Lobectomy
What is lobectomy?
VATS for lung cancer surgery
Candidates for VATS lobectomy
Is a lobectomy major surgery?
What happens when a lung lobe is removed?
How long does it take to recover from a lung lobectomy?
Is coughing normal after lobectomy?
What is lobectomy?
If you have a lung disease, a type of surgery called a lobectomy is one treatment option your doctor may suggest.
Your lungs are made up of five sections called lobes. You have three in your right lung and two in your left. A lobectomy removes one of these lobes. After the surgery, your healthy tissue makes up for the missing section, so your lungs should work as well or better than they did before.
It’s usually the main treatment for people with the early stages of lung cancer, when there’s a tumor in just one part of the lung. In that case, a lobectomy may offer the best chance for a cure and may be the only treatment you need. But it doesn't help when cancer has spread to your whole lung or to other parts of your body.
The surgery may also help people who have other diseases in one part of their lungs, like:
- Tuberculosis
- Emphysema
- Tumors that aren’t cancer
- Fungal infections
- Pus that fills one area, called an abscess
When you have the damaged lobe removed, other parts of your lungs expand, making it easier to breathe.
Read more about : Chemotherapy Procedure
Read more about: cervical cancer risk factors
Traditional approach to lung cancer surgery: thoracotomy
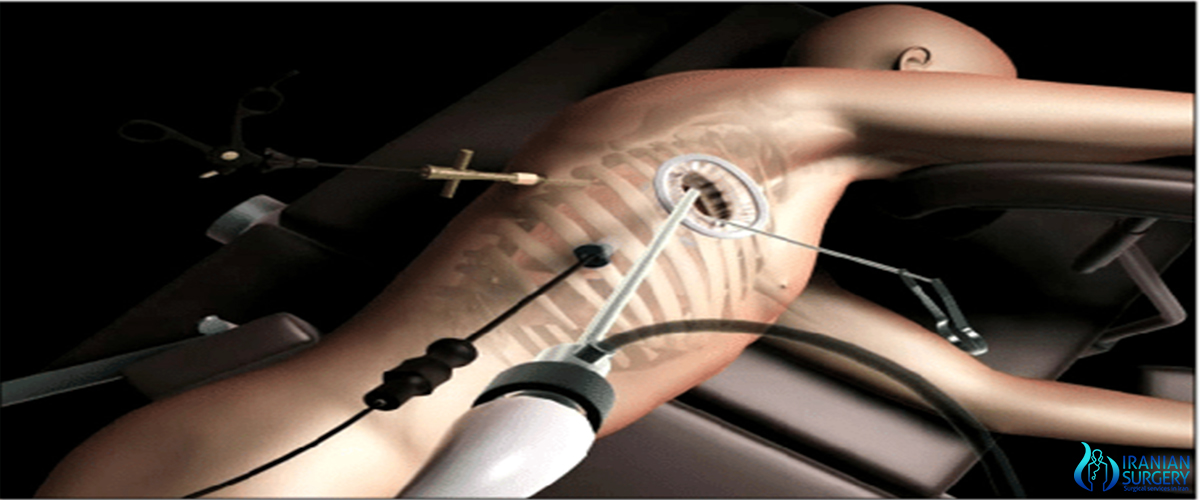
Dissection of the right superior pulmonary vein with VATS
Dissection of the anterior trunk of the right pulmonary artery with VATS
Preparing to divide the anterior trunk of the right pulmonary artery with the endoscopic stapler
Placing the resected lobe into a water-tight bag for removal from the chest
Anatomic lung resection, i.e. pulmonary lobectomy or pneumonectomy, in conjunction with removal of the lymph nodes from the mediastinum is the treatment modality that provides the greatest chance of long-term survival in patients with early stage non-small cell lung cancer. Anatomic lung resections require a dissection of the pulmonary hilum with individual ligation and division of the pulmonary artery, pulmonary vein, and the bronchus where these enter the lung. In the setting of lung cancer, the rationale for anatomic lung resection is a complete removal of a lung tumor along with the lymphatics that drain that tumor to assure that any tumor cells present in the lymphatics will also be removed; lesser resections have been shown to be associated with a higher risk of local recurrence and diminished long-term survival. A cornerstone of surgical treatment of early stage lung cancer is aggressive removal of lymph nodes from the mediastinum; this enhances the likelihood of removing all cancer cells (complete resection) and identifies patients who will require additional treatment (i.e. adjuvant chemotherapy). An important consideration when performing anatomic lung resection is to spare as much lung tissue as possible; while lobectomy and pneumonectomy are equivalent cancer operations, the risk of complications and morbidity is considerably less with lobectomy.
