Spinal Stenosis
What is Spinal Stenosis?
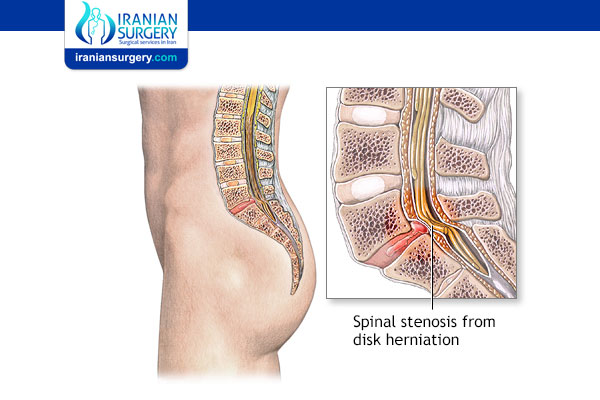
Spinal stenosis is the narrowing of one or more spaces within your spine. Less space within your spine reduces the amount of space available for your spinal cord and nerves that branch off your spinal cord. A tightened space can cause the spinal cord or nerves to become irritated, compressed or pinched, which can lead to back pain and sciatica.
Spinal stenosis usually develops slowly over time. It is most commonly caused by osteoarthritis or “wear-and-tear” changes that naturally occur in your spine as you age. For this reason, you may not have any symptoms for a long time even though some changes might be seen on X-rays or other imaging tests if taken for another reason. Depending on where and how severe your spinal stenosis is, you might feel pain, numbing, tingling and/or weakness in your neck, back, arms, legs, hands or feet.
Before Spinal Stenosis Treatment
Where does spinal stenosis occur?
Spinal stenosis can occur anywhere along the spine but most commonly occurs in two areas:
. Lower back (lumbar canal stenosis).
. Neck (cervical spinal stenosis).
What is lumbar canal stenosis?
Lumbar canal stenosis is the narrowing of the spinal canal or the tunnels through which nerves and other structures communicate with that canal. Narrowing of the spinal canal usually occurs due to changes associated with aging that decrease the size of the canal, including the movement of one of the vertebrae out of alignment.
The narrowing of the spinal canal or the side canals that protect the nerves often results in a pinching of the nerve root of the spinal cord. The nerves become increasingly irritated as the diameter of the canal becomes narrower.
Symptoms of lumbar canal stenosis include pain, numbness or weakness in the legs, groin, hips, buttocks, and lower back. Symptoms usually worsen when walking or standing and might decrease when lying down, sitting, or leaning slightly forward.
Who gets spinal stenosis?
Spinal stenosis can develop in anyone but is most common in men and women over the age of 50. Younger people who are born with a narrow spinal canal can also have spinal stenosis. Other conditions that affect the spine, such as scoliosis, or injury to the spine can put you at risk for developing spinal stenosis.
What are the parts of the spine?
Your spine (or backbone) is a stack or column of 24 bones (vertebrae) plus the fused bones of the sacrum and coccyx. It begins at the base of your skull and ends at your pelvis. Your spine supports your body’s weight and protects your spinal cord. Each vertebrae has a round front portion (the body), a central ring-shaped opening (the spinal canal), flat bony areas (facet joints) where one vertebrae comes into contact with others above and below it, and bone sections along the sides (transverse processes) and back (laminae). Part of the lamina called the spinous process is the ridge you feel when you run your hand down your back. Between each vertebrae body is a flat, round pad called an intervertebral disk that serves as a cushion or shock absorber. Ligaments are strong fiber bands that hold the vertebrae together, keep the spine stable and protect the disks.
The spinal cord – the body’s “master cable cord” that sends and receives messages between the body (including muscles and organs) and the brain – runs through the center of the spinal canal. It is completely surrounded by the bony parts of the spine. Nerves roots are the initial segment of a bundle of nerve fibers that come off the spinal cord and exit the spinal column through side spaces between the vertebrae called the neural foramen. The nerve fibers or “nerves” (the “mini cable network”) then go out to all parts of the body.
Symptoms and Causes
What causes spinal stenosis?
Spinal stenosis has many causes. What they share in common is that they change the structure of the spine, causing a narrowing of the space around your spinal cord and nerves roots that exit through the spine. The spinal cord and/or nerve roots become compressed or pinched, which causes symptoms, such as low back pain and sciatica.
