Uterine Cancer
Uterine Cancer
What is Uterine Cancer?
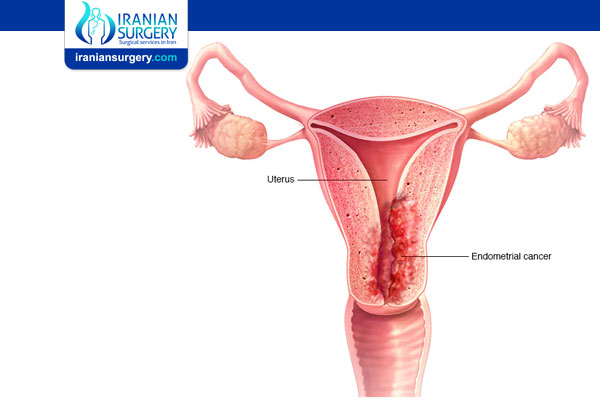
Uterine cancer is a general term that describes cancers of your uterus, or womb.
Uterine cancer includes two types of cancer: endometrial cancer (more common) and uterine sarcoma.
. Endometrial cancer develops in the endometrium, the inner lining of your uterus. It’s one of the most common gynecologic cancers — cancers affecting your reproductive system.
. Uterine sarcoma develops in the myometrium, the muscle wall of your uterus. Uterine sarcomas are very rare.
Before Uterine Cancer Treatment
Are endometrial cancer and uterine cancer the same?
Uterine cancer can refer to either endometrial cancer, uterine sarcoma or other rare forms of cancer that can arise in your uterus. But people often treat the terms “endometrial cancer” and “uterine cancer” the same. That’s because endometrial cancers are much more common than other cancers that can form in your uterus.
What does the uterus do?
The uterus is part of the reproductive system of people who are designated female at birth (DFAB), including cisgender women and nonbinary people with vaginas. It’s where a baby grows and develops during pregnancy.
The top part of your uterus is called the body or corpus. At the end of your uterus is your cervix, which connects your uterus to your vagina. Uterine cancer refers to cancer in the body of your uterus. Cancer in your cervix — cervical cancer — is a different type of cancer.
What does the endometrium do?
The endometrium is the inner layer of your uterus. It changes during your menstrual cycle.
A hormone called estrogen causes the endometrium to thicken in case of pregnancy. If no pregnancy occurs, your body produces less estrogen and more progesterone, a different hormone. When that happens, the endometrial lining sheds. That’s when periods take place.
Who’s at risk for uterine cancer?
There are several risk factors for endometrial cancer. Many of them relate to the balance between estrogen and progesterone. These risk factors include having obesity, a condition called polycystic ovarian syndrome (PCOS) or taking unopposed estrogen (taking estrogen without taking progesterone, too). A genetic disorder known as Lynch syndrome is another risk factor unrelated to hormones.
Risk factors include:
Age, lifestyle and family history:
. Age: As you get older, your likelihood of developing uterine cancer increases. Most uterine cancers occur after age 50.
. Diet high in animal fat: A high-fat diet can increase your risk of several cancers, including uterine cancer. Fatty foods are also high in calories, which can lead to obesity. Extra weight is a uterine cancer risk factor.
. Family history: Some parents pass on genetic mutations (changes) for hereditary nonpolyposis colorectal cancer (HNPCC). This inherited condition raises the risk for a range of cancers, including endometrial cancer.
Other conditions:
. Diabetes: This disease is often related to obesity, a risk factor for cancer. But some studies suggest a more direct tie between diabetes and uterine cancer as well.
. Obesity (having excess body weight): Some hormones get changed to estrogen by fat tissue, raising uterine cancer risk. The higher the amount of fat tissue, the greater the effect on estrogen levels.
. Ovarian diseases: People who have certain ovarian tumors have high estrogen levels and low progesterone levels. These hormone changes can increase uterine cancer risk.
Menstrual and reproductive history:
. Early menstruation: If your period started before age 12, your risk for uterine cancer might increase. That’s because your uterus gets exposed to estrogen for more years.
. Late menopause: Similarly, if menopause occurs after age 50, the risk also increases. Your uterus gets exposed to estrogen longer.
. Long menstruation span: The number of years menstruating might be more important than your age when periods started or ended.
. Not getting pregnant: People who haven’t been pregnant have a higher risk because of the increased exposure to estrogen.
Previous treatments for other conditions:
. Earlier radiation therapy to the pelvis (between belly and legs): Radiation therapy to treat other cancers can damage cell DNA. This damage may increase your risk of developing a second type of cancer.
