What is Stage 4 Prostate Cancer?
Stage 4 prostate cancer is a cancer that begins in the prostate and spreads to nearby lymph nodes or to other areas of the body.
Stage 4 prostate cancer is an uncommon diagnosis. Most often, prostate cancer is diagnosed at an earlier stage, when the cancer is confined to the prostate.
Treatments may slow or shrink an advanced prostate cancer, but for most men, stage 4 prostate cancer isn't curable. Still, treatments can extend your life and reduce the signs and symptoms of cancer.
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Surgeons to treat your Prostate Cancer in Iran. The price of treating a Prostate Cancer in Iran can vary according to each individual’s case and will be determined by the type of treatment you have and an in-person assessment with the doctor.
For more information about the cost of Prostate Cancer Treatment in Iran and to schedule an appointment in advance, you can contact Iranian Surgery consultants via WhatsApp number 0098 901 929 0946. This service is completely free.
Before Prostate Cancer Stage 4
Symptoms
Signs and symptoms of stage 4 prostate cancer may include:
. Painful urination
. Decreased force in the stream of urine
. Blood in the semen
. Bone pain
. Swelling in the legs
. Fatigue
When to see a doctor
Make an appointment with your doctor if you have any persistent signs or symptoms that worry you.
Causes
Doctors aren't certain what causes stage 4 prostate cancer.
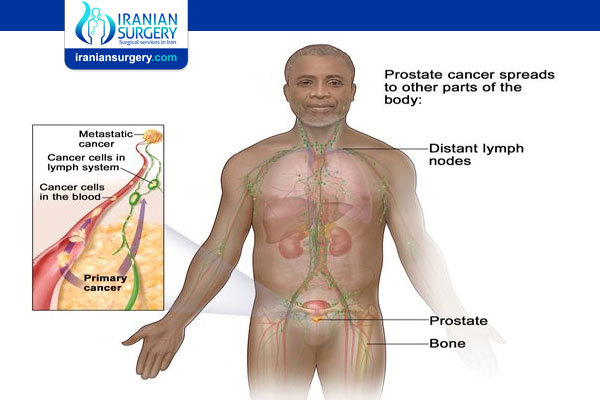
Stage 4 prostate cancer occurs when prostate cancer cells break away from the prostate and spread to the lymph nodes or to other areas of the body.
Prostate cancer cells that spread beyond the prostate most often travel to the:
. Lymph nodes
. Bones
. Liver
Read more about: prostate cancer treatments pros and cons
Risk factors
Factors that may increase your risk of stage 4 prostate cancer include:
. A family history of prostate cancer. Men with certain inherited gene mutations that increase the risk of prostate cancer have an increased risk of more-aggressive prostate cancers.
. African-American race. Black men have an increased risk of aggressive prostate cancer.
Diagnosis
If your doctor suspects you may have prostate cancer, tests and procedures may include:
. Imaging tests. Imaging tests may help your doctor understand the size and extent of your prostate cancer. Tests may include ultrasound, MRI, CT, positron emission tomography (PET) and bone scans.
Which tests you undergo depends on your situation, such as whether you're experiencing signs and symptoms.
. Biopsy. To confirm the diagnosis of prostate cancer, your doctor may recommend a biopsy procedure to remove a sample of suspicious cells for laboratory testing. In a lab, doctors can examine the cells and determine if they're cancerous.
During Prostate Cancer Stage 4
Treatment
Treatments for stage 4 prostate cancer may slow the cancer and extend your life. But stage 4 prostate cancer often can't be cured.
Hormone therapy
Hormone therapy is treatment to stop your body from producing the male hormone testosterone or to block the effects of testosterone on the cancer. Prostate cancer cells rely on testosterone to help them grow. Cutting off the supply of hormones may cause the cancer to shrink or to slow its growth.
In men with stage 4 prostate cancer, hormone therapy is most often used alone, but it can be combined with chemotherapy and it may be used after radiation therapy or, rarely, surgery. Hormone therapy may be continued for as long as the treatment continues to work.
Hormone therapy options include:
. Medications that stop your body from producing testosterone. Medications known as luteinizing hormone-releasing hormone (LH-RH) agonists and antagonists prevent the testicles from receiving messages to make testosterone. Drugs typically used in this type of hormone therapy include leuprolide (Eligard, Lupron Depot, others), goserelin (Zoladex), triptorelin (Trelstar), histrelin (Vantas) and degarelix (Firmagon).
