Phalloplasty
What is Phalloplasty?
A phalloplasty is the construction or reconstruction of a penis. The phalloplasty is a common surgical choice for transgender and nonbinary people interested in gender confirmation surgery. It’s also used to reconstruct the penis in cases of trauma, cancer, or congenital defect.
The goal of a phalloplasty is to build a cosmetically appealing penis of sufficient size that is capable of feeling sensations and releasing urine from a standing position. It’s a complex procedure that often involves more than one surgery.
Read more about : Penis enlargement
Read more about : Penile Curvature Deformity
Read more about : Penile Curvature
Read more about : Chordee
Before Phalloplasty
Who needs phalloplasty?
People with gender dysphoria undergoing female-to-male (FtM) gender confirmation surgery. It’s also for those who have:
Congenital (present at birth) conditions, such as:
. Ambiguous genitalia.
. Aphalia, which occurs when a person is born without a penis.
. Epispadias, a rare condition in which urine exits the body from the top of the penis instead of the tip.
. Hypospadias.
. Micropenis.
Experienced trauma affecting their penis, including:
. Burns.
. Car accidents.
. Circumcision complications.
. Explosions.
. Penile fracture due to sudden bending during an erection.
Where will the tissue for the neopenis come from?
Tissue flaps may come from your:
. Forearm: Radial forearm free flap.
. Thigh: Anterolateral thigh free flap.
. Back: Latissimus dorsi myocutaneous flap.
How do I prepare for penis surgery?
Before surgery, you'll undergo assessments and testing. These may include:
. Physical exam to assess your health and learn more about your medical history.
. Genital hair removal, which starts months before surgery.
. Patient education about risks, benefits and postsurgical care requirements.
. Mental health evaluation to ensure your understanding of the procedure. Healthcare providers also explain its impact on your life.
. Recommendations, including quitting smoking and losing weight, which lower your risk of complications.
What are the benefits of phalloplasty?
One of the main benefits of phalloplasty is relief from physical and emotional challenges. Results include a natural-looking penis that may be capable of erections. When part of transgender surgery, phalloplasty helps you achieve your desired gender identity.
Read more about : Virgin tightening surgery before and after pictures
Other benefits depend on which options you choose:
. Radial forearm free flaps provide excellent cosmetic results and better sensation.
. Anterolateral thigh free flaps give you more penis length options. And the scars on your thigh from removing the flap are easier to hide.
. Latissimus dorsi flaps (from your back) cause less scarring. They offer the best potential for an erection without a device.
. Urethra lengthening enables you to urinate while standing.
Risks and Complications
Phalloplasty, like all surgeries, comes with the risk of infection, bleeding, tissue damage, and pain. Unlike some other surgeries, however, there is a fairly high risk of complications associated with phalloplasty. The most commonly occurring complications involve the urethra.
Possible phalloplasty complications include:
. Urethral fistulas
. Urethral stricture (a narrowing of the urethra that obstructs urinary flow)
. Flap failure and loss (the death of the transferred tissue)
. Wound breakdown (ruptures along the incision lines)
. Pelvic bleeding or pain
. Bladder or rectal injury
. Lack of sensation
. Prolonged need for drainage (discharge and fluid at wound site requiring dressings)
The donation site is also at risk for complications, these include:
. Unsightly scarring or discoloration
. Wound breakdown
. Tissue granulation (red, bumpy skin at wound site)
. Decreased mobility (rare)
. Bruising
. Decreased sensation
. Pain
Read more about : Male to female surgery
During Phalloplasty
What happens during a phalloplasty?
During a phalloplasty, doctors remove a flap of skin from a donor area of your body. They might remove this flap entirely or leave it partially attached. This tissue is used to make both the urethra and the shaft of the penis, in a tube-within-a-tube structure. The larger tube is basically rolled up around the inside tube. Skin grafts are then taken from inconspicuous areas of the body, where they will leave no visible scars, and grafted on to the donation site.
