Side effects of fissure surgery
How long does it take to recover from fissure surgery?
Can fissure come back after surgery?
Is fissure surgery painful?
How successful is fissure surgery?
Is fissure completely curable?
Is laser treatment safe for fissure?
Which surgery is best for fissure?
What is the fastest way to heal after fissure surgery?
Side effects of fissure surgery may include the following:
- Infection.
- Bleeding.
- Fistula development.
- Incontinence (the most feared complication)
As with all surgery, you should expect some discomfort. It can be quite painful for the first couple of days and it may seem like it gets worse before it starts to feel more comfortable again, but the pain will ease.
Read more about: fissure surgery recovery time
Read more about: stages of fissure healing
Read more about: Colorectal cancer
How long does it take to recover from fissure surgery?
It is important to note that complete healing with both medical and surgical treatments can take up to approximately 6-12 weeks. However, acute pain after surgery often disappears after a few days. Most patients will be able to return to work and resume daily activities a few short days after the surgery.
Can fissure come back after surgery?
Approximately 1-6% of patients have a recurrence of their anal fissure after sphincterotomy. The recurrence rate is higher after a sphincter stretch. If a patient develops a recurrence after a sphincterotomy, it could be from recurrent disease or from an improperly or incompletely performed initial sphincterotomy. Having a fissure come back again (recur) after a sphincterotomy is rare and most patients are satisfied with the results of the procedure.
Read more about: Precautions after fissure surgery
Is fissure surgery painful?
Fissure surgery or sphincterotomy is less painful than the fissure itself. This surgery causes mild pain and reduces pain and pressure resulting from fissures. Some of the complications of sphincterotomy involve:
- Temporary inability to control gas
- Mild fecal leakage
- Infection
In one study that compared the outcomes of patients with sphincterotomies with those who had a fissurectomy, all patients reported no pain or bleeding one week after their surgery, and all wounds were fully healed by eight weeks. Those who had a sphincterotomy, however, had faster wound healing and a lower rate of recurrences.
Read more about : Femoral Hernia vs. Inguinal Hernia
Read more about : Anal fissure surgery
Read more about : What should not eat in fissure?
How successful is fissure surgery?
The success rate for fissure healing following surgery was 92 %, being significantly more likely in patients with textbook symptoms (p = 0.016) and those with chronic disease (p = 0.006). The overall complication rate was 13.2 %. Success rates after lateral anal sphincterotomy were satisfactory, but careful patient selection based on symptoms and disease chronicity may improve results further. Patients with predisposing risk factors for the development of incontinence, particularly multiparous women, are arguably better treated with non-surgical options.
Read more about: Anal fissure surgery
Is fissure completely curable?
Most anal fissures heal with home treatment after a few days or weeks. These are called short-term (acute) anal fissures. If you have an anal fissure that hasn't healed after 8 to 12 weeks, it is considered a long-term (chronic) fissure. A chronic fissure may need medical treatment. In the present study, 98% of patients presenting with a chronic anal fissure were successfully cured medically.
Read more about: Foods that heal fissures
Is laser treatment safe for fissure?
With advancement in science and technology fissure can be treated easily through laser-based surgery. The surgery can be easily performed by using local anaesthesia in a clinic with least postoperative morbidity. The chance of recurrence of the fissure is also less compared to the traditional surgeries.
Laser treatment of fissure generally involves the use of CO2 laser. The infrared radiation from the laser is used to increase the blow flow to the area of fissure which results in proper healing of the fissure. The reason CO2 laser is used is that it offers a fixed area of concentration and greater control over the surgery.
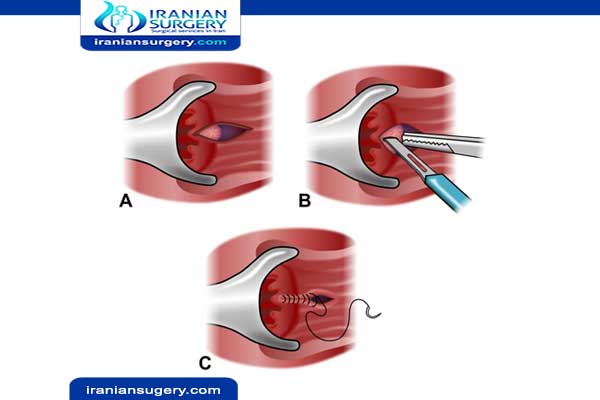
There is another type of surgery that is conducted which is called sphincterotomy. In this surgery, the sphincter is cut with the help of scalpel which handled by the surgeon.
Read more about: Anal fissure surgery Risks and side effects
Which surgery is best for fissure?
Lateral sphincterotomy
A lateral sphincterotomy involves making a small cut in the ring of muscle surrounding the anal canal (sphincter) to help reduce the tension in your anal canal. This allows the anal fissure to heal and reduces your chances of developing any more fissures.
It is a short and relatively straightforward operation that's usually carried out under a general anaesthetic on a day patient basis. This means you'll be asleep while the procedure is carried out, but you won't usually have to spend the night in hospital.
A lateral sphincterotomy is 1 of the most effective treatments for anal fissures, with a good track record of success. Most people will fully heal within 2 to 4 weeks.
Less than 1 in 20 people who have this type of surgery will experience some temporary loss of bowel control (bowel incontinence) afterwards as a result of damage to the anal muscles.
However, this is usually a mild type of incontinence where the person is unable to prevent passing wind, and usually only lasts a few weeks.
What is the fastest way to heal after fissure surgery?