. Surgery to remove the testicles (orchiectomy). Removing your testicles reduces testosterone levels in your body. The effectiveness of orchiectomy in lowering testosterone levels is similar to that of hormone therapy medications, but orchiectomy may lower testosterone levels more quickly.
. Medications that block testosterone from reaching cancer cells. Medications known as anti-androgens prevent testosterone from reaching your cancer cells. Examples include bicalutamide (Casodex), flutamide and nilutamide (Nilandron). These drugs may be given along with an LH-RH agonist or given before taking an LH-RH agonist.
Apalutamide (Erleada) and enzalutamide (Xtandi) work differently from other anti-androgen drugs and may be an option if other hormone therapy treatments are no longer effective.
. Other medications. Other medications that work differently from other hormone therapies to control testosterone in the body may be options. Examples include abiraterone (Yonsa, Zytiga), the antifungal medication ketoconazole, the female hormone estrogen, and steroid drugs.
Side effects of hormone therapy may include erectile dysfunction, hot flashes, loss of bone mass, reduced sex drive, breast enlargement and weight gain.
Most advanced prostate cancers will eventually adapt to hormone therapy and begin growing despite treatment (castration-resistant prostate cancer). When that occurs, your doctor may recommend switching to a different combination of hormone therapy drugs to see if your cancer responds.
Radiation therapy
Radiation therapy uses high-powered beams of energy, such as X-rays and protons, to kill cancer cells. Radiation therapy for stage 4 prostate cancer uses a large machine that moves around your body, directing energy beams to the area around the cancer (external beam radiation therapy).
In men with very large prostate tumors or cancer that has spread to nearby lymph nodes (locally advanced prostate cancer), radiation therapy may be combined with hormone therapy. Or it may be used after surgery to kill any cancer cells that might remain.
In men with cancer that has spread to other areas of the body, radiation therapy is used to relieve pain or other symptoms.
Surgery
Surgery isn't often used to treat stage 4 prostate cancer, but it might be recommended in certain situations. In men with stage 4 prostate cancer, surgery is generally limited to men who are experiencing signs and symptoms that would be relieved by surgery, such as difficulty passing urine.
Surgery may include:
. Radical prostatectomy. Your doctor may recommend surgery to remove your prostate and any cancer that has grown locally beyond the prostate. Surgery may be an option if your prostate cancer is locally advanced and hasn't spread to other areas of the body.
. Lymph node removal. Your doctor may recommend removal of several lymph nodes near your prostate (pelvic lymph node dissection) to test for cancer cells.
Surgery can cause infection, bleeding, incontinence, erectile dysfunction and damage to the rectum.
Treatments for cancer that spreads to other areas of the body
If your cancer has spread beyond your prostate to other areas of your body, your doctor may recommend:
. Chemotherapy. Chemotherapy can slow the growth of cancer cells, relieve signs and symptoms of cancer, and prolong the lives of men with advanced prostate cancer.
. Training your immune system to recognize cancer cells. Immunotherapy uses your immune system to kill cancer cells. Sipuleucel-T (Provenge), a form of immunotherapy, has been developed to genetically engineer your immune cells to fight prostate cancer.
. Bone-building medications. Medications used to treat thinning bones (osteoporosis) may be helpful in preventing broken bones in men with prostate cancer that has spread to the bones.
. Infusions of a radioactive drug. Men with prostate cancer that has spread to the bones may consider treatment that infuses a radioactive substance into a vein. Strontium-89 (Metastron), samarium-153 (Quadramet) and radium-223 (Xofigo) are medications that target fast-growing cancer cells in the bones, and may help relieve bone pain.
. Radiation therapy. External beam radiation therapy may help control bone pain in men with prostate cancer that has spread to the bones.
. Targeted drug therapy. Targeted drugs attack specific weaknesses in the cancer cells. Your doctor might have samples of your cancer tested in a lab to see if targeted therapy might be helpful for you.
. Pain medications and treatments. Medications and treatments are available if you experience cancer pain. Which pain treatments are right for you will depend on your particular situation and your preferences.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
Alternative medicine
No alternative medicine treatments have been proved to cure stage 4 prostate cancer. But complementary and alternative medicine may help you cope with symptoms of your cancer.