The female urethra is shorter than the male urethra. Surgeons can lengthen the urethra and attach it to the female urethra so that urine will flow from the tip of the penis. The clitoris is usually left in place near the base of the penis, where it can still be stimulated. People who can achieve orgasm before their surgery can usually still do so after their surgery.
A phalloplasty, specifically, is when surgeons turn a flap of donor skin into a phallus. But generally, it refers to a number of separate procedures that are often done in tandem. These procedures include:
. A hysterectomy, during which doctors remove the uterus
. An oophorectomy to remove the ovaries
. A vaginectomy or vaginal mucosal ablation to remove or partially remove the vagina.
. A phalloplasty to turn a flap of donor skin into a phallus
. A scrotectomy to turn the labia majora into a scrotum, either with or without testicular implants.
. An urethroplasty to lengthen and hook up the urethra inside the new phallus
. A glansplasty to sculpt the appearance of an uncircumcised tip
. A penile implant to allow for erection
There is no single order or timeline for these procedures. Many people do not do all of them. Some people do some of them together, while others spread them out over many years. These procedures require surgeons from three different specialties: gynecology, urology, and plastic surgery.
When looking for a surgeon, you may want to look for one with an established team. Before any of these medical interventions, talk to your doctor about fertility preservation and impact on sexual functioning.
Phalloplasty Techniques
The difference between the prevailing phalloplasty techniques is the location from which the donor skin is taken and the way in which it is removed and reattached. Donor sites can include the lower abdomen, groin, torso, or thigh. However, the preferred site of most surgeons is the forearm.
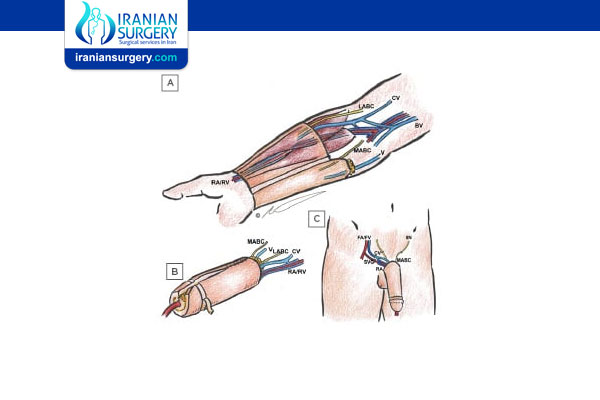
. Radial forearm free-flap phalloplasty
The radial forearm free-flap (RFF or RFFF) phalloplasty is the most recent evolution in genital reconstruction. In a free flap procedure, the tissue is completely removed from the forearm with its blood vessels and nerves intact. These blood vessels and nerves are reattached with microsurgical precision, allowing blood to flow naturally to the new phallus.
This procedure is preferred to other techniques because it provides excellent sensitivity along with good aesthetic results. The urethra can be constructed in a tube-within-a-tube fashion, allowing for standing urination. There is room for the later implantation of an erection rod or inflatable pump.
The chances of mobility damage to the donor-site are also low, however skin grafts to the forearm often leave moderate to severe scarring. This procedure is not ideal for someone worried about visible scars.
. Anterior lateral thigh pedicled flap phalloplasty
The anterior lateral thigh (ALT) pedicled flap phalloplasty is not the leading choice of most surgeons because it results in a much lower level of physical sensitivity in the new penis. In a pedicled flap procedure, the tissue is separated from the blood vessels and nerves. The urethra can be restructured for standing urination, and there is ample room for a penile implant.
Those who have undergone this procedure are generally satisfied, but report low levels of erotic sensitivity. There is a higher rate of urinary and other complications with this procedure than with RFF. The skin grafts can leave significant scaring, but in a more discrete place.
. Abdominal phalloplasty
The abdominal phalloplasty, also called the supra-pubic phalloplasty, is a good choice for trans men who don’t require a vaginectomy or a restructured urethra. The urethra will not go through the tip of the penis and urination will continue to require a seated position.
