Pancreatic Surgery
What to Expect After an Operation?
How serious is pancreatic surgery?
How long does it take to recover from a pancreas surgery?
Why would you need pancreas surgery?
How long can you live without a pancreas?
What is the average hospital stay for pancreatitis?
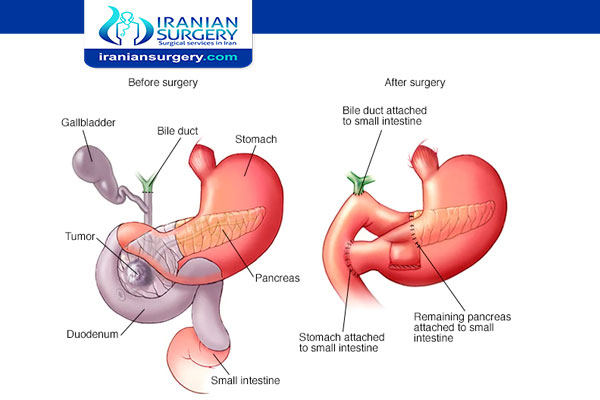
Whipple procedure
A Whipple procedure also known as a pancreaticoduodenectomy is a complex operation to remove the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder and the bile duct.
The Whipple procedure is used to treat tumors and other disorders of the pancreas, intestine and bile duct. It is the most often used surgery to treat pancreatic cancer that's confined to the head of the pancreas. After performing the Whipple procedure, your surgeon reconnects the remaining organs to allow you to digest food normally after surgery.
The Whipple procedure is a difficult and demanding operation and can have serious risks. However, this surgery is often lifesaving, particularly for people with cancer.
Read more about : Kidney transplant in Iran success story in Iran
Read more about : Cancer treatment success story in Iran
Related procedures
Depending on your situation, your doctor may talk with you about other pancreatic operations. Seek a second opinion from a specialized surgeon if needed.
Options include:
Surgery for tumors or disorders in the body and tail of the pancreas. Surgery to remove the left side (body and tail) of the pancreas is called a distal pancreatectomy. With this procedure, your surgeon may also need to remove your spleen.
Surgery to remove the entire pancreas. This is called total pancreatectomy. You can live relatively normally without a pancreas but will need lifelong insulin and enzyme replacement.
Surgery for tumors affecting nearby blood vessels. Many people are not considered eligible for the Whipple procedure or other pancreatic surgeries if their tumors involve nearby blood vessels.
Who Is a Candidate for the Whipple Procedure?
Only about 20% of pancreatic cancer patients are eligible for the Whipple procedure and other surgeries. These are usually patients whose tumors are confined to the head of the pancreas and haven't spread into any nearby major blood vessels, the liver, lungs, or abdominal cavity. Intensive testing is usually necessary to identify possible candidates for the Whipple procedure.
Some patients may be eligible for a minimally invasive (laparoscopic) Whipple procedure, which is performed through several small incisions instead of a single large incision. Compared to the classic procedure, the laparoscopic procedure may result in less blood loss, a shorter hospital stay, a quicker recovery, and fewer complications.
Types of Pancreatic Surgery
Pancreatic surgical procedures include:
- Minimally invasive pancreatic resections
- Spleen-preserving pancreatectomy
- Enucleation of pancreatic tumors
Read more about: Pancreatic islets
Read more about: Is Pancreatic cancer aggressive?
Why it's done?
A Whipple procedure may be a treatment option for people whose pancreas, duodenum or bile duct is affected by cancer or other disorder. The pancreas is a vital organ that lies in the upper abdomen, behind your stomach. It works closely with the liver and ducts that carry bile. The pancreas releases (secretes) enzymes that help you digest food, especially fats and protein. The pancreas also secretes hormones that help manage your blood sugar.
Open surgery
During an open procedure, your surgeon makes an incision in your abdomen in order to access your pancreas. This is the most common approach and the most studied.
Laparoscopic surgery
During laparoscopic surgery, the surgeon makes several smaller incisions in your abdomen and inserts special instruments, including a camera that transmits video to a monitor in the operating room. The surgeon watches the monitor to guide the surgical tools in performing the Whipple procedure. Laparoscopic surgery is a type of minimally invasive surgery.
