Nasolacrimal duct obstruction (NLDO)
What is NLDO of the eye?
What are signs of Nasolacrimal?
Nasolacrimal duct obstruction cause
Nasolacrimal duct obstruction diagnosis
Nasolacrimal duct obstruction management
How do you treat nasolacrimal duct blockage?
What antibiotics treat Dacryocystitis?
What is NLDO of the eye?
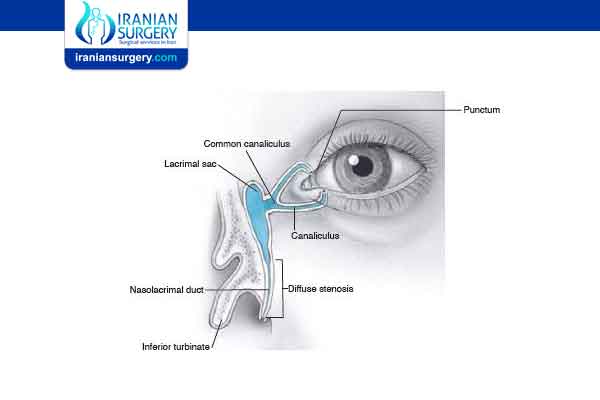
Nasolacrimal duct obstruction (NLDO) is the obstruction of nasolacrimal duct and may be either congenital or acquired. Obstruction of the nasolacrimal duct leads to the excess overflow of tears called epiphora.
Read more about: eye surgery in iran
What are signs of Nasolacrimal?
Signs and symptoms of a blocked tear duct include:
- Excessive tearing
- Redness of the white part of the eye
- Recurrent eye infection or inflammation (pink eye)
- Painful swelling near the inside corner of the eye
- Crusting of the eyelids
- Mucus or pus discharge from the lids and surface of the eye
- Blurred vision
Read more about: Are You a Candidate for lasik eye surgery?
Nasolacrimal duct obstruction cause
- Involutional stenosis
Involutional stenosis is probably the most common cause of NLD obstruction in older persons. It affects women twice as frequently as men. Although the inciting event in this process is unknown, clinicopathologic study suggests that compression of the lumen of the NLD is caused by inflammatory infiltrates and edema. This may be the result of an unidentified infection or possibly an autoimmune disease.
- Dacryolith
Dacryoliths or cast formation, within the lacrimal sac can also produce obstruction of the NLD.
- Sinus disease
Sinus disease often occurs in conjunction with, and in other instances may contribute to the development of NLD obstruction. Patients should be asked about previous sinus surgery, as the NLD is sometimes damaged when the maxillary sinus ostium is being enlarged anteriorly.
- Trauma
Naso-orbital fractures may involve the NLD. Early treatment by fracture reduction with stenting of the entire lacrimal drainage system should be considered. However, such injuries are often not recognized or are initially neglected as more serious injuries are managed. In such cases, late treatment of persistent epiphora usually requires DCR.
- Inflammatory disease
Granulomatous disease, including sarcoidosis, granulomatosis with polyangiitis, and midline granuloma, may also lead to NLD obstruction.
- Lacrimal plugs
As with similar cases of canalicular obstruction, dislodged punctual and canalicular plugs can migrate to and occlude the NLD.
- Neoplasm
Neoplasm should be considered in any patient presenting with NLD obstruction.In patients with an atypical presentation, including younger age and male gender, further workup is appropriate. Bloody punctual discharge or lacrimal sac distension above the medial canthal tendon is also highly suggestive of neoplasm.
- Congenital
Congenital nasolacrimal duct obstruction, or dacryostenosis, occurs when the lacrimal duct has failed to open at the time of birth, most often due to an imperforate membrane at the valve of Hasner. Around 6% of infants have CLDO, usually experiencing a persistent watery eye even when not crying. If a secondary infection occurs (Dacryocystitis), purulent (yellow / green) discharge may be present.
Most cases resolve spontaneously, with antibiotics reserved only if conjunctivitis occurs. Lacrimal sac massage has been proposed as helping to open the duct, though this is not always successful. The aim of massage is to generate enough hydrostatic pressure (downward, toward the nose) to “pop” open any obstruction. Additional massage may then be performed up toward the lacrimal punctum, in order to express any infectious material out of the nasolacrimal sac. When discharge or crusting is present, the lids should be gently cleaned using cooled pre-boiled water or saline.
