Prostate biopsy Procedure
Prostate Biopsy
What is a Prostate Biopsy?
is Prostate Biopsy painthful?
A prostate biopsy is a procedure to remove samples of suspicious tissue from the prostate. The prostate is a small, walnut-shaped gland in men that produces fluid that nourishes and transports sperm.
During a prostate biopsy a needle is used to collect a number of tissue samples from your prostate gland. The procedure is performed by a doctor who specializes in the urinary system and men's sex organs (urologist).
Your urologist may recommend a prostate biopsy if results from initial tests, such as a prostate-specific antigen (PSA) blood test or digital rectal exam, suggest you may have prostate cancer. Tissue samples from the prostate biopsy are examined under a microscope for cell abnormalities that are a sign of prostate cancer. If cancer is present, it is evaluated to determine how quickly it's likely to progress and to determine your best treatment options.
Read more about : Prostate Biopsy Procedure Types(anesthesia)
Read more about : Pancreatic cancer
Read more about : Prostate Cancer Treatments Pros and Cons
Before Prostate Biopsy
Why it's done
A prostate biopsy is used to detect prostate cancer.
Your doctor may recommend a prostate biopsy if:
. A PSA test shows levels higher than normal for your age
. Your doctor finds lumps or other abnormalities during a digital rectal exam
. You've had a previous biopsy that was normal, but you still have elevated PSA levels
. A previous biopsy revealed prostate tissue cells that were abnormal but not cancerous.
Advantages and disadvantages of having a prostate biopsy
Your doctor should talk to you about the advantages and disadvantages of having a biopsy. If you have any concerns, discuss them with your doctor or specialist nurse before you decide whether to have a biopsy.
Advantages
. It’s the only way to find out for certain if you have cancer inside your prostate.
. It can help find out how aggressive any cancer might be – in other words, how likely it is to spread.
. It can pick up a faster growing cancer at an early stage, when treatment may prevent the cancer from spreading to other parts of the body.
. If you have prostate cancer, it can help your doctor or nurse decide which treatment options may be suitable for you.
. If you have prostate cancer, you’ll usually need to have had a biopsy if you want to join a clinical trial in the future. This is because the researchers may need to know what your cancer was like when it was first diagnosed.
Disadvantages
. The biopsy can only show whether there was cancer in the samples taken, so it’s possible that cancer might be missed.
. It can pick up a slow growing or non-aggressive cancer that might not cause any symptoms or problems in your lifetime. You’d then have to decide whether to have treatment or whether to have your cancer monitored. Treatment can cause side effects that can be hard to live with. But having your cancer monitored rather than having treatment might make you worry about your cancer.
. A biopsy has side effects and risks, including the risk of getting a serious infection.
. If you take medicines to thin your blood, you may need to stop taking them for a while, as the biopsy can cause some bleeding for a couple of weeks.
Read more about : Cancer Treatment
Read more about : Pancreatic Cancer Stages
How do I get ready for a prostate biopsy?
Some things you can expect before a prostate biopsy include:
. Your healthcare provider will explain the procedure and you can ask questions.
. You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if anything is not clear.
. Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, and anesthesia.
. Make sure your healthcare provider has a list of all medicines (prescription and over-the-counter) and all herbs, vitamins, and supplements that you are taking.
. Tell your healthcare provider if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medicines, aspirin, or other medicines that affect blood clotting. You may need to stop these medicines before the procedure.
. Generally, no prior preparation, such as fasting or sedation, is needed for the transrectal or perineal method. If the transurethral method is to be used, general anesthesia may be used. If you are to have general anesthesia, you may be told to fast (not eat or drink anything) before the procedure, generally after midnight. Your healthcare provider will give you specific instructions.
. If your healthcare provider uses the transrectal method, you may need to use an enema the night before or the morning of the biopsy.
. You may get a sedative before the procedure to help you relax. Because the sedative may make you drowsy, you will need to arrange for someone to drive you home. You will most likely get a sedative if your healthcare provider is using the transurethral method.
. You may start to take antibiotics the day before the biopsy is done and continue them for a few days after it. This is to help prevent infection.
. Provide a urine sample to analyze for a urinary tract infection. If you have a urinary tract infection, your prostate biopsy will likely be postponed while you take antibiotics to clear the infection.
. Follow any other instructions your healthcare provider gives you to get ready.
