Dacryocystorhinostomy (DCR) Surgery
What is Blocked Tear Duct?
When you have a blocked tear duct, your tears can't drain normally, leaving you with a watery, irritated eye. The condition is caused by a partial or complete obstruction in the tear drainage system.
A blocked tear duct is common in newborns. The condition usually gets better without any treatment during the first year of life. In adults a blocked tear duct may be due to an injury, an infection or a tumor.
A blocked tear duct is almost always correctable. Treatment depends on the cause of the blockage and the age of the affected person.
What is Dacryocystorhinostomy (DCR) Surgery?
A dacryocystorhinostomy (DCR) is a type of surgery done to create a new tear drain between your eyes and your nose. You may need this surgery if your own tear duct has become blocked.
Read more about : Glaucoma symptoms
Read more about : Cataract
Read more about : Can a chalazion come back after surgery?
Read more about : How to Put in and Remove Contact Lenses?
Read more about : Eye color change surgery
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Surgeons to treat blocked tear duct in Iran. The price of treating a blocked tear duct in Iran can vary according to each individual’s case and will be determined by the type of treatment you have and an in-person assessment with the doctor. So if you are looking for the cost of Dacryocystorhinostomy (DCR) Surgery in Iran, you can contact us and get free consultation from Iranian surgery.

Before Dacryocystorhinostomy (DCR) Surgery
Symptoms
Signs and symptoms of a blocked tear duct
Signs and symptoms of a blocked tear duct include:
. Excessive tearing
. Redness of the white part of the eye
. Recurrent eye infection or inflammation (pink eye)
. Painful swelling near the inside corner of the eye
. Crusting of the eyelids
. Mucus or pus discharge from the lids and surface of the eye
. Blurred vision
Read more about : Lasik Eye Surgery
Read more about : Cat Eye Surgery
When to see a doctor
See your doctor if you tear constantly for several days or if your eye is repeatedly or continually infected. A blocked tear duct may be caused by a tumor pressing on the tear drainage system. Early identification of the tumor can give you more treatment options.
Causes
Blocked tear ducts can happen at any age. They may even be present at birth (congenital). Causes include:
. Congenital blockage. Many infants are born with a blocked tear duct. The tear drainage system may not be fully developed or there may be a duct abnormality. Often a thin tissue membrane remains over the opening that empties into the nose (nasolacrimal duct).
. Age-related changes. As you age, the tiny openings that drain tears (puncta) may get narrower, causing blockage.
. Infection or inflammation. Chronic infection or inflammation of your eyes, tear drainage system or nose can cause your tear ducts to become blocked.
. Injury or trauma. An injury to your face can cause bone damage or scarring near the drainage system, disrupting the normal flow of tears through the ducts. Even small particles of dirt or loose skin cells lodged in the duct can cause blockage.
. Tumor. A tumor in the nose or anywhere along the tear drainage system can cause blockage.
. Inflammatory conditions. Disorders that cause swelling, such as sarcoidosis or granulomatosis with polyangiitis, can increase the risk of developing a blocked tear duct.
. Eyedrops. Rarely, long-term use of certain medications, such as eyedrops used to treat glaucoma, can cause a blocked tear duct.
. Cancer treatments. A blocked tear duct is a possible side effect of chemotherapy medication and radiation treatment for cancer.
How the tear drainage system works
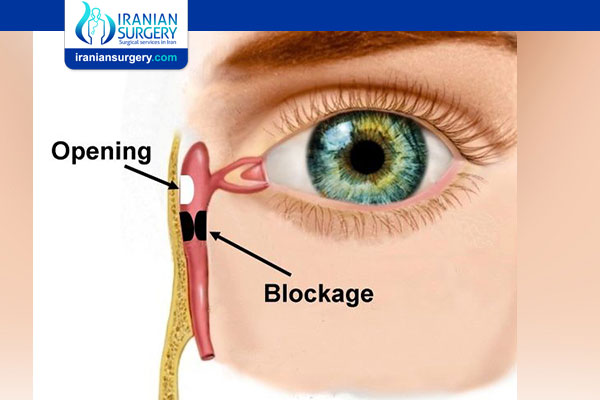
The lacrimal glands produce most of your tears. These glands are located inside the upper lids above each eye. Normally, tears flow from the lacrimal glands over the surface of your eye. Tears drain into the puncta, located in the inside corners of your upper and lower eyelids.
Your eyelids have small canals (canaliculi) that move tears to a sac where the lids are attached to the side of the nose (lacrimal sac). From there tears travel down a duct (the nasolacrimal duct) draining into your nose. Once in the nose, tears are reabsorbed.
A blockage can occur at any point in the tear drainage system, from the puncta to your nose. When that happens, your tears don't drain properly, giving you watery eyes and increasing your risk of eye infections and inflammation.
