Can hysteroscopy help infertility?
How long does a diagnostic hysteroscopy take?
Is diagnostic hysteroscopy painful?
What are the chances of getting pregnant after hysteroscopy?
Should I get a diagnostic laparoscopy for infertility?
How long does it take to recover from a laparoscopy and hysteroscopy?
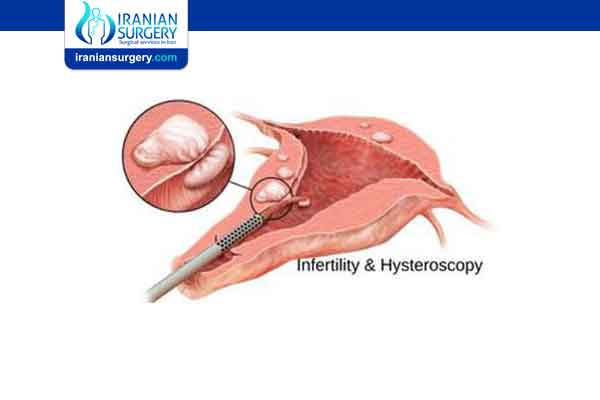
The most common indication for diagnostic hysteroscopy was as a part of an early infertility workup. Other indications included cases being part of a continuous workup either before IVF treatment or after a number of failed IVF cycles. Hysteroscopy revealed a normal uterine cavity in 156 (70%) women
Hysteroscopy is performed approximately half the time for the diagnosis of infertility. It is generally best performed in the postmenstrual proliferative phase. Different locations for hysteroscopy include the office, surgery center, or hospital operating room. Different media include CO2 gas, Sorbitol, glycine, Mannitol/Sorbitol mixture, 5% dextrose in water, or 32% Dextran-70. Endoscopes can range from 2 mm in size to 6.5 mm in size. The choice of location, medium, and instrumentation depends on the availability of facilities and resources, the anticipated diagnosis, and the surgical plan. The optimum approach involves one which has a high probability of resolving the clinical issue at hand, with the major difference in approach depending on whether or not operative intervention will be required, safety, and cost. Adjunctive procedures such as hysterosalpingography and sonohysterography can be of significant help in identifying the patient who requires hysteroscopy, and the best hysteroscopic approach for that patient given the clinical conditions.
Read more about: Hysteroscopy infertility
Can hysteroscopy help infertility?
- investigate symptoms or problems – such as heavy periods, unusual vaginal bleeding, postmenopausal bleeding, pelvic pain, repeated miscarriages or difficulty getting pregnant
- diagnose conditions – such as fibroids and polyps (non-cancerous growths in the womb)
- treat conditions and problems – such as removing fibroids, polyps, displaced intrauterine devices (IUDs) and intrauterine adhesions (scar tissue that causes absent periods and reduced fertility)
A procedure called dilatation and curettage (D&C) used to be common to examine the womb and remove abnormal growths, but now hysteroscopies are carried out instead.
Using hysteroscopy improves fertility and increases pregnancy rates.
Read more about: hysteroscopy infertility workup
Can I get pregnant after hysteroscopy?
Hysteroscopic removal of polyps in women with unexplained infertility may increase their chances of becoming pregnant.
Abnormalities in the uterine cavity, such as endometrial polyps, submucous fibroids, uterine septum, and intrauterine adhesions, may disrupt the process of implantation of a fertilized egg into the inner layer of the cavity of the uterus. In subfertile women with a uterine cavity abnormality, removal of these abnormalities using hysteroscopy may be recommended to help increase the odds of pregnancy. Although the practice is theoretically sound, it is unknown whether hysteroscopic removal of uterine cavity abnormalities results in a definitive increase in pregnancy and live birth rates.
The median duration of days from surgery to the last menstrual period was 60 days ranging from 1 to 270 days. 66.7% (12/18) and 94.4% (17/18) of the patients were conceived within postoperative 3 months and 6 months, respectively.
Read more about: Can hysteroscopy cause infertility?
How long does a diagnostic hysteroscopy take?
A hysteroscopy is usually carried out on an outpatient or day-case basis. This means you do not have to stay in hospital overnight.
It may not be necessary to use anaesthetic for the procedure, although local anaesthetic (where medication is used to numb your cervix) is sometimes used.
General anaesthetic may be used if you're having treatment during the procedure or you would prefer to be asleep while it's carried out.
A hysteroscopy can take up to 30 minutes in total, although it may only last around 5 to 10 minutes if it's just being done to diagnose a condition or investigate symptoms.
Read more about: Hysteroscopy for unexplained infertility
Is diagnostic hysteroscopy painful?
This seems to vary considerably between women. Some women feel no or only mild pain during a hysteroscopy, but for others the pain can be severe.
If you find it too uncomfortable, tell the doctor or nurse. They can stop the procedure at any time.
If you're worried, speak to the doctor or nurse before having the procedure about what to expect and ask them about pain relief options.
