic fluid:
Amniotic fluid, which bathes the fetus in the womb, contains fetal cells including mesenchymal stem cells, which are able to make a variety of tissues. Many pregnant women elect to have amniotic fluid drawn to test for chromosome defects, the procedure known as amniocentesis
3) From pluripotent stem cells:
Because embryonic stem cells and induced pluripotent cells (iPS cells), which are functionally similar, are able to create all types of cells and tissues, scientists at Children’s and elsewhere hope to use them to produce many different kinds of adult stem cells. Laboratories around the world are testing different chemical and mechanical factors that might prod embryonic stem cells or iPS cells into forming a particular kind of adult stem cell. Adult stem cells made in this fashion would potentially match the patient genetically, eliminating both the problem of tissue rejection and the need for toxic therapies to suppress the immune system.
4) From other adult stem cells:
A number of research groups have reported that certain kinds of adult stem cells can transform, or differentiate, into apparently unrelated cell types (such as brain stem cells that differentiate into blood cells or blood-forming cells that differentiate into cardiac muscle cells). This phenomenon, called transdifferentiation, has been reported in some animals. However, it’s still far from clear how versatile adult stem cells really are, whether transdifferentiation can occur in human cells, or whether it could be made to happen reliably in the lab.
What are the 5 different types of stem cells?
- Hematopoietic Stem Cells (Blood Stem Cells)
- Mesenchymal Stem Cells
- Neural Stem Cells
- Epithelial Stem Cells
- Skin Stem Cells
What are the four different types of stem cells?
- Embryonic stem cells
- Tissue-specific stem cells
- Mesenchymal stem cells
- Induced pluripotent stem cells
Embryonic stem cells
Embryonic stem cells are obtained from the inner cell mass of the blastocyst, a mainly hollow ball of cells that, in the human, forms three to five days after an egg cell is fertilized by a sperm. A human blastocyst is about the size of the dot above this “i.”
In normal development, the cells inside the inner cell mass will give rise to the more specialized cells that give rise to the entire body all of our tissues and organs. However, when scientists extract the inner cell mass and grow these cells in special laboratory conditions, they retain the properties of embryonic stem cells.
Embryonic stem cells are pluripotent, meaning they can give rise to every cell type in the fully formed body, but not the placenta and umbilical cord. These cells are incredibly valuable because they provide a renewable resource for studying normal development and disease, and for testing drugs and other therapies. Human embryonic stem cells have been derived primarily from blastocysts created by in vitro fertilization (IVF) for assisted reproduction that were no longer needed.
Tissue-specific stem cells
Tissue-specific stem cells (also referred to as somatic or adult stem cells) are more specialized than embryonic stem cells. Typically, these stem cells can generate different cell types for the specific tissue or organ in which they live.
For example, blood-forming (or hematopoietic) stem cells in the bone marrow can give rise to red blood cells, white blood cells and platelets. However, blood-forming stem cells don’t generate liver or lung or brain cells, and stem cells in other tissues and organs don’t generate red or white blood cells or platelets.
Some tissues and organs within your body contain small caches of tissue-specific stem cells whose job it is to replace cells from that tissue that are lost in normal day-to-day living or in injury, such as those in your skin, blood, and the lining of your gut.
Tissue-specific stem cells can be difficult to find in the human body, and they don’t seem to self-renew in culture as easily as embryonic stem cells do. However, study of these cells has increased our general knowledge about normal development, what changes in aging, and what happens with injury and disease.
Read more about: Blood transfusion
Read more about: Intralase Lasik in Iran
Read more about: Laparotomy Surgery In Iran


4 Comments
Buenas tardes compis.
Me llamo jose de España de 34 años y Bombero de profesion,he sufrido una lesion medular y estoy buscando sin Exito Clinica en Iran donde hagan el tratamiento con Celulas Madres Schwann,hay un articulo que habeis publicado como en muchos sitios mas pero no encuentro informacion sobre la clinica donde se puede hacer el tratamiento.
Me podeis ayudar PorFavor¿
Me podeis localizar la clinica donde se hace el tratamiento de Celulas Madres Schwann y pasadme contacto Email y Telefonico para poder ir hacer el tratamiento que lo necesito.
espero que me podais ayudar porfavor¡
espero pronto vuestra repsuesta y la info si la podeis conseguir,para pode ir cuanto antes a hacer el tratamiento y no perder mas tiempo.
Graciasssssss
hello
please get in touch with us through whatsApp to provide you with enough information.
Need to refer patients for stem cell transplant
hello dear dr Faswala, would you please send your patient’s medical documents on whatsApp, this is my whatsApp number +989019290946. thank you