Pancreatic Cancer Stage 4
Pancreatic Cancer Stage 4
What is Stage 4 Pancreatic Cancer?
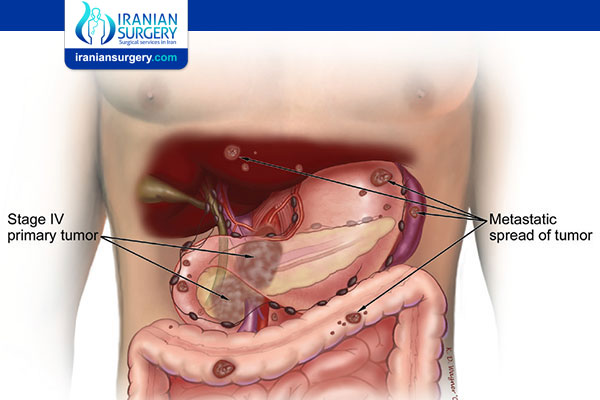
In stage 4 pancreatic cancer, abnormal cells that grew into a tumor in the pancreas have spread through the bloodstream to form tumors in distant parts of the body, such as the bones or lungs. It is also called metastatic pancreatic cancer.
Stage 4 pancreatic cancer is not curable, but palliative care and treatments can help improve quality of life and survival time.
This article looks at the two types of pancreatic cancer, its stages, and its symptoms. It also explains how healthcare providers identify and treat stage 4 pancreatic cancer and offers some ideas for coping with what this diagnosis means.
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Surgeons to treat your Pancreatic Cancer in Iran. The price of treating a Pancreatic Cancer in Iran can vary according to each individual’s case and will be determined by the type of treatment you have and an in-person assessment with the doctor.
For more information about the cost of Pancreatic Cancer Treatment in Iran and to schedule an appointment in advance, you can contact Iranian Surgery consultants via WhatsApp number 0098 901 929 0946. This service is completely free.
What Stage 4 Pancreatic Cancer Means?
Healthcare providers use cancer stages to describe how cancer has grown or spread. Stage 4 is the most advanced and, by definition, it means that cancer has spread throughout the body (metastasized).
One system for staging cancers, called the TNM system, has three components:
. T (tumor): Based on the tumor’s size and spread, the T rating ranges from T0 to T4. In stage 4 pancreatic cancer, the primary tumor can have any T rating.
. N (lymph nodes): Stage 4 pancreatic cancer can have an N rating of either N1 (cancer has spread to one to three regional lymph node) or N2 (cancer is in four or more regional lymph nodes). Lymph nodes are structures throughout the body that help filter foreign substances. Their involvement makes it easier for cancer to spread to other locations.
. M (metastasis): Metastasis is the spread of cancer to distant organs and lymph nodes. There are only two M stages—M0 or M1. Any pancreatic cancer with an M1 rating is considered stager 4.
Pancreatic cancer most frequently spreads within the peritoneal cavity, which encloses the organs in the abdomen. It can also spread to the liver, lungs, brain, and bones.
While some healthcare providers use the TNM staging system, others use four categories that describe the extent of a cancer's spread. Stage 4 would be classified as "metastatic.
Your Stage vs. Your Actual Diagnosis
Practically speaking, if you have a stage 2 pancreatic tumor that spreads throughout your body, you now have a stage 4 tumor. However, that's not exactly what your lab report will say.
On paper, the stage of your cancer will always be what it was when you were diagnosed—even if it advances and spreads. This is so that doctors can understand your disease's progression. If cancer is re-staged, the new stage will be added to the original one (with an "r" designation).
For example, a stage 2 pancreatic tumor may be diagnosed based on a T1, N1, M0 rating. If that tumor metastasizes (meaning it's now stage 4) but otherwise doesn't change, it would have a T1, N1, rM1 rating. This tells the doctor that your stage 2 tumor has now spread to distant parts of your body.
Is Stage 4 Pancreatic Cancer Terminal?
Stage 4 pancreatic cancer is not curable and it does not have a good prognosis. However, not all cases are defined as terminal cancer. Terminal means a patient is actively dying and will usually die within months. Stage 4 pancreatic cancer is better described as advanced or late-stage cancer.
Stage 4 Pancreatic Cancer Symptoms
One reason that pancreatic cancer gets diagnosed at an advanced stage is that it's easy to miss.
While symptoms of early stage disease are possible, they are not common. When they do occur, they are relatively mild.
Instead, pancreatic cancer symptoms typically only arise when the disease has spread to other organs. Then, many of the symptoms are due to the complications caused by the metastasis.
For example:
. Blood clots: Deep vein thrombosis (DVT) might be the first clue someone has pancreatic cancer. A blood clot in the limbs can cause pain, swelling, and redness.
. Jaundice: Yellowed eyes and skin are caused by a buildup of bilirubin. This may happen because some nearby pancreatic tumors press on the bile duct and cause a blockage. Other symptoms of jaundice include dark urine, light-colored or greasy stools, and itchy skin.