Like the ALT, this procedure does not require microsurgery, so it is less expensive. The new phallus will have tactile, but not erotic sensation. But the clitoris, which is preserved in its original location or buried, can still be stimulated, and a penile implant can allow for penetration.
The procedure leaves a horizontal scar stretching from hip to hip. This scar is easily hidden by clothing. Because it does not involve the urethra, it is associated with fewer complications.
. Musculocutaneous latissimus dorsi flap phalloplasty
A musculocutaneous latissimus dorsi (MLD) flap phalloplasty takes donor tissue from the back muscles underneath the arm. This procedure provides a large flap of donor tissue, which allows surgeons to create a larger penis. It is well-suited for both a restructuring of the urethra and the addition of an erectile device.
The flap of skin includes blood vessels and nerve tissue, but the single motor nerve is less erotically sensitive than the nerves connected with RFF. The donor site heals well and is not nearly as noticeable as other procedures.
After Phalloplasty
Recovery
You should be able to go back to work about four to six weeks after your phalloplasty, unless your job requires strenuous activity. Then you should wait six to eight weeks. Avoid exercise and lifting during the first few weeks, although taking a brisk walk is fine. You will have a catheter in place for the first few weeks. After two to three weeks you can start to urinate through the phallus.
Your phalloplasty may be broken into stages, or you may have the scrotoplasty, urethral reconstruction, and glansplasty simultaneously. If you separate them, you should wait at least three months between the first and second stages. For the final stage, which is the penile implant, you should wait for about one year. It is important that you have full feeling in your new penis before getting your implant.
Depending on which type of surgery you had, you may never have erotic sensation in your phallus (but you can still have clitoral orgasms). It takes a long time for nerve tissue to heal. You may have tactile sensation before erotic sensation. Full healing can take up to two years.
Aftercare
. Avoid putting pressure on the phallus.
. Try to elevate the phallus to decrease swelling and improve circulation (prop it up on a surgical dressing).
. Keep incisions clean and dry, reapply dressings, and wash with soap and water as directed by your surgeon.
. Do not apply ice to the area.
. Keep the area around drains clean with a sponge bath.
. Do not shower for the first two weeks, unless your doctor tells you otherwise.
. Do not pull at the catheter, as this could damage the bladder.
. Empty the urine bag at least three times per day.
. Do not try to urinate from your phallus before you are supposed to.
. Itching, swelling, bruising, blood in the urine, nausea, and constipation are all normal in the first few weeks.
. Limiting physical activity, like exercise, work and household chores.
. Taking medications to ease pain, prevent infection and relieve constipation.
. Eliminating urine through a thin tube inserted into the penis (Foley catheter) or through the skin of the lower abdomen (suprapubic catheter).
How long will it take to achieve a functioning penis?
Achieving the full function of your penis takes time — in some cases, a year or more. It may require multiple surgeries. The length of your recovery depends in part on whether surgery involves:
. Repairing or constructing a penis.
. Removing female genitals.
. Taking a flap from the arm, leg or back.
. Constructing a scrotum or glans.
. Implanting a device to create erections.
When should I contact my healthcare provider after having phalloplasty?
Your care should include follow-up appointments to track your recovery. Contact your healthcare provider immediately if you experience:
. Blood-soaked dressings, which can be a sign of excessive bleeding.
. Infections that cause a fever or yellowish discharge from the incision.
. Pain that does not respond to medications.
. Signs of blood clots, such as abnormal swelling in your groin or lower leg.
. Vomiting and not being able to keep fluids down.
. If the neopenis appears discolored or if there are skin changes.
Outlook
While phalloplasty techniques have improved over the years, there is still no optimal procedure. Do a ton of research and talk to people in the community before making a decision about which type of bottom surgery is right for you. There are alternatives to phalloplasty, including packing and a less risky procedure called a metoidioplasty.
Phalloplasty Cost
The cost of Phalloplasty in Iran is $ 6000.

