Uterine Factor Infertility
Uterine Factor Infertility
What is Absolute Uterine Factor Infertility?
Infertility is a disease of the reproductive system that affects about 15% of heterosexual (a man and woman) couples in the United States. For most people, infertility is diagnosed after one year of unprotected sex without a pregnancy. It’s not always clear why infertility happens. While a third of cases are due to a female factors and a third are due to male factors, the remaining third of cases are due to unknown factors or a combination of factors.
Among the female factors for infertility, absolute uterine factor infertility is a condition where a woman is unable to get pregnant because her uterus is not present or completely non-functional. The uterus is an organ specific to the female reproductive system. It consists of the fallopian tubes (which sweep up eggs after they exit the ovaries), the main body of the uterus (which is the home of the growing fetus during pregnancy) and the cervix (which connects the uterus to the top of the vagina). The uterus is roughly the size of an upside down pear and has the ability to expand to accommodate a fetus and shrink back down in size after a delivery.
There are two types of absolute uterine factor infertility: congenital and acquired. A congenital condition is one that’s there at birth.
If you have congenital absolute uterine factor infertility, it means that you were born without a uterus, a condition known as Mayer-Rokitansky-Küster-Hauser syndrome (MRKH).
Acquired absolute factor infertility is caused when the uterus is surgically removed. This can happen for a variety of reasons and is done through a procedure called a hysterectomy. The hysterectomy may have been done to save a woman’s life, such as in life-threatening hemorrhage or a cancer diagnosis, or because of severe pain, such as in severe forms of endometriosis.
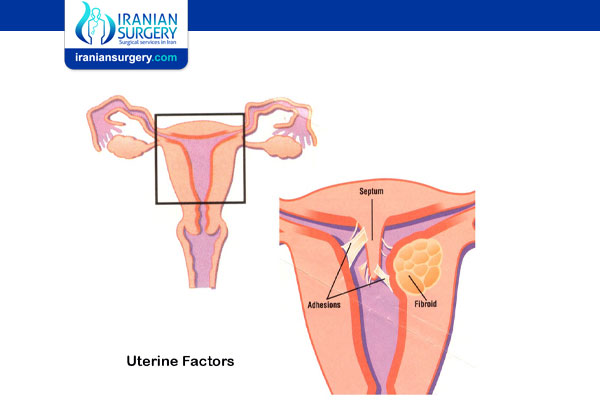
It is possible to have uterine factor infertility and still have a uterus. This can include infertility that’s caused by fibroids, polyps, scar tissue, radiation damage or injuries to the uterus that prevent a pregnancy. Asherman’s syndrome is a rare condition where the scar tissue in the uterus creates adhesions — physical blocks — inside the uterus, preventing a pregnancy. Causes of Asherman’s syndrome include infections, radiation, and uterine surgery, such as dilation and curettage (D&C) procedures.
Before Absolute Uterine Factor Infertility Treatment
How is absolute uterine factor infertility different from other types of female infertility?
It can often be difficult to pinpoint the reason a woman or couple has infertility issues. With absolute uterine factor infertility, however, the problem is clear. While a physical exam is usually enough for the diagnosis, use of ultrasound and other imaging can confirm that the uterus is absent.
All causes of infertility can have a great emotional toll on the people experiencing it. Different types of infertility may cause unique kinds of challenges.
For those with acquired absolute uterine factor infertility, they may have had life-threatening bleeding requiring an emergency hysterectomy to save their life, with little or no time to think about or emotionally prepare for this new, sudden form of infertility.
For people with congenital (born with) absolute uterine factor infertility, this discovery happens during the teen years when her period doesn’t start. Before then, there is usually no reason to suspect that the uterus might be missing, so this discovery can be shocking and devastating. They then face the difficulty of knowing from an early age that they do not have a uterus. For these women, questions about when to tell a new partner about their absolute infertility or worries about how the inability to have children may impact their future family life can be difficult.
What causes uterine factor infertility?
Absolute uterine factor infertility happens when the uterus is not present, the uterus is underdeveloped, or the uterus is present but is nonfunctional. There are two main causes of absolute uterine factor infertility. These causes include:
. Being born without a functioning uterus.
. Having the uterus removed (hysterectomy).
Being born without a uterus.
This is a rare congenital (something you are born with) condition called Mayer-Rokitansky-Küster-Hauser syndrome (MRKH). This condition causes parts of the female reproductive system to be underdeveloped — meaning the vagina can be shorter than normal or the uterus may not be the correct shape and size. In severe cases, there’s no uterus present at birth. In MRKH, the ovaries are present and functioning, so patients may still have mood changes and other signs of a menstrual cycle, but they will not have bleeding. While the ovaries aren’t affected, MRKH is associated with kidney and skeletal problems. MRKH is often diagnosed during the teen years when menstrual cycles (periods) don’t start as expected.
Having the uterus removed (hysterectomy).
Having the uterus surgically removed during childbearing years can happen for a variety of reasons. These reasons can include:
. Hemorrhage: A hysterectomy — the procedure used to remove the uterus — can be an emergency surgery that’s used to save a life. A woman might need an emergency hysterectomy if she has a severe hemorrhage (large amounts of blood loss). This can happen during a Cesarean section (C-section) when there’s severe bleeding that needs to be controlled. In this case, a hysterectomy is a life-saving procedure for the mother, but it results in the loss of her uterus right after childbirth.