- The most important thing you can do to facilitate your recovery is to keep your bowels soft and moving and avoid constipation at all costs. Most of the pain and discomfort that people have after this kind of surgery is related to bowel movements.
- In the week prior to the surgery begin taking stool softeners such as Colace or Docusate and adding a fiber supplement to your daily routine such as Benefiber, Citrucel, Metamucil or a similar product. The goal is to have soft but formed stools.
- Stay well hydrated and drink lots of fluids including juices and Gatorade. Your colon helps to maintain water balance in your body and if you get dehydrated this can cause constipation and hard stools.
- You must continue to eat. Fasting to avoid having bowel movements does not work well as people find they end up feeling constipated after a few days and then strain to go to the bathroom, which is painful and can lead to fissures.
- Eat a regular diet and avoid foods that are constipating; only you as an individual know what those foods are. Eat plenty of fresh fruits and vegetables. Avoid excessively hot and spicy foods that might burn on the way out.
- As mentioned, most of the discomfort and pain that people experience is related to bowel movements and is directly due to spasm or cramping of the sphincter muscle, which is irritated because of the raw areas that were burned. The best way to get immediate pain relief is to SOAK IN HOT WATER immersing your pelvis as opposed to just taking a "sitz bath" while sitting on the toilet. We recommend that you soak 6 to 8 TIMES PER DAY. Immediately after a bowel movement, you should soak. Soaking helps people to heal better and more quickly, often provides immediate relief of anal pain even when pain medications aren't helping, improves the blood supply to the area, and keeps it clean.
- Soak in hot water 6 to 8 times per day!
- Pain control is very important. Be sure to discuss this with your health care provider and let them know what medications work best for you. If you can take medications like ibuprofen or Advil or naprosyn or Aleve, these can be very helpful in decreasing the pain and inflammation and you should take them around the clock when you are not taking your other pain medication. They are also not constipating.
- Usually we prescribe extra strength Vicodin or hydrocodone, also known as Lortab, but some people require Percocet or oxycodone. It's important to realize that all of these pain medications contain acetaminophen or Tylenol and that patients should not take more than 4 grams per day, otherwise liver toxicity can occur. This translates to no more than eight (8) 500 mg tablets in a day. Patients with underlying liver disease such as chronic hepatitis should probably stay below this dose. Do not take extra Tylenol with these pain medications, but you can take Advil or Aleve.
- All pain medications containing narcotics are constipating, so if you find that you are requiring a lot of pain pills, then you may need to take more fiber or stool softeners. Again, the goal is to avoid constipation at all costs. If you haven't had a bowel movement in 2 or 3 days, then consider taking a laxative such as milk of magnesia.
- Unless patients have an allergy to sulfa drugs, they are sent home with a tube of Silvadene cream. This can be applied after bathing and is used to help decrease symptoms, because it is used for burn patients. If you find you would rather put the numbing jelly on and are not getting any relief from the Silvadene, then it's OK not to use it. Some people find as time passes after surgery that they begin to heal but still have external wounds that are slow to heal
- It is normal to have bleeding and oozing after surgery and often it occurs with bowel movements. Do not be frightened about this and realize that just a few drops of blood will turn the toilet bowel red. If you are continuously passing blood clots or dripping large amounts of blood that doesn't stop with rest and simple pressure, call your physician. Rarely after surgery patients will have bleeding that is significant enough to require a trip back to the operating room on an emergency basis, but this is very uncommon.
- If you had a lot of external disease treated, then you are more likely to have oozing and bleeding. Some people find that wearing feminine panty liners in their underwear can be helpful and cut down on the amount of laundry that needs to be done.
- Infection is very uncommon, but if you develop a fever greater than 101.5 degrees Fahrenheit, then call your physician. Occasionally in people who are prone to herpes outbreaks and are not receiving suppressive medication such as acyclovir or Valtrex, a herpes outbreak can be precipitated by the surgery. If this happens, it often occurs 5 to 7 days following the surgery and is recognized by the fact that just when things started to feel better, they suddenly begin to feel worse.
- Activity should be as tolerated, but we recommend that you take it easy for the first week or so depending on how you are feeling. You need time to allow your body to heal. You also need to be close to your bathtub to be able to soak. It's probably a good idea to avoid putting yourself in situations where you will have to stand or walk or sit for extended periods of time. As you begin to heal and the pain abates, you can begin to resume your normal activities. Heavy exercise in which you increase your intra-abdominal pressure such as heavy sit ups, squats and leg lifts should probably be avoided for several weeks because of the possibility of causing spontaneous bleeding by aggravating your hemorrhoids.
- The good news is everyone gets better; it just takes time. Sometime between 7 and 14 days, things begin to turn around and improve. That's a good sign that you will continue to get better on a daily basis, but don't push it too hard or too fast. Some people do amazingly well and have almost no pain and discomfort. Some people take little to no pain medications. Recovery is a very individual experience and seems to be somewhat different for everyone.
- We usually recommend that patients return to be examined 2 to 3 months following the surgery. This is ample time to allow healing and allow people to be examined without causing significant pain or discomfort. Continued follow-up is very important and you should continue to be monitored on a regular basis, because the HSIL can and frequently does recur. Frequent monitoring may catch it at a time when it can be treated in the office avoiding another operation.
- If you have anal sex, we also recommend that you wait 2 to 3 months before resuming receptive anal intercourse. It is important to start slowly, because scar tissue does not stretch as well or as quickly as normal skin and is more prone to tearing creating a fissure.
Read more about: Fissure Treatment Without Surgery