Read more about : Orchiectomy surgery for prostate cancer
Complications and Side effects
Side effects of a prostate biopsy
Having a biopsy can cause side effects. These will affect each man differently, and you may not get all of the possible side effects.
. Pain or discomfort
Some men feel pain or discomfort in their back passage (rectum) for a few days after a TRUS biopsy. Others feel a dull ache along the underside of their penis or lower abdomen (stomach area). If you have a transperineal biopsy, you may get some bruising and discomfort in the area where the needle went in for a few days afterwards.
If you receive anal sex, wait about two weeks, or until any pain or discomfort from your biopsy has settled, before having sex again. Ask your doctor or nurse at the hospital for further advice.
Some men find the biopsy painful, but others have only slight discomfort. Your nurse or doctor may suggest taking mild pain-relieving drugs, such as paracetamol, to help with any pain.
If you have any pain or discomfort that doesn’t go away, talk to your nurse or doctor.
. Short-term bleeding
It’s normal to see a small amount of blood in your urine or bowel movements for about two weeks. You may also notice blood in your semen for a couple of months – it might look red or dark brown. This is normal and should get better by itself. If it takes longer to clear up, or gets worse, you should see a doctor straight away.
A small number of men (less than 1 in 100) who have a TRUS biopsy may have more serious bleeding in their urine or from their back passage (rectum). This can also happen if you have a transperineal biopsy but it isn't very common. If you have severe bleeding or are passing lots of blood clots, this is not normal. Contact your doctor or nurse at the hospital straight away, or go to the accident and emergency (A&E) department at the hospital.
. Infection
Some men get an infection after their biopsy. This is more likely after a TRUS biopsy than after a transperineal biopsy. It's very important to take any antibiotics you’re given, as prescribed, to help prevent this. But you might still get an infection even if you take antibiotics.
Symptoms of a urine infection may include:
. Pain or a burning feeling when you urinate
. Dark or cloudy urine with a strong smell
. Needing to urinate more often than usual
. Pain in your lower abdomen (stomach area).
If you have any of these symptoms, contact your doctor or nurse at the hospital straight away. If you can’t get in touch with them, call your GP.
Around 3 in 100 men (three per cent) who have a TRUS biopsy get a more serious infection that requires going to hospital. If the infection spreads into your blood, it can be very serious. This is called sepsis. Symptoms of sepsis may include:
. A high temperature (fever)
. Chills and shivering
. A fast heartbeat
. Fast breathing
. Confusion or changes in behaviour.
If you have symptoms of sepsis, go to your nearest hospital A&E department straight away.
. Acute urine retention
A small number of men find them suddenly and painfully can’t urinate after a biopsy – this is called acute urine retention. This happens because the biopsy can cause the prostate to swell, making it difficult to urinate. Acute urine retention may be more likely if you have a template biopsy. This is because more samples are taken, so there may be more swelling.
Your doctor will make sure you can urinate before you go home after your biopsy. If you can’t urinate, you might need to have a catheter for a few days at home – this is a thin tube that’s passed into your bladder to drain urine out of the body.
If you develop acute urine retention at home, contact your doctor or nurse at the hospital straight away, or go to your nearest A&E department. You might need a catheter for a few days.
. Sexual problems
You can masturbate and have sex after a biopsy. If you have blood in your semen, you might want to use a condom until the bleeding stops.
A small number of men have problems getting or keeping an erection (erectile dysfunction) after having a biopsy. This may happen if the nerves that control erections are damaged during the biopsy. It isn’t very common and it should get better over time, usually within two months. Speak to your doctor or nurse if you’re worried about this.
During Prostate Biopsy
Types of prostate biopsy
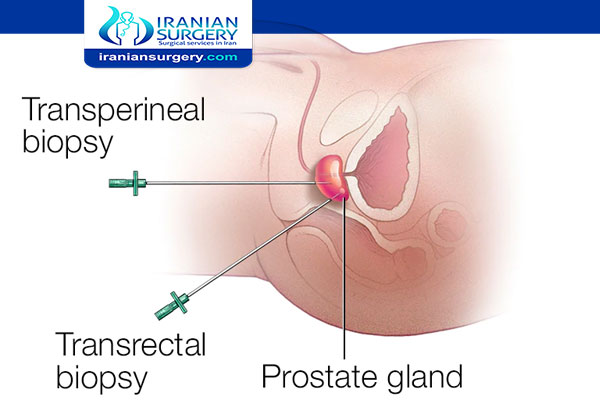
Prostate biopsy samples can be collected in different ways. Your prostate biopsy may involve:
. Transrectal ultrasound-guided (TRUS) biopsy. This is the most common type of prostate biopsy. An ultrasound probe is put into your rectum to create a scan (picture) of your prostate. Your doctor takes several small biopsies (tissue samples) using a needle which goes next to the probe. They’ll first inject some local anaesthetic to numb the area around your prostate. The procedure usually takes 20 to 30 minutes and you can go home afterwards.