The causes of spinal stenosis include:
. Bone overgrowth/arthritic spurs: Osteoarthritis is the “wear and tear” condition that breaks down cartilage in your joints, including your spine. Cartilage is the protective covering of joints. As cartilage wears away, the bones begin to rub against each other. Your body responds by growing new bone. Bone spurs, or an overgrowth of bone, commonly occurs. Bone spurs on the vertebrae extend into the spinal canal, narrowing the space and pinching nerves in the spine. Paget’s disease of the bone also can also cause on overgrowth of bone in the spine, compressing the nerves.
. Bulging disks/herniated disk: Between each vertebrae is a flat, round cushioning pad (vertebral disk) that acts as shock absorbers along the spine. Age-related drying out and flattening of vertebral disks and cracking in the outer edge of the disks cause the gel-like center of these disks to break through a weak or torn outer layer. The bulging disk then press on the nerves near the disk.
. Thickened ligaments: Ligaments are the fiber bands that hold the spine together. Arthritis can cause ligaments to thicken over time and bulge into the spinal canal space.
. Spinal fractures and injuries: Broken or dislocated bones and inflammation from damage occurring near the spine can narrow the canal space and/or put pressure on spinal nerves.
. Spinal cord cysts or tumors: Growths within the spinal cord or between the spinal cord and vertebrae can narrow the space and put pressure on the spinal cord and its nerves.
. Congenital spinal stenosis: This is a condition in which a person is born with a small spinal canal. Another congenital spinal deformity that can put a person at risk for spinal stenosis is scoliosis (an abnormally shaped spine).
What are the symptoms of spinal stenosis?
You may or may not have symptoms when spinal stenosis first develops. The narrowing of the spinal canal is usually a slow process and worsens over time. Although spinal stenosis can happen anywhere along the spinal column, the lower back (number one most common area) and neck are common areas. Symptoms vary from person to person and may come and go.
Symptoms of lower back (lumbar) spinal stenosis include:
. Pain in the lower back. Pain is sometimes described as dull ache or tenderness to electric-like or burning sensation. Pain can come and go.
. Sciatica. This is pain that begins in the buttocks and extends down the leg and may continue into your foot.
. A heavy feeling in the legs, which may lead to cramping in one or both legs.
. Numbness or tingling (“pins and needles”) in the buttocks, leg or foot.
. Weakness in the leg or foot (as the stenosis worsens).
. Pain that worsens when standing for long periods of time, walking or walking downhill.
. Pain that lessens when leaning, bending slightly forward, walking uphill or sitting.
. Loss of bladder or bowel control (in severe cases).
Symptoms of neck (cervical) spinal stenosis include:
. Neck pain.
. Numbness or tingling in the arm, hand, leg or foot. (Symptoms can be felt anywhere below the point of the nerve compression.)
. Weakness or clumsiness in the arm, hand, leg or foot.
. Problems with balance.
. Loss of function in hands, like having problems writing or buttoning shirts.
. Loss of bladder or bowel control (in severe cases).
Symptoms of abdomen (thoracic) spinal stenosis include:
. Pain, numbness, tingling and or weakness at or below the level of the abdomen.
. Problems with balance.
Can spinal stenosis cause permanent paralysis?
While the narrowing of the spine can cause pain, it usually doesn’t cause paralysis. However, if a spinal nerve or the spinal cord is compressed for a long period of time, permanent numbness and/or paralysis is possible. This is why it is especially important to see your healthcare provider right away if you experience numbness or weakness in your arms or legs.
Diagnosis and Tests
How is spinal stenosis diagnosed?
Your healthcare provider will review your medical history, ask about your symptoms and conduct a physical exam. During your physical exam, your healthcare provider may feel your spine, pressing on different area to see if this causes pain. Your provider will likely ask you to bend in different directions to see if different spine positions bring on pain or other symptoms. Your provider will check your balance, watch how you move and walk and check your arm and leg strength.
You will have imaging tests to examine your spine and determine the exact location, type and extent of the problem. Imaging studies may include:
. X-rays: X-rays use a small amount of radiation and can show changes in bone structure, such as loss of disk height and development of bone spurs that are narrowing the space in the spine.
. MRI: Magnetic resonance imaging (MRI) uses radio waves and a powerful magnet to create cross-sectional images of the spine. MRI images provide detailed images of the nerves, disks, spinal cord and presence of any tumors.