Traditionally, pulmonary lobectomy is performed through a poster-lateral thoracotomy incision; over decades, thoracotomy has demonstrated its effectiveness in providing access to structures in the thorax and is in general tolerated by patients. Thoracotomy, as most commonly performed, requires cutting through one or more major muscles of the chest wall including the latissimus dorsi, pectoralis or serratus muscles, and spreading of the ribs with a rib spreader. Because the joints of the ribs with the vertebral bodies have only limited flexibility, the use of a rib spreader usually results in rib fracture in the process of rendering the interspace between the ribs wide enough to perform a pulmonary lobectomy. Because of this, thoracic surgeons generally intentionally remove a section of one or more ribs in an effort to prevent splintered rib fracture associated with the use of the rib spreader. There is wide consensus that thoracotomy is one of the most painful incisions that patients can undergo. In the initial post-operative setting after thoracotomy, the use of epidural catheters, patient-controlled analgesia pumps for intravenous narcotic administration, and intravenous ketorolac are commonplace and patients generally require a 7- to 10-day hospital stay before their pain is adequately controlled with oral opioidanalgesics that they can take at home. A great deal of emphasis is placed on post-operative pulmonary toilet because the incisional pain associated with thoracotomyleads to a decreased ability of patients to cough and clear bronchial secretions, which in turn leads to an increased risk of persistent atelectasis (collapsed areas of lung) or pneumonia. Finally, to allow time for the divided muscles and bone fractures to heal, patients must refrain from strenuous activity or lifting greater than 5 lbs for 6 weeks after surgery.
Read more about: Liver Biopsy
The advent of VATS (video-assisted thoracoscopic surgery)
Video-assisted thoracoscopic surgery, or VATS, came into widespread use in the 1990s and early on in its development practitioners began to perform lobectomy via VATS incisions. The advantage of VATS over thoracotomy is that major chest wall muscles are not divided and ribs are not spread. This leads to reductions in the intensity and duration of post-operative pain and allows patients to return to full activity more quickly.
VATS for lung cancer surgery
VATS lobectomy is the same as lobectomy performed via thoracotomy in that the pulmonary artery, pulmonary vein, and bronchus to the involved pulmonary lobe are individually dissected, ligated and divided. Generally, endoscopic stapling devices are used to ligate and divide the vessels and the bronchus however conventional suture material can also be used. During VATS lobectomy, the structures being operated on are not directly visualized with the naked eye but are visualized solely with a rigid thoracoscope. A camera attached to the thoracoscope transmits the image to a video screen, which allows surgeons and assistants to observe the flow of the operation. Surgical specimens are placed into a water-tight bag and removed from the chest without morcellization (i.e. breaking up the specimen into small pieces before removal); this prevents seeding of the VATS incisions with tumor cells and allows for an intact specimen for pathology examination and cancer staging. Removal of lymph nodes from the mediastinum is not compromised by VATS and remains a cornerstone of the surgical therapy of lung cancer. Visualization is enhanced due to the magnification afforded by the fiberoptic thoracoscope and a 30-degree angle of visualization aids in looking around corners. However, because the incisions are too small to allow passage of the surgeon's hands into the thorax, the surgeon's tactile input is compromised. VATS operations rely on a thorough understanding of pulmonary anatomy to allow for strategically placed incisions (usually 3–5 incisions total). The main advantages of VATS over thoracotomy are that major muscles of the chest wall are not divided and rib spreaders that can lead to rib fractures or costovertebral joint pain are not used. This results in a hospital length of stay after VATS lobectomy generally reported to range from 3–5 days, or roughly half that for lobectomy via thoracotomy.