Robotic surgery
Robotic surgery is a type of minimally invasive surgery in which the surgical tools are attached to a mechanical device (robot). The surgeon sits at a console nearby and uses hand controls to direct the robot. A surgical robot can use tools in tight spaces and around corners, where human hands may be too large to be effective.
During the procedure
A surgical team works together to enable you to have a safe and effective surgery. The team is made up of pancreatic surgeons, specialized surgical nurses, anesthesiologists and anesthetists doctors and nurses trained in giving medication that causes you to sleep during surgery and others.
After you are asleep, additional intravenous lines may be placed with other monitoring devices, depending on the complexity of the operation and your overall health conditions. Another tube, called a urinary catheter, will be inserted into your bladder. This drains urine during and after surgery. It is typically removed one or two days after surgery.
Surgery may take four to 12 hours, depending on which approach is used and the complexity of the operation. Whipple surgery is done using general anesthesia, so you'll be asleep and unaware during the operation.
Read more about: Is Pancreatic cancer aggressive?
Read more about: pancreas cancer treatment in iran
What to Expect After an Operation?
As with all major operations, recovering from pancreatic surgery takes time. Full recovery requires an average of two months. Your recovery can be divided into different stages, each of which carry a different set of expectations. However, it is important to remember that every patient's recovery is different, even patients undergoing the exact same procedure.
Hospital Recovery
Patients spend an average of 3-10 days in the hospital after pancreas surgery. While you are in the hospital, many members of your health care team will be checking in on you daily. Your in-house team consists of residents, medical students, nurses, and your surgeon. Your team will closely monitor your progress throughout your stay. You will be seen by residents and nurses several times each day and by your surgeon and/or one of our Pancreas Center surgeons at least once each day.
It is normal to experience pain after pancreas surgery. While in the hospital, you will be able to manage your pain with intravenous pain medication. Once you are at home, you will manage your pain with oral medications prescribed by your health care team.
After your operation, you will have staples and special dressings where incisions were made during your procedure. You may also have some surgical drainage tubes left in your abdomen. Your team will check your dressings regularly to ensure they are healing well and monitor any tubes to ensure proper drainage. It is normal to be discharged home with the surgical drainage tubes still in place, so do not be worried about your recovery if this happens to you. You will be given specific instructions on how to care for both the drainage tubes and your surgical dressing before you are discharged from the hospital; both will be removed during one of your postoperative visits to the Pancreas Center.
Due to a condition known as "gastric ileus," or temporary paralysis of the stomach, you will not be able to eat for many days after your surgery. While you are in the hospital, your health care team will ensure you receive proper hydration intravenously. There is no way to predict how quickly your stomach will regain its full function after an operation, and patients must undergo a trial-and-error process as they attempt to resume normal eating. While this process can be frustrating, it is also perfectly normal. You will not be discharged from the hospital until you can tolerate food and liquid, however it still may take several weeks before your digestive system returns to "normal."
Read more about: pancreatic cancer stages timeline
Read more about: Cervical cancer causes
Food and medications
Talk to your doctor about:
- When you can take your regular medications and whether you can take them either the night before or the morning of surgery
- When you need to stop eating or drinking the night before the surgery
- Allergies or reactions you have had to medications
- Any history of difficulty or severe nausea with anesthesia
What Are Complications of the Whipple Procedure?
Immediately after the Whipple procedure, serious complications can affect many patients. One of the most common of these include the development of false channels (fistulas) and leakage from the site of the bowel reconnection. Other possible surgical complications include:
- Infections
- Bleeding
- Trouble with the stomach emptying itself after meals
Other possible complications include:
- Weight loss. Most patients can expect to lose weight after the surgery.
- Diabetes. This condition can develop if too many insulin-producing cells are removed from the pancreas. However, patients who have normal blood sugar before surgery are unlikely to develop diabetes, and those who recently developed diabetes before surgery are even likely to improve.
Below are five more key facts about pancreatic cancer surgery.