. CT or CT myelogram: A computed tomography (CT) scan is a combination of X-rays that creates cross-sectional images of the spine. A CT myelogram adds a contrast dye to more clearly see the spinal cord and nerves.
Prevention
Can spinal stenosis be prevented?
Since most causes of spinal stenosis are normal age-related “wear and tear” conditions, such as osteoarthritis and loss of bone and muscle mass, you can’t 100% prevent spinal stenosis. However, you can take certain measures to lower your risk or slow the progression, including:
. Eat a healthy diet and maintain an ideal body weight.
. Don’t smoke. If you do smoke, quit. Ask your healthcare provider for assistance to quit.
. Maintain good posture.
. Exercise. Avoid exercises that cause pain but do stay active. Check with your healthcare provider or physical therapist before starting a home exercise program. Too much rest can be more harmful than helpful.
Also keep in mind that although there is no “cure” for spinal stenosis, its symptoms can be successfully managed with the nonsurgical or surgical options discussed in this article.
During Spinal Stenosis Treatment
Management and Treatment
What are the treatments for spinal stenosis?
Choice of stenosis treatments depend on what is causing your symptoms, the location of the problem and the severity of your symptoms. If your symptoms are mild, your healthcare provider may recommend some self-care remedies first. If these don’t work and as symptoms worsen, your provider may recommend physical therapy, medication and finally surgery.
Self-help remedies include:
. Apply heat: Heat usually is the better choice for pain due to osteoarthritis. Heat increases blood flow, which relaxes muscles and relieves aching joints. Be careful when using heat – don’t set the settings too high so you don’t get burned.
. Apply cold: If heat isn’t easing your symptoms, try ice (an ice pack, frozen gel pack, or frozen bag of peas or corn). Typically, ice is applied 20 minutes on and 20 minutes off. Ice reduces swelling, tenderness and inflammation.
. Exercise: Check with your healthcare provider first, but exercise is helpful in relieving pain, strengthening muscles to support your spine and improving your flexibility and balance.
Non-surgical treatments include:
. Oral medications: Nonsteroidal anti-inflammatory medications (NSAIDs) – such as ibuprofen (Advil®, Motrin®), naproxen (Aleve®), aspirin – or acetaminophen (Tylenol®) can help relieve inflammation and provide pain relief from spinal stenosis. Be sure to talk with your healthcare provider and learn about possible long-term problems of taking these medicines, such as acid reflux and stomach ulcers. Your healthcare provider may also recommend other prescription medications with pain-relieving properties, such as the anti-seizure drug gabapentin (Neurontin®) or tricyclic antidepressants such as amitriptyline (Elavil®). Opioids, such as oxycodone (Oxycontin®) or hydrocodone (Vicodin®), may be prescribed for short-term pain relief. However, they are usually prescribed with caution since they can become habit forming. Muscle relaxants such as cyclobenzaprine (Amrix®, Fexmid®) can treat muscle camps and spasms.
. Physical therapy: Physical therapists will work with you to develop a back-healthy exercise program to help you gain strength and improve your balance, flexibility and spine stability. Strengthening your back and abdominal muscles — your core — will make your spine more resilient. Physical therapists can teach you how to walk in a way that opens up the spinal canal, which can help ease pressure on your nerves.
. Steroid injections: Injecting corticosteroids near the space in the spine where nerve roots are being pinched or where worn areas of bone rub together can help reduce inflammation, pain and irritation. However, only a limited number of injections are usually given (typically three or four injections per year) because corticosteroids can weaken bones and nearby tissue over time.
. Decompression procedure: This outpatient procedure, also known as percutaneous image-guided lumbar decompression (PILD), specifically treats lumbar spinal stenosis caused by a thickening of a specific ligament (ligamentum flavum) in the back of the spinal column. It is performed through a tiny incision and requires no general anesthesia and no stitches. The procedure is guided by an X-ray and a contrast agent that is injected during the procedure. The surgeon uses special tools to remove a section of the thickened ligament, which frees up space within the spinal canal, reducing compression on nerve roots. Some of the advantages of this procedure are that the bony architecture of the spine is left intact and there is little disruption in the mechanics of the spine so people recovery quickly. People usually go home a couple hours after the procedure and begin walking and/or physical therapy soon thereafter. Compared with before the procedure, you will be able to walk and stand for longer periods of time and experience less numbness, tingling and muscle weakness.