. Transperineal biopsy. This type of biopsy is becoming more widely available than it used to be. Your doctor will insert biopsy needles through the skin in the area between your testicles and rectum (this area is called your perineum). They’ll put an ultrasound probe into your rectum to help guide them to the right spot. You’ll have either a general anaesthetic so you’ll be asleep, or a spinal anaesthetic so you’ll be numb from the waist down. Or you may be able to have the procedure under a local anaesthetic, which numbs the area. You may be in hospital for a day. An MRI or CT scan is generally used to guide this procedure.
During prostate biopsy
. During Transrectal ultrasound-guided (TRUS) biopsy
The doctor or nurse uses a thin needle to take small samples of tissue from the prostate.
You’ll lie on your side on an examination table, with your knees brought up towards your chest. The doctor or nurse will put an ultrasound probe into your back passage (rectum), using a gel to make it more comfortable. The ultrasound probe scans the prostate and an image appears on a screen. The doctor or nurse uses this image to guide where they take the cells from. If you’ve had an MRI scan, the doctor or nurse may use the images to decide which areas of the prostate to take biopsy samples from.
You will have an injection of local anaesthetic to numb the area around your prostate and reduce any discomfort. The doctor or nurse then puts a needle next to the probe in your back passage and inserts it through the wall of the back passage into the prostate. They usually take 10 to 12 small pieces of tissue from different areas of the prostate. But, if the doctor is using the images from your MRI scan to guide the needle, they may take fewer samples.
. During Transperineal biopsy
This is where the doctor inserts the biopsy needle into the prostate through the skin between the testicles and the back passage (perineum). In the past, hospitals would only offer a transperineal biopsy if other health problems meant you couldn’t have a TRUS biopsy. But many hospitals have stopped doing TRUS biopsies and now only do transperineal biopsies.
A transperineal biopsy is normally done under general anaesthetic, so you will be asleep and won’t feel anything. A general anaesthetic can cause side effects – your doctor or nurse should explain these before you have your biopsy. Some hospitals now do transperineal biopsies using a local anaesthetic, which numbs the prostate and the area around it, or a spinal (epidural) anaesthetic, where you can’t feel anything in your lower body.
The doctor will put an ultrasound probe into your back passage, using a gel to make this easier. An image of the prostate will appear on a screen, which will help the doctor to guide the biopsy needle.
If you’ve had an MRI scan, the doctor may just take a few samples from the area of the prostate that looked unusual on the scan images. This is known as a targeted biopsy.
Or they might decide to take up to 25 samples from different areas of the prostate. You may hear this called a template biopsy, as the doctor places a grid (template) over the area of skin between the testicles and back passage. They then insert the needle through the holes in the grid, into the prostate. A template biopsy is sometimes used if a TRUS biopsy hasn’t found any cancer, but the doctor still thinks there might be cancer.
A transperineal biopsy usually takes about 20 to 40 minutes. If you've had a general anaesthetic, you will need to wait a few hours to recover from the anaesthetic before going home. And you will need to get someone to take you home. Your doctor may ask you to wait until you’ve urinated. This is because the biopsy can cause the prostate to swell, so they’ll want to make sure you can urinate properly before you leave.
What are the alternatives to a prostate biopsy?
Your doctor will take into account your previous test results and your individual circumstances and risk factors when deciding what to recommend as your next steps. For example, rather than suggesting a prostate biopsy, your doctor may keep an eye on your symptoms and do regular blood tests.
In many hospitals, you may have a special type of magnetic resonance imaging (MRI) scan before or instead of having a prostate biopsy. This is called a multi-parametric MRI (mpMRI) scan. The mpMRI scan may help your doctor decide if you need a prostate biopsy or your cancer needs treating.
After Prostate Biopsy
What to expect after a prostate biopsy
After your prostate biopsy, you’ll usually need to stay at the hospital for at least 30 minutes until the anaesthetic wears off. Your doctor may also ask you to wait until you’re able to pee properly. This is because a biopsy can make your prostate gland swell up for a while, which can make it harder to pee.
