Achilles Tendon Repair Surgery Techniques
Percutaneous Achilles tendon repair
Reconstruction with VY advancement
How long will it take to walk normally after Achilles tendon surgery?
Is Achilles tendon repair a major surgery?
Functional bracing/casting in resting equinus
Conservative treatment regimens vary greatly but commonly involve immobilisation with rigid casting or functional bracing. The foot is initially placed in full equinus (30° namely full plantarflexion). The foot is then brought into neutral sequentially over a period of 8-12 wk.
Read more about : Knee Ligament Repair
Read more about : Hip replacement
Read more about: Acl Repair Surgery Procedure
End-to-end Achilles tendon repair
We prospectively analyzed the functional and clinical results of patients who underwent a single end-to-end suture and an augmented tendon repair with plantaris tendon at middle-term follow-up. From January 2003 to May 2005, 30 consecutive patients were operated on for the treatment of acute Achilles' tendon rupture by means of 2 different methods. No cases required adjunctive procedures to allow for acceptable end-to-end apposition.
All ruptures were acute and repairable. The patients were divided into 2 groups. In group 1, augmentation with plantaris tendon was performed in addition to the Krakow end-to-end suturing technique in 16 patients, and in group 2, only the Krakow end-to-end suturing technique was used in 14 patients. The average age of the patients was 40.6 years.
Patients in the study groups were followed up at a mean of 17.8 months after surgery. At the end of the follow-up, functional and subjective outcome scores were evaluated. The American Orthopaedic Foot and Ankle Society hindfoot clinical outcome scores were 96.7 in group 1 and 98.8 in group 2. Although there was a numerical increase in group 2, no significant difference was determined between the 2 study groups statistically. The surgical outcome concerning local tenderness, skin adhesion scar, and tendon thickness was better in group 2 than in group 1 without a statistical significance.
Although functional outcomes of both treatment groups were the same, the end-to-end suturing technique provided a safer and more reliable treatment with a low risk of complications in the treatment of acute Achilles' tendon ruptures compared with the plantaris tendon augmentation technique.
Read more about: Acl Repair Surgery Time
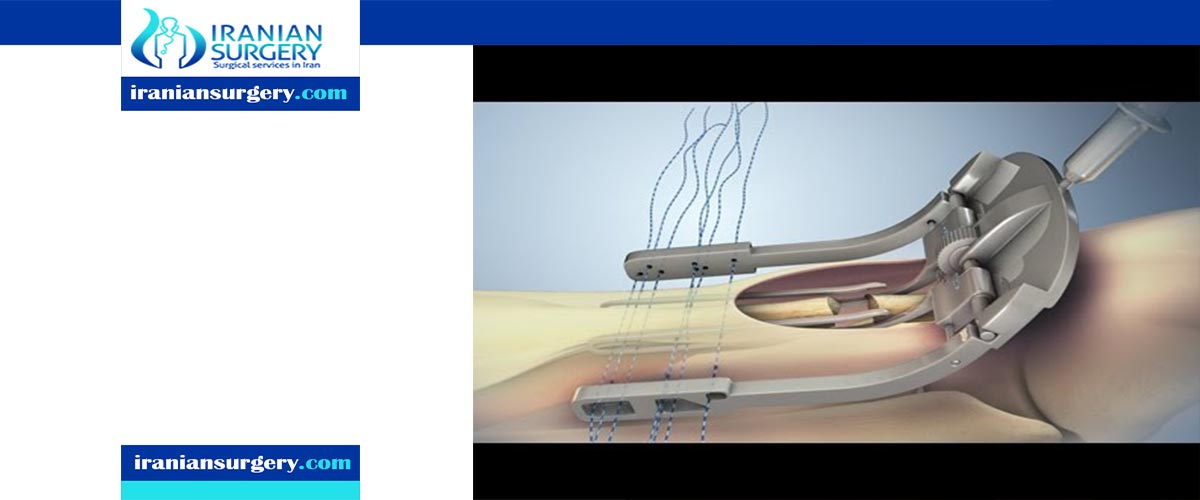
Percutaneous Achilles tendon repair
Klein recommends the use of absorbable sutures to reduce the symptoms should nerve injury occur. The Ma & Griffith repair consists of a Bunnel suture applied to the proximal tendon and a box suture distally in the stump inserted through 6 para-tendinous stab incisions.
Read more about: Repair of rotator cuff tendon
Reconstruction with VY advancement
A gap of 2 to 5 cm will usually require a V-Y slide lengthening. When the gap is more than 5 cm, V-Y advancement has been hypothesized to result in increased weakness of the muscle unit. Defects of more than 7 cm will require an Achilles turndown procedure or an allograft replacement.