When is spinal stenosis surgery considered?
Because of the complexity of spinal stenosis and the delicate nature of the spine, surgery is usually considered when all other treatment options have failed. Fortunately, most people who have spinal stenosis don’t need surgery. However, talk with your healthcare provider about surgical options when:
. Your symptoms are intolerable, you no longer have the quality of life you desire and you can’t do or enjoy everyday life activities.
. Your pain is caused by pressure on the spinal cord.
. Walking and maintaining your balance have become difficult.
. You have lost bowel or bladder control or have sexual function problems.
What are the surgical treatments for spinal stenosis?
Surgery options involve removing portions of bone, bony growths on facet joints or disks that are crowding the spinal canal and pinching spinal nerves.
Types of spine surgery include:
. Laminectomy (decompression surgery): The most common type of surgery for this condition, laminectomy involves removing the lamina, which is a portion of the vertebra. Some ligaments and bone spurs may also be removed. The procedure makes room for the spinal cord and nerves, relieving your symptoms.
. Laminotomy: This is a partial laminectomy. In this procedure, only a small part of the lamina is removed – the area causing the most pressure on the nerve.
. Laminoplasty: In this procedure, performed in the neck (cervical) area only, part of the lamina is removed to provide more canal space and metal plates and screws create a hinged bridge across the area where bone was removed.
. Foraminotomy: The foramen is the area in the vertebrae where the nerve roots exit. The procedure involves removing bone or tissue this area to provide more space for the nerve roots.
. Interspinous process spaces: This is a minimally invasive surgery for some people with lumbar spinal stenosis. Spacers are inserted between the bones that extends off the back of each vertebrae called the spinous processes. The spacers help keep the vertebrae apart creating more space for nerves. The procedure is performed under local anesthesia and involves removing part of the lamina.
. Spinal fusion: This procedure is considered if you have radiating nerve pain from spinal stenosis, your spine is not stable and you have not been helped with other methods. Spinal fusion surgery permanently joins (fuses) two vertebrae together. A laminectomy is usually performed first and bone removed during this procedure is used to create a bridge between two vertebrae, which stimulates new bone growth. The vertebrae are held together with screws, rods, hooks or wires until the vertebrae heal and grow together. The healing process takes six months to one year.
Is spinal surgery safe? What are the risks of surgery for spinal stenosis?
All surgeries have the risks of infection, bleeding, blood clots and reaction to anesthesia. Additional risks from surgery for spinal stenosis include:
. Nerve injury.
. Tear in the membrane that covers the nerve or spinal cord.
. Failure of the bone to heal after surgery.
. Failure of the metal plates, screws and other fasteners.
. Need for additional surgery.
. No relief of symptoms/return of symptoms.
How do I prepare for spinal stenosis surgery?
To prepare for spine surgery, quit smoking if you smoke and exercise on a regular basis (after checking with your healthcare provider first) to speed your recovery time. Ask your provider if you need to stop taking any non-essential medications, supplements or herbal remedies that you may be taking that could react with anesthesia. Also, never hesitate to ask your healthcare team any questions you may have or discuss any concerns.
After Spinal Stenosis Treatment
What happens after spinal surgery?
If you’ve had a laminectomy, you may be in the hospital for a day or two. If you’ve had spinal fusion, you may have a three- to five-day hospital stay. If you’re older, you may be transferred to a rehabilitation facility to receive additional care before going home.
You will be given pain medications and/or NSAIDs to reduce pain and swelling. You may be given a brace or corset to wear for comfort. You will likely be encouraged to get up and walk as soon as possible. Your healthcare provider or physical therapist will recommend a light form of exercise right after spinal surgery to ensure that your back does not stiffen and to reduce swelling. Your physical therapist will develop an individualized exercise plan to stretch and strengthen muscles to support your back and stabilize your spine.
Taking hot showers and using hot compresses may help alleviate pain. Additionally, using an ice pack may ease pain before and after exercise.
How long is the recovery period after spinal stenosis surgery?
Full recovery after surgery for spinal stenosis and return to normal activities typically takes three months and possibly longer for spinal fusion, depending partially on the complexity of your surgery and your progress in rehabilitation.