. Cancer: Another reason the uterus could be surgically removed is cancer. When removing the uterus could help treat and stop the spread of cancer throughout the body, a hysterectomy may be an option.
. Severe endometriosis, fibroids, or adenomyosis: A hysterectomy may also be used in severe cases of endometriosis, adenomyosis, or fibroids. These are different benign diseases (meaning they aren’t forms of cancer) in the female reproductive system that can cause very severe symptoms, including pelvic pain, bowel and bladder issues, and heavy bleeding. There are many treatments and surgeries that do not require removal of the uterus. However, in very severe cases, these other therapies aren’t enough and the uterus must be completely removed.
What are the signs or symptoms of uterine factor infertility?
In women who have absolute uterine factor infertility (who have not had a hysterectomy), the main symptom is never having had menstrual periods. This is often the sign that leads a doctor to perform a physical exam or an imaging test and reveal the diagnosis.
Diagnosis and Tests
How is uterine factor infertility diagnosed?
Women who are born without a uterus (MRKH), are typically diagnosed at a young age, often in their teen years. This early diagnosis happens because the young woman doesn’t get a menstrual period. A healthcare provider will typically use an ultrasound (an imaging test that uses sound waves to create an image of something inside your body) to look at the reproductive organs. The size and shape of the vagina and the uterus will be examined. If the uterus is not there, the healthcare provider will usually diagnose MRKH.
For those with acquired absolute uterine factor infertility, the healthcare provider will look over the medical history. If a hysterectomy has been done in the past, the provider will confirm a diagnosis of absolute uterine factor infertility.
Prevention
Can absolute uterine factor infertility be prevented?
When absolute uterine factor infertility is caused by a congenital condition like MRKH, it’s unfortunately not preventable. This condition happens before birth and there’s currently no screening for it during pregnancy.
In acquired cases of absolute uterine factor infertility, prevention centers around pre-surgery discussions with the healthcare team. It’s important to be very open and honest with your healthcare provider about your wishes for future children. In some cases, there are other options for treatment that don’t involve a hysterectomy. Ask your provider for all of your options and ask for information about the risks and benefits of each choice. However, it’s also important to remember that there are times when a hysterectomy is a life-saving surgery. In those cases there may not be time to discuss the pros and cons of the procedure.
During Absolute Uterine Factor Infertility Treatment
Management and Treatment
How is absolute uterine factor infertility treated?
For a long time there was no treatment for women without a uterus. Whether it happened at birth or through a hysterectomy, not having a uterus meant that the only options for family-building were (where available and legal) adoption or gestational surrogacy. However, uterus transplantation has changed this in recent history. Though they aren’t commonplace currently, uterus transplantation is a procedure that can allow a woman to have a baby even if she has absolute uterine factor infertility.
A uterus transplant is similar to many other organ transplants. The organ is taken from a donor and surgically implanted in a recipient, who must take special medications to prevent their immune system from rejecting the transplanted organ. There are two types of donors that can give a donor – living and deceased.
. Living donors: A living donor can either be directed (known) or non-directed (anonymous). A directed donor is often a family member (a mother or sister) who chooses to give their uterus. These are called directed donors because their identity is known and there’s often a clear connection between the person giving the organ and the person receiving it. There are also anonymous donors (non-directed). These are people who decide that they want to donate their uterus, but they don’t have any one person singled out for the organ.
. Deceased donors: In this case, the donor is someone who has died and who previously expressed a wish to give their organs to others. This is also done with family consent of the deceased person. The donor typically has no relationship with the recipient in this type of organ donation.
Before they are put on a waiting list to receive a transplanted uterus, the patient undergoes in vitro fertilization (IVF) to create embryos in the lab. Most patients with absolute uterine factor infertility have ovaries (the part of the reproductive system that provides the egg). As part of the IVF process, medications are given to stimulate the ovaries to produce lots of mature eggs, which are retrieved during a surgical procedure. These eggs are fertilized and become embryos. The embryos are frozen so that when everything is ready, they can be implanted into the transplanted uterus.
Unlike a traditional organ transplant, a uterus transplant is not meant to last forever. The uterus is removed after the delivery of one or two babies. This is done to prevent long-term risks from the immunosuppressant medications transplant patients need to use after receiving a new organ. In any transplant, there is always a worry that the body will fight and “reject” the new organ and think of it as an invader. To avoid this, medications called immunosuppressants are used to avoid rejection. These medications, however, have their own risks and side effects.
After one or two babies — or if there is concern for severe rejection or transplant complications--the transplanted uterus is removed through a hysterectomy.
After Absolute Uterine Factor Infertility Treatment
Outlook / Prognosis
Is there a cure for absolute uterine factor infertility?
Uterus transplantation is the only treatment for absolute uterine factor infertility. Receiving a transplant isn’t permanent, but it can allow a woman to carry her own children before the uterus is removed. Currently, uterus transplantation is not widely available and is only through clinical trials. In the future, there is hope that this treatment will be widely available for women with absolute uterine factor infertility.
Source:
. https://my.clevelandclinic.org/health/diseases/17738-uterine-factor-infertility