Intracytoplasmic Sperm Injection (ICSI)
What is Intracytoplasmic Sperm Injection (ICSI)?
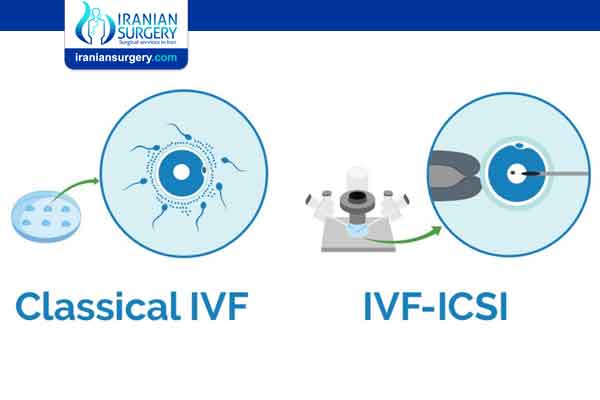
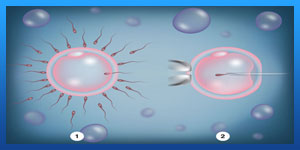
Before a man’s sperm can fertilize a woman’s egg, the head of the sperm must attach to the outside of the egg. Once attached, the sperm pushes through the outer layer to the inside of the egg (cytoplasm), where fertilization takes place.
Read more about : Ivf process in Iran start to finish step by step
Sometimes the sperm cannot penetrate the outer layer, for a variety of reasons. The egg’s outer layer may be thick or hard to penetrate or the sperm may be unable to swim. In these cases, a procedure called intracytoplasmic sperm injection (ICSI) can be done along with in vitro fertilization (IVF) to help fertilize the egg. During ICSI, a single sperm is injected directly into the cytoplasm the egg.
Read more about : Icsi procedure step by step
Before Intracytoplasmic Sperm Injection (ICSI)
Why would I need ICSI?
ICSI helps to overcome fertility problems, such as:
. The male partner produces too few sperm to do artificial insemination (intrauterine insemination [IUI]) or IVF.
. The sperm may not move in a normal fashion.
. The sperm may have trouble attaching to the egg.
. A blockage in the male reproductive tract may keep sperm from getting out.
. Eggs have not fertilized by traditional IVF, regardless of the condition of the sperm.
. In vitro matured eggs are being used.
. Previously frozen eggs are being used.
Risks
ICSI-IVF comes with all the risks of a regular IVF cycle, but the ICSI procedure does introduce additional ones.
A normal pregnancy comes with a 1.5% to 3% risk of major birth defects. ICSI treatment carries a slightly increased risk of birth defects, but it is still rare.
Some birth defects are more likely to occur with ICSI-IVF, specifically Beckwith-Wiedemann syndrome, Angelman syndrome, hypospadias, and sex chromosome abnormalities. They occur in less than 1 percent of babies conceived using ICSI with IVF.
There is also a slightly increased risk of a male baby having fertility problems in the future. This is because male infertility may be passed on genetically.
These additional risks are why many doctors are saying ICSI should not be used for every IVF cycle. It is one thing if you need ICSI to conceive. Then, you can discuss with your doctors the pros and cons of using this assisted reproduction technology. However, if you can have a successful IVF cycle without ICSI, why risk even the slight increase in birth defects?
During Intracytoplasmic Sperm Injection (ICSI)
ICSI Procedure Step by Step
. Step one: Stimulation of the ovaries
In the stimulation phase of an ICSI cycle, you will use injectable medications for approximately 8 to 14 days to stimulate the ovaries to produce eggs. Follicle-stimulating hormone (FSH) and luteinizing hormone (LH), both produced naturally within the body, comprise the medications. During this phase, you will come into the clinic approximately 7 to 8 times for morning monitoring, which allows the team to track the progress of your cycle and adjust medication dosages as needed.
The trigger injection is the final step in the stimulation phase of treatment. Depending on your individual protocol, you will either have a human chorionic gonadotropin (HCG) or a buserelin trigger. This injection helps the developing eggs complete the maturation process and sets ovulation in motion. Timing is very important here, as the doctor must perform the egg retrieval prior to the expected time of ovulation.
Read more about: How long does donor egg IVF take time
Read more about : Type of Infertility Treatment in Iran
Read more about : Egg donation in iran
. Step two: Egg retrieval
On the morning of your egg retrieval, a doctor will meet with you before the procedure to review your protocol. You will also meet with an anesthetist, who will review your medical history and will administer the intravenous fluid you will receive prior to the start of the procedure to induce sleep.