Referral to an ophthalmologist is indicated if symptoms are still present at 12 months, or sooner if significant symptoms or recurrent infections occur. Nasolacrimal duct probing may be performed in the office setting (usually from 4 to 8 months of age) or under general anesthesia in an operating room for older patients. The success rate of probing is higher for younger children. A silastic tube or stent may be employed along with probing to maintain tear duct patency. A systematic review comparing immediate probing with deferred probing found that in children with unilateral NLDO, immediate probing resulted in a higher success rate of treatment compared to deferred probing.
Read more about: eye bag removal surgery in Iran
Nasolacrimal duct obstruction diagnosis
Evaluation is in the form of a dye disappearance test followed by irrigation test. By using this sequence (with modifications) as a guide, the physician can frequently streamline diagnostic testing.
- Dye disappearance test
The dye disappearance test (DDT) is useful for assessing the presence or absence of adequate lacrimal outflow, especially in unilateral cases. It is more heavily relied upon in children, in whom lacrimal irrigation is impossible without deep sedation. Using a drop of sterile 2% fluorescein solution or a moistened fluorescein strip, the examiner instills fluorescein into the conjunctival fornices of each eye and then observes the tear film, preferably with the cobalt blue filter of the slit lamp. Persistence of significant dye and, particularly asymmetric clearance of the dye from the tear meniscus over a 5-minute period indicate an obstruction. If the DDT result is normal, severe lacrimal drainage dysfunction is highly unlikely. Variations of the DDT are the Jones tests.
- Irrigation test
Flushing the nasolacrimal duct in a cat.
In irrigation test, a lacrimal irrigation cannula is passed into the punctum and advanced through the canaliculus to the lacrimal fossa. Clear water or saline is then irrigated through the cannula. If fluid passes into the nose without reflux out of the opposite canaliculus, the system is patent. If no fluid passes but it all comes back through either punctum, nasolacrimal duct obstruction is present.
Read more about: PRK eye surgery in Iran
Nasolacrimal duct obstruction management
- Intubation and stenting
Some clinicians believe that partial stenosis of the NLD with symptomatic epiphora sometimes responds to surgical intubation of the entire lacrimal drainage system. This procedure should be performed only if the tubes can be passed easily. In complete NLD obstruction, intubation alone is not effective, and a DCR should be considered.
- Dacryocystorhinostomy (DCR)
A DCR is the treatment of choice for most patients with acquired NLD obstruction. Surgical indications include recurrent dacryocystitis, chronic mucoid reflux, painful distension of the lacrimal sac, and bothersome epiphora. For patients with dacryocystitis, active infection should be cleared, if possible, before DCR is performed.
Read more about: Epi-lasik eye surgery
How do you treat nasolacrimal duct blockage?
For adults with a blocked tear duct, treatment usually require a doctor’s attention. There’s no home remedy, though keeping your face and eyes and contact lenses if you use them clean may help prevent tear duct complications in the future.
The proper treatment for a blocked tear duct depends on the underlying cause.
If you have a bacterial infection, your doctor will prescribe antibiotic eye drops or pills to treat the infection.
For a narrowed punctum, your doctor can use a small probe to widen it. They’ll then flush or irrigate the tear duct with a saline solution. This is an outpatient procedure.
If an injury caused the blockage, your best approach may be to wait several weeks to see if it heals on its own without any treatment.
Other treatments for a blocked tear duct may include:
- Balloon catheter dilation
Your doctor guides a very thin catheter through the blockage in the tear duct, starting from the nose. They then inflate a tiny balloon several times to push away the blockage and open up the duct system. This requires general anesthesia.
- Stenting or intubation
Your doctor threads a thin tube through the puncta and throughout the tear drainage system to the nose. The tube, or stent, remains in place and allows tears to drain normally. The procedure also requires general anesthesia.
- Surgery
The surgical procedure is called dacryocystorhinostomy. It can be done through an incision on the side of the nose near the lacrimal sac or with special endoscopic tools through the nasal cavity, which leaves no visible scar.
Read more about: Keratoconus
What antibiotics treat Dacryocystitis?
Topical antibiotics include Polytrim, gentamicin, tobramycin, and TobraDex (antibiotic/steroid combination drop). Occasionally, nasal decongestants (eg, Afrin) are used on a short-term basis. Oral antibiotics are useful in patients with acute dacryocystitis who are not acutely ill.
Read more about: Dacryocystorhinostomy(DCR) surgery Iran

