Lumbar Radiculopathy
What is Lumbar Radiculopathy?
Lumbar radiculopathy is inflammation of a nerve root in the lower back that causes symptoms in the back and down the leg.
Radiculopathy in the lumbar region
Radiculopathy is pain and other neurological symptoms caused by the pinching of nerve roots where they leave your spinal cord. When radiculopathy develops in your lower back, it’s called lumbar radiculopathy.
Lumbar radiculopathy is very common and is estimated to occur in 3% to 5%Trusted Source of people at some point in their life. The vast majority of cases resolve with conservative management. Potential causes include herniated discs, spinal degeneration, and narrowing of the bony canal where nerves exit your spinal cord.
If conservative treatments fail to alleviate your symptoms, a doctor may recommend surgery.
Keep reading to learn more about lumbar radiculopathy, including symptoms, causes, and treatment options.
Before Lumbar Radiculopathy Treatment
Lumbar radiculopathy symptoms
Pain is the most common symptom of radiculopathy. It’s often described as electric, burning, or sharp pain that may worsen with activity. The pain may travel down your:
. buttocks
. hip
. groin
. leg
This type of pain is also referred to as sciatica.
Other signs and symptoms of lumbar radiculopathy can include:
. weakness
. loss of reflexes
. numbness
. pins and needles
. issues walking
What causes lumbar radiculopathy?
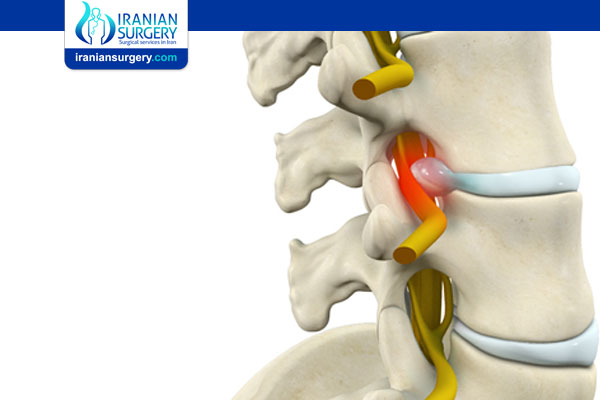
Lumbar radiculopathy is caused by pressure on a nerve root. This pressure causes the nerve root to become inflamed. Any condition that puts pressure on a nerve root can lead to lumbar radiculopathy.
The most common underlying cause is a herniated disc in your lower back.
A herniated disc is when the jelly-like interior of one of the discs between your vertebrae bulges out of the thicker exterior. Herniated discs are most likely to occur at the level of L4, the fourth vertebrae from the bottom of your spine.
Other causes can include:
. degenerative conditions and complications, such as:
. spinal stenosis
. spondylolisthesis
. bone spurs
. traumatic injury like a fracture
. benign or cancerous tumors
. infections
. vascular conditions like hemangioblastoma
Who’s at risk for lumbar radiculopathy?
Age is the primary risk factor for lumbar radiculopathy, according to a 2019 research review. The peak age range is 45 to 64. Men often are affected in their 40s and women in their 50s and 60s, the 2019 review suggests.
Men have a higher risk than women overall, but certain subgroups of women have a higher risk. For example, women who have physically strenuous careers like military service are at higher risk, according to the researchers of the 2019 review.
Other risk factors for lumbar radiculopathy may include:
. working a job that involves driving
. frequently lifting, especially with poor form or twisting
. doing heavy industrial work
. having a history of back trauma
. having a taller height
. smoking
. having a chronic cough
. being overweight
. not being physically active
. having had multiple pregnancies
How is lumbar radiculopathy diagnosed?
Doctors usually start the diagnostic process by reviewing your medical history and performing a physical exam. The physical exam will likely include tests such as:
. muscle function testing
. deep reflex testing
. sensation testing
Your doctor will likely perform Lasegue’s sign. This is a test where you lie on your back and your doctor raises your leg straight to assess for pain.
If your back pain doesn’t resolve in 1 or 2 months, your doctor will likely want to order imaging. Magnetic resonance imaging (MRI) is considered the gold standard imaging technique. Computed tomography (CT) scan is an option for people who can’t undergo an MRI.
In some cases, nerve conduction tests are used to find where along the nerve the problem is located. These tests involve placing electrodes on your skin that send very small amounts of electricity through your nerves.
Can you prevent lumbar radiculopathy?
Some causes of lumbar radiculopathy, like age-related degeneration, may be outside of your control. The most common cause of lumbar radiculopathy is a herniated disc. You may be to lower your odds of a herniated disc by:
. lifting weights with good technique and not heavier than your capabilities
. maintaining a healthy weight
. breaking up periods of prolonged sitting
. avoiding smoking, which may increase disc degeneration
. avoiding twisting when lifting heavy objects
. exercising regularly
When to contact a doctor
You may want to contact a doctor if you have persistent pain that lasts for more than a couple of days. It’s especially important if you have pain that keeps you up at night or you have other concerning symptoms like urinary incontinence or numbness in the genital region or saddle region, which are symptoms of cauda equina syndrome.
During Lumbar Radiculopathy Treatment
Treatment for lumbar radiculopathy
Treatment for lumbar radiculopathy depends on the underlying cause and severity of your symptoms. Conservative treatment is usually considered before surgery.
About 90% of people with back pain caused by disc herniation see improvements within 3 months without surgery.
Lumbar radiculopathy exercises
Doctors usually recommend staying active after your injury.
The 2019 review mentioned earlier suggests that a certain set of exercises called McKenzie exercises may provide short-term symptom relief. The best way to perform these exercises is with guidance from a physical therapist or other trained professional.
These exercises may include movements, such as:
. lying flat and facedown
. propping yourself on your elbows with your spine extended
. propping yourself on your hands with your elbows fully extended
. extending your spine while standing with your hands on your lower back
Over-the-counter (OTC) medication
A doctor may recommend OTC medications to help manage pain. These include acetaminophen (Tylenol) and nonsteroidal anti-inflammatory drugs like ibuprofen.
Medical treatment
If OTC medications aren’t effective for pain relief, your doctor may recommend one of several types of injections to reduce inflammation and pain, including:
. epidurals
. facet injections
. transforaminal injections
Injections typically contain a mixture of an anti-inflammatory drug and a long-lasting anesthetic.
Surgery
There is some controversy about when surgery should be considered for lumbar radiculopathy. In general, doctors likely won’t recommend surgery until other treatments have failed to offer relief for at least 4 to 8 weeks.
The type of surgery you receive depends on the underlying cause of the radiculopathy. The gold standard for disc herniation is a diskectomy, which is the removal of the injured part of your disc.
Source:
. https://www.healthline.com/health/lumbar-radiculopathy