Read more about : Lasik Eye Surgery
Read more about : Cat Eye Surgery
Risk factors
Certain factors increase your risk of developing a blocked tear duct:
. Age and sex. Older women are at highest risk of developing blocked tear ducts due to age-related changes.
. Chronic eye inflammation. If your eyes are continually irritated, red and inflamed (conjunctivitis), you're at higher risk of developing a blocked tear duct.
. Previous surgery. Previous eye, eyelid, nasal or sinus surgery may have caused some scarring of the duct system, possibly resulting in a blocked tear duct later.
. Glaucoma. Anti-glaucoma medications are often used topically on the eye. If you've used these or other topical eye medications, you're at higher risk of developing a blocked tear duct.
. Previous cancer treatment. If you've had radiation or chemotherapy to treat cancer, particularly if the radiation was focused on your face or head, you're at higher risk of developing a blocked tear duct.
Complications
Because your tears aren't draining the way they should, the tears that remain in the drainage system become stagnant. This promotes growth of bacteria, viruses and fungi, which can lead to recurrent eye infections and inflammation.
Any part of the tear drainage system, including the clear membrane over your eye surface (conjunctiva), can become infected or inflamed because of a blocked tear duct.
Read more about : Heart Valve Replacement Surgery
Read more about : Keratoconus Treatment
Read more about : Epi-Lasik Eye Surgery
Diagnosis
To diagnosis your condition, your doctor talks with you about your symptoms, examines your eyes and does a few tests. He or she will also examine the inside of your nose to determine if any structural disorders of your nasal passages are causing an obstruction. If your doctor suspects a blocked tear duct, he or she may have you undergo other tests to find the location of the blockage.
Tests used to diagnose a blocked tear duct include:
. Tear drainage test. This test measures how quickly your tears are draining. One drop of a special dye is placed on the surface of each eye. You may have a blocked tear duct if after five minutes most of the dye is still on the surface of your eye.
. Irrigation and probing. Your doctor may flush a saline solution through your tear drainage system to check how well it's draining. Or he or she may insert a slender instrument (probe) through the tiny drainage holes at the corner of your lid (puncta) to check for blockages. In some cases this probing may even fix the problem.
. Eye imaging tests. For these procedures, a contrast dye is passed from the puncta in the corner of your lid through your tear drainage system. Then X-ray, computerized tomography (CT) or magnetic resonance imaging (MRI) images are taken to find the location and cause of the blockage.
Why might I need a Dacryocystorhinostomy (DCR) Surgery?
The procedure is done to relieve the symptoms of a blocked tear duct. These include excessive eye watering or crusting around your eye. If the duct is infected, you might have the following symptoms:
. Swelling and tenderness around your eye
. Eye irritation
. Mucous discharge
Not everyone who has a blocked tear duct needs a DCR. A DCR is a much more common treatment for adults than for children. Your healthcare provider might first recommend less invasive treatments. These may include warm compresses, massage, and antibiotics for an infection. Or a healthcare provider might advise a procedure to try to dilate the nasolacrimal duct. If your symptoms are severe, however, you may need a DCR.
Depending on the cause of your blocked tear duct, you may need another treatment. You may need a different kind of surgery if a tumor blocks your duct.
You and your healthcare provider may also need to discuss what type of DCR will be best for you. Sometimes, healthcare providers perform the procedure externally. Other times, they use a rigid tube inserted into the nasal cavity to perform the surgery. With this approach, you may be able to avoid having an external scar. Ask your eye doctor about the benefits and risks of all your treatment options.
What are the risks of a Dacryocystorhinostomy (DCR) Surgery?
All procedures have risks. Some possible risks of this procedure include:
. Abnormally fused tissue in the nose
. Displacement of the stent placed in the duct
. Excess bleeding
. Infection
. Prominent facial scar
There is also a risk that the DCR will not be effective.
Your risks may differ according to your age, your other health conditions, the type of DCR performed, and the reasons for it. Talk with your doctor about all your concerns and about the risks that are most applicable to you.
Prevention
To reduce your risk of developing a blocked tear duct later in life, get prompt treatment of eye inflammation or infections. Follow these tips to avoid eye infections in the first place:
. Wash your hands thoroughly and often.
. Try not to rub your eyes.
. Replace your eyeliner and mascara regularly. Never share these cosmetics with others.
If you wear contact lenses, keep them clean according to recommendations provided by the manufacturer and your eye care specialist.
During Dacryocystorhinostomy (DCR) Surgery
Treatment
Your treatment depends on what's causing the blocked tear duct. You may need more than one approach to correct the problem. If a tumor is causing your blocked tear duct, treatment will focus on the cause of the tumor. Surgery may be performed to remove the tumor, or your doctor may recommend using other treatments to shrink it.
. Medications to fight infection. If your doctor suspects an infection is present, he or she may prescribe antibiotic eyedrops or pills.