Prostate cancer often spreads to the bones, which can cause bone pain. Your doctor can offer treatments and medications to control the pain. But you may also find that complementary therapies can help relieve your pain when used in addition to treatments recommended by your doctor.
Complementary and alternative medicine treatments that may reduce cancer pain include:
. Acupuncture
. Acupressure
. Hypnosis
. Massage
. Relaxation techniques
If your pain isn't adequately controlled, talk with your doctor about your options.
After Prostate Cancer Stage 4
After surgery
After your operation you will wake up on the recovery room. Once it’s safe to do so, you usually go back to the ward. Recovery rooms and wards are busy and often noisy places that some people find strange and disorienting. You'll feel drowsy because of the anaesthetic and painkillers.
. Tubes and drains
When you wake up, you may have several tubes in you. This can be frightening, so it helps to know what they’re for.
You may have:
. A drip to give you fluids usually through a vein in your arm
. A small wound drain to drain any blood or fluid if you’ve had a radical prostatectomy
. A tube into your bladder (catheter) to measure how much urine you pass.
The catheter stays in for a couple of weeks if you’ve had a radical prostatectomy. After removal of the inner part of the prostate gland (TURP) it stays in for a couple of days. Sometimes you need the catheter to stay in place for a while after you go home. Before you leave hospital your nurse will show you how to look after it.
You may also have an oxygen mask on.
. Painkillers
It’s normal to have pain for the first week or so. You have painkillers to help.
Tell your doctor or nurse as soon as you feel any pain. They need your help to find the right type and dose of painkiller for you. Painkillers work best when you take them regularly.
Immediately after surgery you might have painkillers through a drip into the bloodstream that you control. This is called patient controlled analgesia (PCA).
Or you might have painkillers through a small thin tube that is put into your back. This tube is connected to a pump that gives you a constant dose of painkiller. This is called an epidural.
You get painkillers to take home. Follow the instructions your nurse gives you about how often and when to take them. Contact your doctor if you still have pain or if it gets worse.
After keyhole surgery you will only need painkillers to take by mouth.
. Eating and drinking
Your team will let you know when you can start eating and drinking again.
. Your wound
After a radical prostatectomy, you have dressings over your wounds. You have 1 wound if you had open surgery. You may have several smaller wounds if you had keyhole (laparoscopic) surgery. After a couple of days your nurse changes the dressings and cleans your wounds.
Your stitches or clips stay in for at least 10 days. The nurse usually takes them out before you go home. You can go home with the stitches in if your wound is still healing and you are otherwise well. The practice nurse, district nurse or hospital nurse then takes them out. This might be at home, at your GPs, or you may need to go back to the hospital.
Before you go home the nurse gives you information about how to care for the wound.
Getting up
Your nurses and physiotherapists help you to move around as soon as possible. They check you’re doing your breathing and leg exercises. This helps you recover.
You might be sitting in a chair within 12 hours of your operation. The day after, you’ll be walking around your bed. And within a few days you’ll be able to walk along the hospital corridor.
Making progress
During the first few days after your operation, you’ll start to feel better. The drips and drains will come out, you’ll start eating and can move about better.
. You’ll begin to feel like you’re making progress.
. Most people go home about 3 to 7 days after an open radical prostatectomy.
. After robotic surgery you will go home within 24 to 48 hours.
Going home
You’ll need help when you first go home. The dietitian will talk to you and your family about what to eat. It can take some time to find what works for you.
You’re likely to feel very tired for several weeks and sometimes months after your surgery. It helps to do a bit more every day.
Try:
. Sitting for less time each day
. Walking around the house a bit more each day
. Building up to walking outside
What you can do depends on how fit you were before your surgery and any problems you have afterwards. Talk to the physiotherapist or your doctor if you’re unsure about what you should be doing.
Contact your doctor or specialist nurse if you have any problems or symptoms you’re unsure about. You’ll have follow up appointments to check your recovery and fix any problems. They’re also your opportunity to raise any concerns you have.
Follow up
You’ll have follow up appointments to check your recovery and sort out any problems. They’re also your opportunity to raise any concerns you have about your progress.
Your first checkup is around 6 weeks after your operation. Then you have one every 6 months for 2 years. Then once a year after that.