The incidence of tendo-achilles rupture in the patients 30-40 years of age is increased specially in athletics to reach 75% of all cases. The tendon rupture is called neglected when the treatment is delayed more than four weeks from the date of injury. The percentage of misdiagnosis of Achilles tendon ruptures may reach 20%.
The delay in treatment of AT ruptures results in soft tissue retraction with degeneration of the tendon filling the gap between the ruptured ends with fibrotic scar tissue which leads to marked functional disability. In neglected or chronic ruptures of Achilles Tendon (AT), the retraction and atrophy of the tendon ends create a gap filled with scar tissue and fibrosis which make the reconstruction difficult. The extent of the gap and the potential recovery of the muscle are factors that affect the repair after reconstruction.
In the literature, the V-Y myotendinous advancement of the (AT) augmented by multiple transfers like gastrocnemius soleus complex Bosworth technique (a “turndown" of proximal tissue of the (AT)). In the study of Us et al. they reported 23% reduction in peak torque of the tendon after a V-Y lengthening technique for neglected A T ruptures.
Therefore, tendon transfer for augmentation of the V-Y advancement was recommended to augment the repair which requires lengthening to approximate the tendon ends for repair to add strength to the plantar flexion of the ankle joint. Many techniques for tendon transfers that augment the AT repair as peroneus brevis (PB) tendon, flexor digitorum longus (FDL) tendon, flexor hallucis longus (FHL) tendon . Different reports of these procedures have yielded satisfactory clinical results but the ankle flexion strength and beak torque deficits were persisted.
Read more about: How do you sleep after Achilles surgery?
How long will it take to walk normally after Achilles tendon surgery?
Achilles surgery takes only about 30 minutes to an hour, and you’ll go home the same day. The surgeons will put you in a cast that extends from below the knee to your toes. It’ll keep your foot in a pointed position.
Below is a timeline for what happens after that. Of course, this isn’t exactly what recovery will look like for everyone. Your progress will depend on your age, health, how bad your injury is -- and how well you stay with your rehab.
- Day of surgery: When you leave the hospital, you’ll get crutches and instructions not to put weight on the injured leg.
- In 2 weeks: Your doctor will take off your cast to remove the stitches and check how the wound is healing. Depending on how it looks, you could go back into the cast, but more likely you’ll get a walking boot. It’ll have a heel lift to keep your foot and ankle in the right position. You’ll also start rehab. The goal is to let the wound heal while you do some upper-body work. All your weight will still be on the crutches.
- By 4 weeks: The boot will be moved gradually to a neutral position (with heel lifts), and in rehab you’ll learn to walk on it correctly. Your physical therapist will move your ankle a bit and start to show you exercises that’ll help strengthen your calves. You’ll also do more work on your core and hips.
- Between 6 and 8 weeks: You’ll have fewer rehab appointments and should be able to stand on the injured leg for 10 seconds at a stretch. The boot could come off during this time, too. You can do more activities now, but still no high-impact exercise. Your therapist might recommend swimming or biking.
- At 4 to 6 months: You should be back to full activity, but you won’t be totally recovered until about a year after surgery. Even then, your strength might never get back to 100%.
Read more about: Achilles Tendon Repair Surgery Steps
Is Achilles tendon repair a major surgery?
tendon repair surgery can be done as a minimally invasive procedure. This is done with several small incisions instead of one large one. You will have some pain after your surgery, especially in the first few days. Achilles tendon surgery is often an outpatient procedure. This means you can go home the same day.
Read more about: Achilles Tendon Repair Surgery Complications
How successful is Achilles tendon surgery?
Both open and percutaneous surgeries are successful. More than 80 out of 100 people who have surgery for an Achilles tendon rupture are able to return to all the activities they did before the injury, including returning to sports.
Read more about: Achilles Tendon Repair Surgery Time
What are the types of Achilles tendon surgeries called?
There are two types of surgery to repair a ruptured Achilles tendon:
- In open surgery, the surgeon makes a single large incision in the back of the leg.
- In percutaneous surgery, the surgeon makes several small incisions rather than one large incision.
In both types of surgery, the surgeon sews the tendon back together through the incision(s). Surgery may be delayed for about a week after the rupture, to let the swelling go down.
Read more about: Achilles Tendon Repair Surgery
How long can you wait for Achilles tendon surgery?
Many surgeons advocate early operative repair of the ruptured Achilles tendon, citing decreased re-rupture rates and improved functional outcome. Waiting for surgical repair for longer than one month may lead to inferior functional results postoperatively.
Read more about: Achilles Tendon Repair Surgery