Obtaining the sperm: If you are using a fresh sperm sample, a member of the embryology team will come to accept the sample. If you are using a frozen sperm sample or donor sperm collected previously, the embryologist will verify those details with you. Our andrology laboratory will wash and prepare the sperm, so that the healthiest sperm are brought together with the eggs for fertilization (after the doctor performs the egg retrieval).
Obtaining the eggs: The egg retrieval itself takes about 20 to 30 minutes. During the procedure, the doctor will guide a needle into each ovary to remove the egg-containing fluid in each follicle. The doctor utilises an ultrasound during the procedure to see where to guide the needle. Recovery will take about 30 minutes and you will be able to walk out on your own. It's important that a responsible adult drive you home after the procedure, as it is unsafe to drive after receiving anaesthesia. The person who is driving you will not need to stay at our clinic during your procedure—he or she should anticipate coming back to the clinic after approximately 3 hours.
. Step three: Fertilisation
After the egg retrieval, the embryologist will prepare the eggs and sperm. For PGD the embryologist will inject one single sperm into each mature egg under a microscope. PGD is therefore possible with very few sperm.
. Step four: Embryo development
Embryo development begins after fertilization. After initial fertilisation the embryos will be placed within our Embryoscopes which enables them to continue to develop completely undisturbed. An embryologist examines each developing embryo over the course of the following 5 to 6 days. The goal is to see progressive development, with a two- to four-cell embryo on day 2 and a six- to eight-cell embryo on day 3. After the eight-cell stage, rapid cell division continues and the embryo enters into what is called the blastocyst stage at day 5 or 6. It is your doctor’s goal to transfer the highest-quality embryo(s) to give you the greatest chance of success.
. Step five: Embryo transfer
The embryo transfer is a simple procedure that only takes about 5 minutes to complete. There is no anaesthesia or recovery time needed. When your nurse arranges your transfer, she will notify you and provide instructions on when to arrive and how to prepare. You need to have a full bladder for the procedure as a full bladder ensures good visualization of the lining of the uterus and proper placement of the embryos. It's important to drink the specific amount of liquid recommended 30 to 40 minutes ahead of time.
You will review your cycle with the doctor and the number of embryos recommended for transfer. Upon entering your procedure room, the embryologist will again confirm your last name and the number of embryos for transfer. The embryologist will load the transfer catheter in the embryology lab with the embryo(s) and then the doctor will insert the catheter into the uterus and push the embryo through with a small amount of fluid.
An external abdominal ultrasound provides visual guidance via a monitor to the doctor throughout the procedure. Once the doctor transfers the embryo, he or she will slowly remove the catheter. Since the embryo is invisible to the naked eye, the embryologist will then examine the catheter under a microscope in the lab to ensure that the catheter did indeed release the embryo. The nurse will give you instructions for the following 2 weeks until it's time for the pregnancy test.
. Step six: The pregnancy test
Two weeks after the embryo transfer, you will perform a pregnancy test. This test is frequently called a "beta" because it measures the beta chain portion of the HCG hormone emitted by the developing embryo. We let you do this test in the privacy of your own home using a urinary pregnancy test and you then let us know the outcome so we can plan the next steps.
After Intracytoplasmic Sperm Injection (ICSI)
Success Rate
The ICSI procedure fertilizes 50 to 80 percent of eggs. You might assume all eggs get fertilized with ICSI-IVF, but they don’t. Fertilization isn’t guaranteed even when a sperm is injected into the egg.
Remember that fertilization rates don’t tell you the clinical pregnancy or live birth rates. Once fertilization happens, the success rate for a couple using ICSI with IVF is the same as a couple using regular IVF treatment.
Can ICSI affect a baby’s development?
If a woman gets pregnant naturally, there is a 1.5% to 3% chance that the baby will have a major birth defect. The chance of birth defects associated with ICSI is similar to IVF, but slightly higher than in natural conception.
The slightly higher risk of birth defects may actually be due to the infertility and not the treatments used to overcome the infertility.
Certain conditions have been associated with the use of ICSI, such as Beckwith-Wiedemann syndrome, Angelman syndrome, hypospadias, or sex chromosome abnormalities. They are thought to occur in far less than 1% of children conceived using this technique.
Some of the problems that cause infertility may be genetic. For example, male children conceived with the use of ICSI may have the same infertility issues as their fathers.
Will ICSI work?
ICSI fertilizes 50% to 80% of eggs. But the following problems may occur during or after the ICSI process:
. Some or all of the eggs may be damaged.
. The egg might not grow into an embryo even after it is injected with sperm.
. The embryo may stop growing.
Once fertilization takes place, a couple’s chance of giving birth to a single baby, twins, or triplets is the same if they have IVF with or without ICSI.