What is the best treatment for a compression fracture?
Can old compression fractures cause pain?
Can a compression fracture get worse?
How are compression fractures treated in the elderly?
Do bones take longer to heal in the elderly?
What is the most common fracture in the elderly?
A compression fracture is a type of fracture or break in your vertebrae. The vertebrae are the bones in your back that are stacked on top of each other to make your spine. Your spine supports your weight, allows you to move, and protects your spinal cord and the nerves that go from it to the rest of your body.
Compression fractures can cause the vertebrae to collapse, making them shorter in height. This collapse can also cause pieces of bone to press on the spinal cord and nerves, decreasing the amount of blood and oxygen that gets to the spinal cord.
A well-balanced diet, regular exercise program, calcium and vitamin D supplements,28 smoking cessation, and medications to treat osteoporosis (such as bisphosphonates) may help prevent additional compression fractures.
Read more about : Leg lengthening surgery success story in Iran
Read more about : Total knee replacement surgery success story in Iran
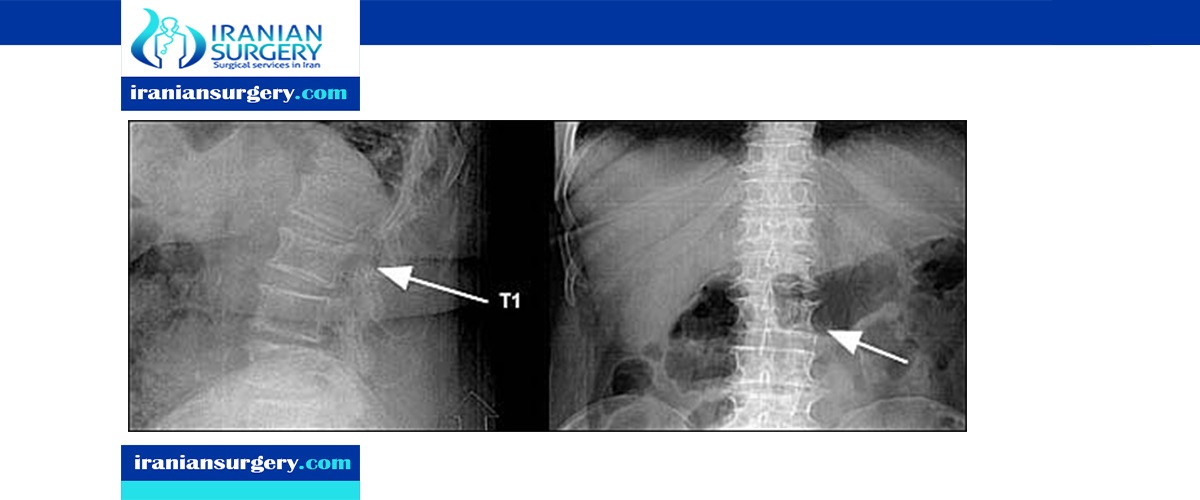
Compression fracture of the vertebral body is common, especially in older adults. Vertebral compression fractures usually are caused by osteoporosis, and range from mild to severe. More severe fractures can cause significant pain, leading to inability to perform activities of daily living, and life-threatening decline in the elderly patient who already has decreased reserves. While the diagnosis can be suspected from history and physical examination, plain roentgenography, as well as occasional computed tomography or magnetic resonance imaging, are often helpful in accurate diagnosis and prognosis. Traditional conservative treatment includes bed rest, pain control, and physical therapy. Interventional procedures such as vertebroplasty can be considered in those patients who do not respond to initial treatment. Family physicians can help patients prevent compression fractures by diagnosing and treating predisposing factors, identifying high-risk patients, and educating patients and the public about measures to prevent falls.
Read more about: Best way to sleep with compression fracture
What is the best treatment for a compression fracture?
Treatment for the vertebral fracture will typically include non-surgical care, such as rest, pain medication, use of heat or ice for local pain, and slow return to mobility. Surgery may also be advisable. If your compression fracture is related to osteoporosis, your healthcare provider will want to treat the osteoporosis. You may need to take bone-strengthening medicine and calcium and vitamin D supplements. Physical therapy and exercises may be recommended, too. These things help make your bones stronger and can help prevent other fractures.