Read more about: Segmentectomy (removal of an anatomic division of a particular lobe of the lung)
Candidates for VATS lobectomy
Not all patients are candidates for VATS lobectomy. The classic indication for a VATS approach to lobectomy is early stage lung cancer in which the primary tumor is 3 cm or less in diameter and located toward the periphery of the lung parenchyma. Tumors that are located close to the major blood vessels or airway where these enter the lung or larger tumors associated with tumor spread to lymph nodes in the central regions of the lung may require the enhanced tactile input afforded by thoracotomy to make sure the tumors are resected with a negative margin, i.e. that the tumor is surrounded completely by a margin of non-cancerous tissue, and that arteries and airways to portions of the lung that are not being removed are preserved intact. In addition, patients who have had pre-operative chemotherapy or radiation for lung cancer or previous chest surgeries may not be candidates for VATS due to scarring around the major blood vessels that makes dissection via VATS difficult. Cases in which a lung tumor invades the chest wall and an en bloc resection of ribs must be performed to achieve negative resection margins generally are felt to abrogate the value of VATS. Finally, pneumonectomy by VATS, though it has been reported, is generally not performed because the size of the specimen requires a large incision with or without rib spreading for removal, abrogating the value of VATS.
Read more about: Bronchoplasty
Published benefits of lobectomy performed by VATS versus thoracotomy
Because of the lesser chest wall trauma of VATS compared to thoracotomy, elderly patients have been shown to tolerate lobectomy by VATS better than via thoracotomy. Patients who require chemotherapy after surgery have been shown to be more likely to succeed in completing the prescribed course of chemotherapy after VATS lobectomy compared to lobectomy via thoracotomy. Along with the lesser chest wall trauma and improved pulmonary mechanics, a lesser level of cytokine disturbance has been reported after VATS lobectomy compared to thoracotomy. From the standpoint of medical economics, VATS lobectomy is less expensive than lobectomy performed via thoracotomy because hospital length of stay and number of days in the intensive care unit are significantly reduced.
Is a lobectomy major surgery?
A lobectomy is a major surgery and it has some risks. The risks of this procedure may include: Infection, Air in the space between the lung covering (pleural space) that causes the lung to collapse (pneumothorax)and bleeding…
Your risks may vary depending on your general health and other factors. Ask your healthcare provider which risks apply most to you. Talk with him or her about any concerns you have.
Read more about: Sublobar resection (removal of part of lobe of the lung)
What happens when a lung lobe is removed?
The surgeon cuts some muscle and spreads the ribs apart. He or she surgically removes the affected lung. The sac that contained the lung (pleural space) fills up with air. Eventually, fluid takes the place of this air. the affected lobe is removed, and the remaining healthy lung tissue can work as normal.
A lobectomy is most often done during a surgery called a thoracotomy. During this type of surgery, the chest is opened.
In most cases, during a lobectomy the cut (incision) is made at the level of the affected lobe. The cut is most often made on the front of the chest under the nipple and wraps around the back under the shoulder blade.
Read more about: Wedge Resection
How long does it take to recover from a lung lobectomy?
Lung resection is surgery to remove part or all of your lung. It is used to treat a damaged or diseased lung.
It is common to feel tired for 6 to 8 weeks after surgery. Your chest may hurt and be swollen for up to 6 weeks. It may ache or feel stiff for up to 3 months. For up to 3 months, you may also feel tightness, itching, numbness, or tingling around the cut (incision) the doctor made. Your doctor will give you medicines to help with pain.
You may have stitches or staples in the incision. Your doctor will take these out 1 to 2 weeks after your surgery. You may have one or more tubes coming out of your chest to drain fluids. Your doctor will probably take these out about 1 week after surgery.
After surgery, you will probably feel short of breath. Your doctor, nurse, or respiratory therapist will teach you deep-breathing and coughing exercises to help your body get as much oxygen as possible. At first, you also may need to get extra oxygen through a mask or a plastic tube in your nostrils (nasal cannula).
Read more about: Liver transplantation
Is coughing normal after lobectomy?
Approximately 25–50% of patients have been reported to experience cough after lung cancer surgery. During surgery, a plastic tube is inserted into your airway so the machine can breathe for you: This can cause irritation, and is a frequent cause for cough. (That usually lasts only a few days.) Fluid overload can also do it. Infection in the lung is probably the biggest concern.