. Estrogen replacement therapy (ERT): Some people receive estrogen therapy to help relieve menopause symptoms. Getting ERT without progesterone places you at a higher risk for uterine cancer.
. Use of tamoxifen: People may receive this drug for breast cancer treatment. It acts like estrogen in the uterus and can increase the risk of uterine cancer.
How common is uterine cancer?
In the United States, endometrial cancer is the most common cancer affecting a DFAB person’s reproductive system. Endometrial cancer mainly develops after menopause. About 3% of cisgender women receive a diagnosis of uterine cancer at some point during their lives.
What causes uterine cancer?
Researchers aren’t sure of the exact cause of uterine cancer. Something happens to create changes in cells in your uterus. The mutated cells grow and multiply out of control, which can form a mass called a tumor.
Certain risk factors can increase the chances you’ll develop uterine cancer. If you’re at high risk, talk to your healthcare provider about steps you can take to protect your health.
What are the symptoms of uterine cancer?
Signs of uterine cancer can resemble those of many conditions. That’s especially true of other conditions affecting reproductive organs. If you notice unusual pain, leaking or bleeding, talk to your healthcare provider. An accurate diagnosis is important so you can get the proper treatment.
Symptoms of endometrial cancer or uterine sarcoma include:
. Vaginal bleeding between periods before menopause.
. Vaginal bleeding or spotting postmenopause, even a slight amount.
. Lower abdominal pain or cramping in your pelvis, just below your belly.
. Thin white or clear vaginal discharge if you’re postmenopausal.
. Extremely prolonged, heavy or frequent vaginal bleeding if you’re older than 40.
Uterine Cancer Surgery Side Effects
Side effects of uterine cancer surgery include:
. Infertility, not being able to get pregnant.
. Menopause (if you were premenopausal) and its symptoms, including vaginal dryness and night sweats.
Diagnosis and Tests
How is uterine cancer diagnosed?
Talk to your healthcare provider if you notice possible signs of uterine cancer. Your provider will:
. Ask about your symptoms, risk factors and family history.
. Perform a physical exam.
. Perform a pelvic exam.
What tests will I need to diagnose uterine cancer?
Your provider may perform one or more tests to confirm a diagnosis of uterine cancer:
Lab tests:
. CA-125 assay is a blood draw that measures CA-125, a protein. A certain amount of CA-125 can point to cancer in your body.
Imaging tests:
. CT scans take a series of detailed pictures of the inside of your body.
. MRI scans use radio waves and a powerful magnet to create images.
. Transvaginal ultrasound inserts a special probe (smooth, rounded device) into your vagina to get pictures of your uterus.
Other tests:
. Endometrial biopsy inserts a thin, flexible tube through your cervix (opening of your uterus) and into your uterus. Your provider removes a small amount of the endometrium.
. Hysteroscopy inserts a hysteroscope, a long thin tube, through your vagina and cervix to reach your uterus. This narrow instrument with a light and camera provides detailed images of your uterus.
. Dilation and curettage (D&C) is a more complex procedure to remove uterine tissue. It takes place in the operating room.
If you had a D&C or biopsy to remove tissue samples, your provider then sends the sample to a lab. There, a pathologist looks at the tissue to confirm if there’s cancer.
Can a Pap test diagnose uterine cancer?
No. The Pap test (Pap smear) doesn’t screen for or diagnose uterine cancer. It checks for cervical cancer.
What else does an endometrial cancer diagnosis show?
If your healthcare provider diagnoses endometrial cancer, they also need to determine the type. Knowing the cancer type helps your care team figure out the best treatment:
. Type 1 endometrial cancers are less aggressive. They usually don’t spread to other tissues quickly.
. Type 2 endometrial cancers are more aggressive. They’re more likely to spread outside of the uterus and need stronger treatment.
Your provider will also determine the stage (severity) of your cancer. Uterine cancers are staged on a scale that ranges from I to IV.
. Stage I cancer hasn’t spread beyond your uterus.
. Stage II cancer has spread to your cervix.
. Stage III cancer has spread to your vagina, ovaries and/or lymph nodes.
. Stage IV cancer has spread to your bladder or other organs far away from your uterus.
In some cases, your provider may not be able to determine what stage of cancer you have until you’ve had surgery to remove it.
Prevention
Can uterine cancer be prevented?
Most of the time, you can’t prevent uterine cancer. But you can take steps to reduce your risk:
. Control diabetes.