Other types of treatment include:
- Pain medicine to relieve your back pain
- Bed rest for a short time, followed by limited activity while your bones heal
- Wearing a back brace
- Physical therapy to help you move better and strengthen the muscles around your spine
Different types of surgery are available and may be needed if other treatments aren't helping:
- Vertebroplasty. Using an X-ray for guidance, your surgeon uses a small needle to inject special quick-setting cement into your fractured vertebra. The cement provides support for the broken vertebra, strengthens the area, and usually results in pain relief.
- Kyphoplasty. This surgery is a lot like vertebroplasty. But before the cement is injected, small balloons are used to expand the fractured space to help make the vertebra taller. The balloons are removed, and then the empty space is filled with cement.
If a cancerous tumor is causing your symptoms, you may need radiation therapy as well as surgery to remove some of the bone and treat the tumor. If an injury has caused the fracture, you may need surgery to repair the bone and join vertebrae together. This is a procedure called fusion.
Read more about: spine compression fractures treatment
Can old compression fractures cause pain?
A vertebral body compression fracture is a type of fracture in the spine in which a vertebral bone has decreased at least 15 to 20 percent in height due to fracture. They are followed by acute back pain and may lead to chronic pain, deformity, loss of height, and crowding of internal organs. Pain from a spinal compression fracture allowed to heal naturally can last as long as three months. But the pain usually improves significantly in a matter of days or weeks. Many people who fracture will eventually heal and recover to the point where they no longer experience any pain. However, some people may continue to experience pain long after the fracture and soft tissues have healed.
Read more about: vertebral compression fractures treatment
Can a compression fracture get worse?
The main symptom you’ll notice with a spinal compression fracture is back pain. It may start gradually and get worse over time or come on suddenly and sharply. But regardless of how it happens, it’s important to let your doctor know about it, especially if you’re a woman who is near or over age 50. When a compression fracture starts harming vertebrae, you may feel: Slowly worsening back pain lying on your back may relieve the pain and standing may make it worse. Pain that gets worse when you stand or walk but with some relief when you lie down.
Read more about: Can spinal tumors be cured?
How are compression fractures treated in the elderly?
The physician must first determine if the fracture is stable or unstable. A stable fracture will not be displaced by physiologic forces or movement. Fortunately, compression fractures are normally stable secondary to their impacted nature. Traditional treatment is nonoperative and conservative. Patients are treated with a short period (no more than a few days) of bedrest. Prolonged inactivity should be avoided, especially in elderly patients. Oral or parenteral analgesics may be administered for pain control, with careful observation of bowel motility. If bowel sounds and flatus are not present, the patient may require evaluation and treatment for ileus. Calcitonin-salmon (Miacalcin) nasal spray can be used for treatment of pain. Muscle relaxants, external back-braces, and physical therapy modalities also may help. [Evidence level B] Nonsteroidal anti-inflammatory drugs have been shown to significantly increase gastrointestinal bleeding in the elderly and must be used with caution.
Read more about: cervical fracture symptoms
Do bones take longer to heal in the elderly?
When kids or young adults break a bone, they might have weeks or months of recovery to get through. But they can usually expect to get back to their prefracture level of functioning. For older adults, the stakes of a fracture can be much higher. All through your life, your body is continually removing old bone and replacing it with fresh bone. This process is called remodeling. Up until about age 40, all the bone removed is replaced. After age 40, however, less bone is replaced. With increasing age, perturbations in bone fracture healing are associated with age-related dysfunction to the bone vascular system and its ability to regenerate in healing. Generally, the vascular perfusion of the skeleton decreases with age.
Read more about: Spinal stenosis treatment
What is the most common fracture in the elderly?
Older adults are prone to different fractures and fracture mechanisms than a younger cohort. The fracture incidences tend to change after age 50, when post-menopausal changes to BMD start. The most common fractures in older adults are vertebral fracture from compression or trauma, followed by hip and distal radius fractures. One in two women and one in five men will suffer from an osteoporotic fragility fracture, which is defined as any low-energy trauma fracture. The most common fragility fractures are proximal humerus, hip, distal radius, and spinal fractures.
Read more about: How to get out of bed with a compression fracture?