. Gallbladder or liver enlargement: This also is from the buildup of bile.
. Belly or back pain: Tumors that press on other organs or nerves can cause pain.
. Weight loss and poor appetite: This is common in many cancer cases, especially pancreatic cancer.
. Nausea and vomiting: This occurs because of pressure from the tumor on the stomach.
. Diabetes: If the cancer damages the insulin-making cells of the pancreas, it can result in diabetes.
Be sure to talk to a healthcare provider if you have any of these issues.
Diagnosis
About 95% of pancreatic cancers come from the cells that produce digestive enzymes. These are called pancreatic adenocarcinomas (PACs).
The other 5% of cases come from the cells that help regulate blood sugar. These are called pancreatic neuroendocrine tumors (PNETs) and typically have a better prognosis, with a five-year survival rate of 93% when there is no spread to other parts of the body.
Staging of pancreatic cancers requires many tests and procedures to determine how large the original tumor is and how far it has spread. The tests may differ based on whether the lab is testing for a PAC or PNET.
First, blood tests are used to check your general health, test for enzymes, and analyze blood cells. These tests may find:
. High levels of the enzyme amylase in the blood, which may indicate PAC9
. Abnormal blood levels of hormones including insulin, glucagon, and various peptides—signs of a PNET
. Liver function tests, which can help determine how much cancer has affected the liver
Tumor markers in the blood can tell healthcare providers about your cancer. For pancreatic cancer, lower levels of tumor marker CA 19-9 correlate with better outcomes.
Imaging tests, such as computed tomography (CT) and magnetic resonance imaging (MRI), can help healthcare providers see a possible tumor and if/how the mass affects other organs and blood flow.
For pancreatic cancer:
. A multiphase CT scan or a pancreatic protocol CT scan can help visualize the tumor.
. Ultrasound waves may help analyze the tumor. Endoscopic ultrasounds can be more accurate, but they involve inserting a tube down the throat.
. Angiography can look at the blood vessels around the pancreas and other abdominal organs. It can be done using X-ray imaging or an MRI to see how the cancer has affected blood vessels.
. Magnetic resonance cholangiopancreatography uses an MRI machine to get a non-invasive look at the bile and pancreatic ducts.
. Endoscopic retrograde cholangiopancreatography (ERCP) requires a tube down your esophagus and into your stomach. Healthcare providers usually use it to take pictures, do a biopsy, or even perform other treatments, like placing a stent.
A biopsy is when a healthcare provider cuts off a small piece of a possible tumor and looks at it under a microscope to see if it's cancer. For pancreatic cancer, a healthcare provider might do this after imaging tests or during surgery.
Recap
About 95% of pancreatic cancers are called pancreatic adenocarcinomas, or PACs. The other 5% are pancreatic neuroendocrine tumors, or PNETs. They have two different origins in the pancreas, are diagnosed and treated differently, and may have very different outcomes. Blood tests, imaging scans, and biopsy results may all be used for diagnosis.
Treatment
Healthcare providers cannot cure stage 4 pancreatic cancer, but they can manage it. The goal of stage 4 pancreatic cancer treatment is to increase life span and decrease symptoms. This may involve surgery, chemotherapy, radiation, and/or newer drug therapies, all of which are covered here.
Palliative care—which is focused on symptom and stress relief—can help increase quality of life for as long as possible.
It is always a good option to seek a second opinion if you get a stage 4 pancreatic cancer diagnosis. Find a healthcare provider at a National Cancer Institute (NCI) registered cancer center to make sure you’re aware of the latest treatments.
Surgery
Because stage 4 pancreatic cancer has spread throughout the body, surgery to remove it completely is impossible. However, healthcare providers may operate on the pancreatic tumor to increase quality of life or ease pain.
Types of surgery for pancreatic cancer include:
. Whipple surgery: Removes the head of the pancreas, the gallbladder, and parts of the stomach and small intestine.
. Total pancreatectomy: Removes the entire pancreas, along with the gallbladder, bile duct, the spleen, and parts of the stomach, small intestine, and nearby lymph nodes
. Distal pancreatectomy: Removes only the pancreas’ body and tail, but may also remove the spleen if the tumor affects it
. Biliary or gastric bypass: These reroute digestive system structures past a blockage caused by a tumor. This is done as palliative care to relieve symptoms and improve how food moves through the body.
. Stent placement: A stent is inserted to move built-up fluids out of a blocked area for symptom relief. Stents may be placed in the bile ducts or the duodenum, a part of the small intestine.
Chemotherapy
Chemotherapy can improve quality of life and ease cancer symptoms. It kills cancer cells, but does so with toxic chemicals—and without discretion. This means that all rapidly dividing cells in the body (e.g., skin cells, hair cells) can be affected as a consequence.