. Watch-and-wait or massage. Babies born with a blocked tear duct often get better without any treatment. This can happen as the drainage system matures during the first couple months of life. Often a thin tissue membrane remains over the opening that empties into the nose (nasolacrimal duct). If your baby's blocked tear duct isn't improving, his or her doctor may teach you a special massage technique to help open the membrane.
If you've had a facial injury that caused blocked tear ducts, your doctor may suggest waiting a few months to see if the condition improves as your injury heals. As the swelling goes down, your tear ducts may become unblocked on their own.
. Dilation, probing and flushing. For infants, this technique is done under general anesthesia. The doctor enlarges the punctal openings with a special dilation instrument and inserts a thin probe through the puncta and into the tear drainage system.
For adults with partially narrowed puncta, your doctor may dilate the puncta with a small probe and then flush (irrigate) the tear duct. This is a simple outpatient procedure that often provides at least temporary relief.
. Balloon catheter dilation. If other treatments haven't worked or the blockage returns, this procedure may be used. It's usually effective for infants and toddlers, and may also be used in adults with partial blockage. First the patient is given a general anesthetic. Then the doctor threads through the tear duct blockage in the nose a tube (catheter) with a deflated balloon on the tip. He or she inflates and deflates the balloon a few times to open the blockage.
. Stenting or intubation. This procedure is usually done using general anesthesia. A thin tube, made of silicone or polyurethane, is threaded through one or both puncta in the corner of your eyelid. These tubes then pass through the tear drainage system into your nose. A small loop of tubing will stay visible in the corner of your eye, and the tubes are generally left in for about three months before they're removed. Possible complications include inflammation from the presence of the tube.
Surgery
The surgery that's commonly used to treat blocked tear ducts is called dacryocystorhinostomy. This procedure opens the passageway for tears to drain out your nose again. First you're given a general anesthetic, or a local anesthetic if it's performed as an outpatient procedure. The procedure takes about one hour.
The steps in this procedure vary, depending on the exact location and extent of your blockage, as well as your surgeon's experience and preferences.
. External. With external dacryocystorhinostomy, your surgeon makes an incision on the side of your nose, near where the lacrimal sac is located. After connecting the lacrimal sac to your nasal cavity and placing a stent in the new passageway, the surgeon closes up the skin incision with a few stitches.
. Endoscopic or endonasal. With this method, your surgeon uses a microscopic camera and other tiny instruments inserted through the nasal opening to your duct system. This method requires no incision so leaves no scar. But the success rates aren't as high as with the external procedure.
Following surgery you'll use a nasal decongestant spray and eyedrops to prevent infection and reduce inflammation. After three to six months, you'll return to your doctor's office for removal of any stents used to keep the new channel open during the healing process.
Read more about: Glaucoma treatment
After Dacryocystorhinostomy (DCR) Surgery
What happens after Dacryocystorhinostomy (DCR) surgery?
After a DCR procedure we generally advise patients not to fly for 2 − 3 weeks, to avoid hot drinks for 36 hours, and not to blow their nose for 2 weeks. Patients should not undertake strenuous exercise for at least ten days, and should try to sleep with their head elevated on an extra pillow if possible.
After surgery, to reduce the chance of a nose-bleed, hot drinks are avoided for 24 hours, and there should be no nose blowing or strenuous exercise for 2 weeks. If sneezing is unavoidable, pressure should not be allowed to build up in the nose. It is advisable to sleep on an extra pillow or two for the first few nights, and driving (including operating heavy machinery), alcohol, and sedative drugs should all be avoided for 24 hours.
If the eye pad has not been removed in the hospital then it should be removed in the morning at home. Normal washing is permissible, with care taken to avoid rubbing the eye. The wound should be kept dry and uncovered. Because surgery involves operating on some of the small sinus air spaces in the nose, swimming and flying in an aircraft should be avoided for least 2 to 3 weeks.
Discomfort after surgery is usually readily controlled with paracetamol or codeine (not Aspirin or Ibuprofen, which increases the risk of bruising and nose bleeds). In order to avoid medication containing Aspirin, the information leaflet accompanying any analgesia should be checked.
Sometimes the skin over the fine skin suture can become a little scabbed, and the inner corner of the eyelids occasionally feels itchy due to the very fine elastic ‘string’, or ‘stent’ which is placed in the operative site and which is removed after about 4 weeks. Frequently, due to the presence of this ‘stent’ the eyes can feel more watery in the first few weeks after surgery.
Many patients continue to have a watery eye for some weeks after surgery until the swelling and inflammation settles, and the silicone ‘string’ in the nose is removed. Although the skin incision heals over a few weeks, internal (unseen) swelling and healing may take many months to settle, and thus some occasional watering can persist for several months after surgery.
Sources :
https://www.hopkinsmedicine.org/health/conditions-and-diseases/dacryocystorhinostomy
https://www.esoprs.eu/for-patients/information/lacrimal-dacryocystorhinostomy-dcr-and-tubes/