- About 20 percent of pancreatic cancer patients are eligible for surgery at diagnosis. Since pancreatic cancer symptoms are often vague and the pancreas is located deep within the body, the disease is often diagnosed in its later stages.
In addition, a significant number of patients who are eligible for surgery are told they are ineligible.
There are different types of surgeries that a pancreatic cancer patient can undergo. The most common surgery is known as the Whipple procedure (pancreaticoduodenectomy). The Whipple is performed on patients whose tumor is confined to the head of their pancreas.
Pancreatic cancer patients may also undergo a distal pancreatectomy or complete pancreatectomy, which involve removing some or all of their pancreas. The appropriate surgery is selected based on the size and location of the tumor within the patient’s pancreas and other eligibility criteria.
- Surgery may be offered alongside other treatments. Pancreatic cancer patients may receive chemotherapy and/or radiation or other treatment types before surgery, known as neoadjuvant therapy, or after surgery, known as adjuvant therapy.
- The tissue removed during surgery can help inform future treatment decisions
. There are some tumor characteristics, known as “actionable alterations,” that can predict a patient’s response to certain types of treatments.
- Surgery can be supportive (palliative), too. Palliative procedures are performed to alleviate (palliate) symptoms. They do not involve the complete removal of the tumor. Palliative procedures may relieve symptoms of jaundice, pain or nausea and vomiting that are caused by blockage of the bile duct and/or duodenum.
The most common palliative procedures for pancreatic cancer are biliary bypass surgery, gastric bypass surgery and biliary or duodenal stent insertion.
How serious is pancreatic surgery?
The Whipple procedure is a difficult and demanding operation and can have serious risks. Up to half of patients develop serious complications and 2 to 4 percent do not survive the procedure one of the highest mortality rates for any operation. One common complication is leakage of fluid from the pancreas after the surgery, often in large amounts that can cause an abscess and lead to infection and sepsis.
Read more about: Pancreas transplantation
Read more about: Surgical oncology
How long does it take to recover from a pancreas surgery?
As with all major operations, recovering from pancreatic surgery takes time. Full recovery requires an average of two months.
Although patients can leave the hospital after a few days or weeks, a full recovery from pancreas surgery can take two months or longer. During the first two months, the patient requires frequent hospital visits to review pathology and surgical reports. Incisions will be examined and staples and tubes will be removed. The doctor will also talk to the patient about diet, bowel functions, and pain control to ensure recovery.
If a patient is having issues with diet, they may be referred to a clinical nutritionist to help with individual needs. After the first two months of very regular postoperative evaluations, the frequency of follow-up evaluations will be reduced to every three to six months. Depending on the type of resection and the resulting pathology, the patient may undergo regular imaging studies such as magnetic resonance imaging or computed tomography to check for recurrence of cancer.
Patients may also need to undergo regular blood tests to ensure important indicators like tumor markers and liver function tests remain within normal ranges. Most patients who undergo surgery for pancreatic cancer will also require a course of chemotherapy after their operation. Chemotherapy does not normally start until six to eight weeks after surgery.
Read more about: Pancreatic islets
Read more about: Pancreatic Surgery
Why would you need pancreas surgery?
Only about 20% of pancreatic cancer patients are eligible for the Whipple procedure and other surgeries. These are usually patients whose tumors are confined to the head of the pancreas and haven't spread into any nearby major blood vessels, the liver, lungs, or abdominal cavity.
How long can you live without a pancreas?
It's possible to live without a pancreas. But when the entire pancreas is removed, people are left without the cells that make insulin and other hormones that help maintain safe blood sugar levels. These people develop diabetes, which can be hard to manage because they are totally dependent on insulin shots. Without artificial insulin injections and digestive enzymes, a person without a pancreas cannot survive. One 2016 study found that about three-quarters of people without cancer survived at least 7 years following pancreas removal.
What is the average hospital stay for pancreatitis?
The length of your hospital stay depends on the severity of the condition. Some people may stay for just a few days, while others may stay for as long as several months if continued monitoring is necessary or surgery is required.
Read more about: Pancreatectomy in Iran