. Maintain a healthy weight.
. Talk to your provider about using oral contraceptives. These medications can offer some protection against uterine cancer.
Will estrogen replacement therapy (ERT) make me more likely to get uterine cancer?
If you are considering ERT, talk to your healthcare provider. Together, you can discuss your cancer risk and make the decision that’s best for you.
Is there a screening test for uterine cancer?
No, there’s no screening tool. And healthcare providers usually don’t recommend regular testing for people without symptoms. They may do so if you’re at higher risk, though. If you’re at high risk, talk to your provider about regular checks for uterine cancer.
During Uterine Cancer Treatment
Management and Treatment
How is uterine cancer treated?
Most people with endometrial cancer need surgery. Your particular treatment plan depends on the type of cancer and your overall health. Other treatments you may have include:
. Chemotherapy, which uses powerful drugs to destroy cancer cells.
. Radiation therapy, which sends targeted radiation beams to destroy cancer cells.
. Hormone therapy, which gives hormones or blocks them to treat cancer.
. Immunotherapy, which helps your immune system fight cancer.
. Targeted therapy, which uses medications to target specific cancer cells to stop them from multiplying.
Researchers continue to study more ways to treat endometrial cancer.
What type of uterine cancer surgery will I need?
Surgery is usually the primary treatment for endometrial cancer. You’ll most likely have a hysterectomy, with the surgeon removing your uterus and cervix. There are three types of hysterectomy procedures:
. Total abdominal hysterectomy: The surgeon makes an incision (cut) in your abdomen to access and remove your uterus.
. Vaginal hysterectomy: The surgeon removes your uterus through your vagina.
. Radical hysterectomy: If cancer has spread to your cervix, you may need a radical hysterectomy. The surgeon removes your uterus and the tissues next to your uterus. The surgeon also removes the top part of your vagina, next to your cervix.
. Minimally invasive hysterectomy: The surgeon makes multiple small incisions (cuts) to remove your uterus. This may be done robotically.
During a hysterectomy, surgeons often perform two other procedures as well:
. Bilateral salpingo-oophorectomy (BSO) to remove your ovaries and fallopian tubes. Most people need this extra step to make sure all cancer gets removed.
. Lymph node dissection to remove lymph nodes and see if cancer has spread.
Do I need to have my ovaries removed?
Many people who have uterine cancer need their ovaries removed. But removing the ovaries means you will go through menopause if you haven’t already. If you’re younger than 45 and premenopausal, talk to your care team to see if you should keep your ovaries.
How is a uterine sarcoma treated?
Often, surgeons use a single procedure to diagnose, stage (describe severity) and treat uterine sarcoma. Treatment options are like those for endometrial cancer. You may have a hysterectomy, as well as a BSO to remove your ovaries and fallopian tubes.
After Uterine Cancer Treatment
Outlook / Prognosis
What’s the survival rate for people with uterine cancer?
The five-year survival rate for endometrial cancer is 81%. That means 81% of people diagnosed with the disease are alive five years later. The rate is even higher when cancer is localized and hasn’t spread outside the uterus. Then the survival rate reaches as high as 95%. Treatments continue to improve, along with survival rates.
How fatal is uterine cancer?
Uterine cancer is fatal when it goes undiagnosed and spreads. The survival rate for cancer that hasn’t spread outside the uterus is 95%. The survival rate decreases to 17% when cancer spreads to other parts of your body outside your uterus. Early detection and early treatment are key to a favorable prognosis.
Can uterine cancer be cured?
Fortunately, endometrial cancer is often diagnosed at an early stage. That’s because many people notice unusual bleeding and tell their healthcare providers. If cancer gets caught early and hasn’t spread to other organs, removing your uterus can cure it.
When should I see my healthcare provider?
Discuss any unusual bleeding or spotting with a provider. If you’ve inherited endometrial cancer risk, talk to your provider about yearly testing. You may need an endometrial biopsy every year, starting at age 35.
How can I take care of myself after uterine cancer treatment?
After you finish treatment, your care team will talk to you about your follow-up visits. It’s important to go to these appointments. During a follow-up visit, your provider will do a pelvic exam. They’ll also ask you about any symptoms. The goal is to make sure cancer isn’t coming back and that you’re feeling OK after treatment.
You can also talk to your provider about ways to live a healthier life after cancer. Eating well, getting enough sleep and exercising can help you feel your best.
Source:
. https://my.clevelandclinic.org/health/diseases/16409-uterine-cancer