When can I return to work after spinal surgery?
If you’ve had a laminectomy, you will likely be able to go back to work at a desk job within a few days of returning home. If you’ve had spinal fusion, you’ll likely be able to return to work a few weeks after your surgery.
Outlook / Prognosis
What can I expect if I have spinal stenosis?
First, spinal stenosis develops slowly over time, so you may not have symptoms even though changes are occurring in your spine. Your first noticeable symptoms may be pain, numbness, tingling or weakness in your back or neck or arms and legs depending on the location of the stenosis. Conservative treatments – such as pain-relieving and anti-inflammatory medicines, ice or heat, and physical therapy – may be enough to relieve pain for a period of time. As stenosis worsens and your quality of life is no longer acceptable to you, talk with your healthcare provider. Most people who undergo spinal stenosis surgery achieve good to excellent results with pain relief. Surgery results depend on your general health and presence of other medical conditions, severity and location of your spinal stenosis, experience and skills of your surgeon and your commitment to your recovery plan.
Can spinal stenosis be reversed? Can spinal stenosis get better?
No, spinal stenosis can’t be reversed but the process might be able to be slowed if you take good care of yourself by maintaining a healthy weight, eating healthy foods, exercising regularly to keep your bones and muscles strong, and following your healthcare provider’s instructions to best manage any existing medical conditions you may have. If you do develop symptoms, there are many options – up to and including surgery – that can be considered to relieve your pain and other symptoms so you feel better.
Can spinal stenosis heal on its own?
Generally no because the most common causes of spinal stenosis is normal age-related “wear and tear” on the bones and structures of the spine. However, if the cause of your spinal stenosis is a herniated disk, it can sometimes get better on its own with a short amount of rest or with treatments such as physical therapy, anti-inflammatory medications or spinal injections.
Can spinal stenosis happen in more than one area of the spine at the same time?
Yes. Spinal stenosis can happen in multiple locations at the same time, such as in both the lower back (lumbar spine) and neck (cervical spine).
Can spinal stenosis cause pain in my groin, hip, thigh and calf?
Yes, this is certainly possible. If your spinal stenosis is pinching your sciatic nerve – a nerve that originates in your lower (lumbar) spine – you might feel pain or have numbness, tingling or muscle weakness along this nerve’s pathway from your lower back, down your leg to your foot. This condition is known as sciatica.
What types of healthcare professionals might be involved in my care if I have spinal stenosis?
In additional to your regular healthcare provider, you may be seen by a team of healthcare professionals that could include:
. A rheumatologist to treat arthritis and related disorders.
. A neurologist to treat nerve disorders.
. An orthopaedic surgeon to operate on bones.
. A neurosurgeon to operate on conditions affecting the nervous system.
. A pain management specialist to manage pain and discomfort.
. A radiologist to interpret imaging studies such as X-rays, CT and MRI scans.
. A physical therapist to develop a healthy back and back surgery recovery exercise plan.
. A physiatrist/rehabilitation specialist to treat back pain using nonsurgical approaches.
. An acupuncturist to administer acupuncture therapy.
. A chiropractor to manipulate your spine and related muscles, ligaments and bones.
Can alternative treatments, such as acupuncture or chiropractics, help relieve pain from spinal stenosis?
Acupuncture and chiropractic manipulation may help relieve mild pain in some people with spinal stenosis. It’s important to keep in mind that similar to other nonsurgical treatments, these alternative therapies don’t improve the narrowing of the spinal canal. Also, chiropractic manipulation must be used in the proper person. For instance, manipulation may worsen symptoms or cause other injuries if a herniated disk is the cause of your spinal stenosis. That being said, alternative therapies are increasingly popular and are used to treat and manage all kinds of pain. Be sure to ask your healthcare provider if these alternative treatments as well as others, like yoga, massage or biofeedback, may be safe and appropriate to manage the cause of your spinal pain.
What medical problems can be confused with spinal stenosis?
Medical problems that can sometimes mimic spinal stenosis include neuropathy, peripheral artery disease, diabetes-related neuropathy and inflammatory arthritis, such as ankylosing spondylitis. Rare, but still other possible medical conditions that might be mistaken for spinal stenosis include cancer and abdominal aortic aneurysms.
Source:
. https://my.clevelandclinic.org/health/diseases/17499-spinal-stenosis