Your doctor or nurse may give you antibiotics and a date for a follow-up appointment to discuss your results. They should also give you a number to call and information about who to contact if you have problems in the first few days after your biopsy.
You shouldn’t drive straight away after a prostate biopsy, so make sure you arrange for someone to take you home.
Recovering from a prostate biopsy
Your prostate gland may feel a bit bruised after the procedure. If you need pain relief, you can take over-the-counter painkillers such as paracetamol. Always read the patient information that comes with your medicine. If you have any questions, ask your pharmacist for advice.
You should be able to get back to your usual activities almost straight away but take it easy for a couple of days. Drink plenty of fluids – perhaps twice as much as you normally would.
It’s normal to have some blood in your urine, poo and semen after a prostate biopsy so don’t be alarmed if you do.
If you’ve been given antibiotics, it’s important that you complete the full course to help prevent an infection. Contact the hospital (or if out of hours the hospital emergency department) if you have:
. Bad pain or discomfort that doesn’t go away
. Difficulty peeing
. A burning feeling when you pee
. Smelly urine
. Increasing amounts of blood in your urine or poo
If you get a high temperature, especially with uncontrollable shivers and chills, seek medical advice straight away. This may mean you have an infection and will need stronger antibiotics.
How soon after a prostate biopsy can I have sex?
You can usually have sex straight away after a prostate biopsy, as long as you feel well enough. If you’re unsure, ask your doctor about this when you have your biopsy.
You may have some blood in your semen for up to six weeks after your biopsy. This won’t harm you or your partner, but you may wish to use condoms until the bleeding stops.
How soon can I exercise after a prostate biopsy?
Everyone recovers differently from a prostate biopsy. As long as you don’t have any complications, you should be able to get back to your usual activities straight away. But if you have any pain and discomfort around your rectum after the procedure, you may wish to rest for a while afterwards.
When you have your biopsy, ask your doctor about getting back to exercise and sporting activities. They’ll be able to discuss what’s right for you. If you have more pain or bleeding after exercising, contact the hospital.
Results
A doctor who specializes in diagnosing cancer and other tissue abnormalities (pathologist) will evaluate the prostate biopsy samples. The pathologist can tell if the tissue removed is cancerous and, if cancer is present, estimate how aggressive it is. Your doctor will explain the pathologist's findings to you.
Your pathology report may include:
. A description of the biopsy sample. Sometimes called the gross description, this section of the report might evaluate the color and consistency of the prostate tissue.
. A description of the cells. Your pathology report will describe the way the cells appear under the microscope. Prostate cancer cells may be referred to as adenocarcinoma. Sometimes the pathologist finds cells that appear abnormal but aren't cancerous. Words used to describe these noncancerous conditions include "prostatic intraepithelial neoplasia" and "atypical small acinar proliferation."
. Cancer grading. If the pathologist finds cancer, it's graded on a scale of 2 to 10 called the Gleason score. Cancers with a high Gleason score are the most abnormal and are more likely to grow and spread quickly.
. The pathologist's diagnosis. This section of the pathology report lists the pathologist's diagnosis. It may also include comments, such as whether other tests are recommended.
It can take up to two weeks to get the results of the biopsy. Ask your doctor or nurse when you're likely to get the results. You might be sent a copy of the pathology report. And you can ask to see copies of letters between the hospital and your GP. If you have trouble understanding any of the information, ask your doctor to explain it or speak to our Specialist Nurses.
How accurate is a prostate biopsy?
No diagnostic test is completely accurate. Doctors usually take several samples of your prostate tissue during the biopsy, which increases the chances of finding any cancer. But sometimes the biopsy still misses cancerous cells. Or sometimes the biopsy will find a very slow-growing cancer that wouldn’t have caused you any problems in your lifetime.
If the doctors don’t find any cancer in the biopsy samples, this is likely to be reassuring. But your doctor will discuss the results with you as it doesn’t definitely mean that you don’t have prostate cancer. There could be a small cancer that the biopsy needles didn’t reach.
Your doctor may keep monitoring your prostate with further prostate specific antigen (PSA) tests to see if anything changes in the future. If your PSA continues to rise, your doctor may recommend you have another biopsy or an MRI scan.
Read more about: prostate biopsy bleeding
Read more about: prostate biopsy preparation