Read more about: Assisted hatching ivf
What are the chances of getting pregnant after hysteroscopy?
If 28% of women become pregnant without surgery, the evidence suggests that about 63% of women will become pregnant following removal of polyps. The real clinical value of hysteroscopic removal of uterine cavity abnormalities to increase fertility rates in subfertile women remains unknown. The limited evidence shows that hysteroscopy may improve the odds of a clinical pregnancy.
Read more about: IUI vs. IVF
Should I get a diagnostic laparoscopy for infertility?
Laparoscopy for infertility is generally only performed after other fertility tests have not resulted in a conclusive diagnosis. For this reason, laparoscopy is often performed on women with unexplained infertility.
Laparoscopy also allows for biopsy of suspect growths and cysts that may be hampering fertility. Laparoscopy may be recommended for women experiencing pelvic pain, which is a potential symptom of endometriosis. Laparoscopy can also remove scar tissue that can be a cause of pelvic or abdominal pain.
Read more about: Ivf
How long does it take to recover from a laparoscopy and hysteroscopy?
Laparoscopy recovery
After laparoscopy, you may feel groggy and disorientated as you recover from the effects of the anaesthetic. Some people feel sick or vomit. These are common side effects of the anaesthetic and should pass quickly.
You'll be monitored by a nurse for a few hours until you're fully awake and able to eat, drink and pass urine.
Before you leave hospital, you'll be told how to keep your wounds clean and when to return for a follow-up appointment or have your stitches removed (although dissolvable stitches are often used).
For a few days after the procedure, you're likely to feel some pain and discomfort where the incisions were made, and you may also have a sore throat if a breathing tube was used. You'll be given painkilling medication to help ease the pain.
Some of the gas used to inflate your abdomen can remain inside your abdomen after the procedure, which can cause:
- bloating
- cramps
- shoulder pain, as the gas can irritate your diaphragm (the muscle you use to breathe), which in turn can irritate nerve endings in your shoulder
These symptoms are nothing to worry about and should pass after a day or so, once your body has absorbed the remaining gas.
In the days or weeks after the procedure, you'll probably feel more tired than usual, as your body is using a lot of energy to heal itself. Taking regular naps may help.
The time it takes to recover from laparoscopy is different for everybody. It depends on factors such as the reason the procedure was carried out (whether it was used to diagnose or treat a condition), your general health and if any complications develop.
If you've had laparoscopy to diagnose a condition, you'll probably be able to resume your normal activities within 5 days.
The recovery period after laparoscopy to treat a condition depends on the type of treatment. After minor surgery, such as appendix removal, you may be able to resume normal activities within 3 weeks. Following major surgery, such as removal of your ovaries or kidney because of cancer, the recovery time may be as long as 12 weeks.
Your surgical team can give you more information about when you'll be able to resume normal activities.
Read more about: How painful are IVF injections?
Hysteroscopy recovery
Your recovery will vary based on the type of anesthesia you have. If your provider used general anesthesia or a sedative, he or she will track your blood pressure, pulse, and breathing until they are stable and you are alert. When stable, you will be discharged to your home. Hysteroscopy is most often done on an outpatient basis.
Otherwise, you won’t need any special care after a hysteroscopy.
You may have cramping and vaginal bleeding for a day or two after the procedure. Report fever, severe abdominal pain, or heavy vaginal bleeding or discharge.
You may have gas in the digestive tract and pains from the gas given during the procedure. This can last for about 24 hours. You may also feel pain in your upper belly and shoulder.
Take a pain reliever for soreness as advised by your healthcare provider. Aspirin or certain other pain medicines may increase the chance of bleeding. Be sure to take only recommended medicines.
Don't douche or have sex for 2 weeks after the procedure, or as advised by your healthcare provider.
You can go back to normal activity and diet unless your healthcare provider tells you otherwise.
Most women feel they can return to normal activities, including work, the day after having a hysteroscopy. Some women return to work later the same day.
However, you may wish to have a few days off to rest, particularly if you had treatment such as fibroids removal and/or a general anaesthetic was used.
Your doctor or surgeon can advise you about any activities you need to avoid while you recover, but generally speaking:
- you can eat and drink as normal straight away– if you feel a bit sick after a general anaesthetic, try eating small, light meals at first
- you can have a shower the same day and a bath the next day, unless your doctor advises you differently. If you have had a general anaesthetic you may still be feeling dizzy so it is a good idea to make sure there is another adult around to help you
- you should avoid having sex for a week, or until any bleeding stops– this will help to reduce the risk of infection
Read more about: ICSI IVF procedure
Is hysteroscopy safe?
Hysteroscopy is a relatively safe procedure. However, as with any type of surgery, complications are possible. With hysteroscopy, complications occur in less than 1% of cases and can include:
- Risks associated with anesthesia.
- Heavy bleeding.
- Injury to the cervix, uterus, bowel or bladder.
- Intrauterine scarring.
- Reaction to the substance used to expand the uterus.
Read more about: Ivf with donor eggs process in Iran