There are many chemotherapy drugs. Here are several commonly used to treat pancreatic adenocarcinoma, the most common type of pancreatic cancer by far:
. Gemzar (gemcitabine)
. Abraxane (albumin-bound paclitaxel)
. 5-Fluorouracil
. Oxaliplatin
. Irinotecan
Radiation
Radiation kills cancer cells with beams of energy, either locally with an implant or from outside the body. Healthcare providers often use radiation in combination with chemotherapy to shrink a tumor.
Radiation also poses a risk of side effects, including skin changes and hair loss.
Immunotherapies
Immunotherapies support the immune system in its fight against cancer. There are different types, each of which do this in their own way.
For example, Keytruda (pembrolizumab) is a type known as a monoclonal antibody. Some cancer cells have a protein that allows them to trick the immune system into leaving them alone, allowing them to grow without interruption. Keytruda helps interfere with that so the cancer cells are "exposed" and can be attacked, stopping or slowing their growth.
However, not everyone can use immunotherapies. Only about 1% of pancreatic cancer cases have the specific genetic changes that current treatments target. Most people are not screened for pancreatic cancer, either. Genetic testing may benefit people whose history includes familial pancreatic cancer (FPC) because it is linked to a pattern of specific gene mutations.
Immunotherapies are used very rarely in pancreatic cancer.
Targeted Therapies
Targeted therapies are drugs that are designed to target cancer cells specifically. Some are specifically for pancreatic adenocarcinoma. Treatments that block the action of the enzyme tyrosine kinase and may help slow cancer growth include:
. Lynparza (olaparib)
. Rozlytrek (entrectinib)
. Tarceva (erlotinib)
. VitrakviI (larotrectinib)
Clinical Trials
You can get access to other (often experimental) treatment options through clinical trials.
Clinical trials are how researchers test new drugs and treatments. They add to what is already known about treating disease and can help future patients survive longer.
If participating in a trial interests you, first talk to your healthcare provider to get all the information you can about your diagnosis. Then, to find a clinical trial, look in the National Cancer Institute’s clinical trial database and other national databases.
Clinical trials will include new treatments that might not be available otherwise. There’s no promise they’ll work better than others do—or work at all—but there is always that possibility.
Palliative Care
It's also important for stage 4 pancreatic patients to work with a palliative care team. When treatments will not cure the cancer, palliative care therapies can improve quality of life. Specialized doctors, nurses, social workers and other healthcare providers work to relieve symptoms of cancer in seriously ill patients.
Palliative care is not hospice or end-of-life care; these treatments improve patients’ stress levels and daily discomfort and pain. They may include radiation therapy to reduce tumor size and symptoms. For pancreatic cancer, a palliative care treatment plan might include injections or cutting nerves to treat pain from a cancerous pancreas.
Recap
Surgery can't remove a stage 4 pancreatic tumor, but it may be done to improve quality of life. Chemotherapy, radiation, and drugs that target unique aspects of some tumors may be used as well. Clinical trials offer access to still-being-researched options. The addition of palliative care can help with symptom relief and stress.
Prognosis
Stage 4 pancreatic cancers are aggressive and have few treatment options. Even with treatment, survival beyond a year or two is low. Survival rates help healthcare providers estimate how long a person with a diagnosis will survive, given how well other people with that diagnosis have done.
The cancer-specific survival rate is the percentage of people with a particular diagnosis that survived until a specific time.
The SEER database does not use the TNM staging system. Instead, they use a three-stage approach in which stage 4 cancer is classified as a distant cancer, or one that has metastasized to remote parts of the body.
Based on SEER’s data, the five-year survival rate for patients diagnosed with distant pancreatic cancer is 3%. That means 3% of people with metastatic pancreatic cancer are alive five years after their diagnosis.
This number varies by age. Patients diagnosed at a younger age have better odds of survival. For example, those under age 50 diagnosed with distant pancreatic adenocarcinoma have a 10.5% chance of surviving at least five years.
The survival rates in the table below are specifically for PACs.
Survival Rates for Distant Pancreatic Cancer, by Age | |
Age | Survival Rate |
All | 3.0% |
Under 50 | 10.5% |
50-64 | 3.9% |
65 or over | 1.7% |
PNET has an overall five-year survival rate of 51.3%, according to one study.
However, the survival rate depends on a variety of factors, including whether the tumor can be removed using surgery.
The five-year survival rate for people with PNET that has not spread to other parts of the body from where it started is 93%.
If the tumor has spread to nearby tissue or the regional lymph nodes, the five-year survival rate is 77%.
If the tumor has spread to distant areas of the body, the survival rate is 25%.
There are some limitations in survival rates. Some people live well longer than data indicates they might. Rates also don’t accurately portray the impact of advancements in care, since they’re based on numbers from 2010 to 2016.
Recap
Stage 4 pancreatic cancer is a difficult diagnosis. Because the cancer is often found at this later stage, and after it has spread, it is associated with lower survival rates. Yet there is much that healthcare providers can do to improve quality of life in people with pancreatic cancer, and new treatments are becoming available all the time. Be sure that you and your team discuss all the options.
Source:
. https://www.verywellhealth.com/stage-4-pancreatic-cancer-5093642