Ureteral Stenting and Nephrostomy procedure in Iran
Ureteral Stenting and Nephrostomy procedure in iran
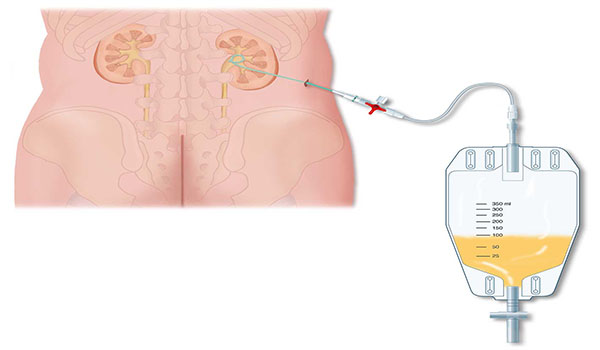
Ureteral stenting and nephrostomy help restore urine flow through blocked ureters and return the kidney to normal function. Ureters are long, narrow tubes that carry urine from the kidneys to the bladder. They can become obstructed – and urine flow blocked – as a result of various conditions. Your doctor may use image guidance to place a thin, flexible tube called a stent into the ureter to restore urine flow. If a stent cannot be placed, he may perform a nephrostomy, during which a tube is placed through the skin into the kidney and connected to either an external drainage bag or the bladder for internal drainage.
Tell your doctor if there is a possibility you are pregnant and discuss any recent illnesses, medical conditions, allergies and medications you're taking. Your doctor may advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners several days prior to your procedure and instruct you not to eat or drink anything after midnight the night before. Take regular medication with sips of water. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. If you are not to be admitted to the hospital, plan to have someone drive you home afterward.
What are Ureteral Stenting and Nephrostomy?
Urine is normally carried from the kidneys to the bladder through long, narrow tubes called ureters. The ureter can become obstructed due to conditions such as kidney stones, tumors, infection, or blood clots. When this happens, physicians can use image guidance to place stents or tubes in the ureter to restore the flow of urine to the bladder.
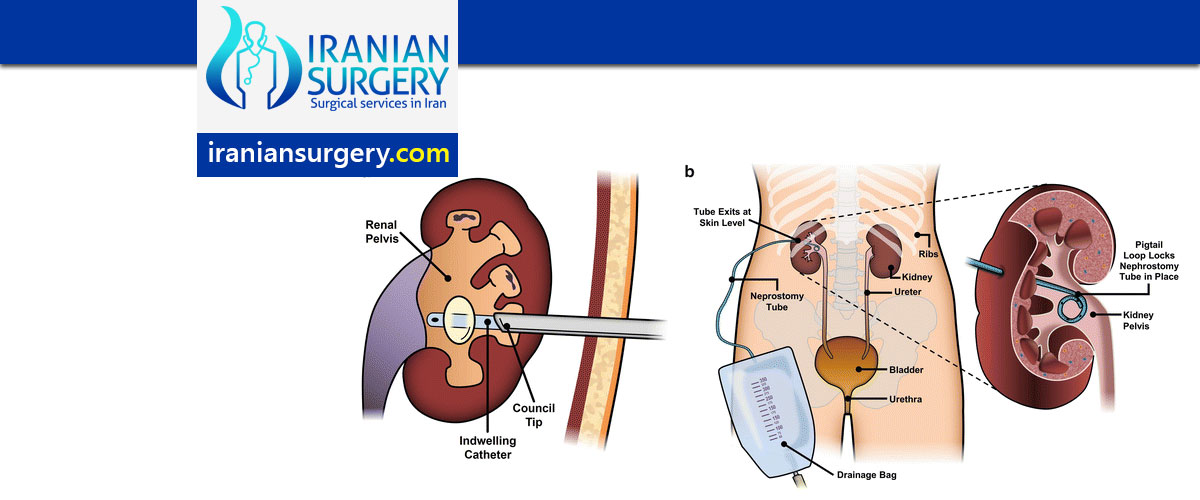
A ureteral stent is a thin, flexible tube threaded into the ureter. When it is not possible to insert a ureteral stent, a nephrostomy is performed. During this procedure, a tube is placed through the skin on the patient's back into the kidney. The tube is connected to an external drainage bag or from the kidney to the bladder for internal drainage.
Before procedure
You might have blood drawn prior to your procedure.
Prior to your procedure, your blood may be tested to determine how well your kidneys are functioning and whether your blood clots normally.
You should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to local anesthetic medications, general anesthesia or to contrast materials containing iodine (sometimes referred to as "dye" or "x-ray dye"). Your physician may advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners for a specified period of time before your procedure.
Also inform your doctor about recent illnesses or other medical conditions.
Women should always inform their physician and x-ray technologist if there is any possibility that they are pregnant. Many imaging tests are not performed during pregnancy so as not to expose the fetus to radiation. If an x-ray is necessary, precautions will be taken to minimize radiation exposure to the baby. See the Safety page for more information about pregnancy and x-rays.
In general, you should not eat or drink anything after midnight the day of your procedure. However, you may take your routine medications with sips of water. If you are diabetic and take insulin, you should talk to your doctor as your usual insulin dose may need to be adjusted.
You will be given a gown to wear during the procedure.
You should plan to have a relative or friend drive you home after your procedure.
What does the equipment look like?
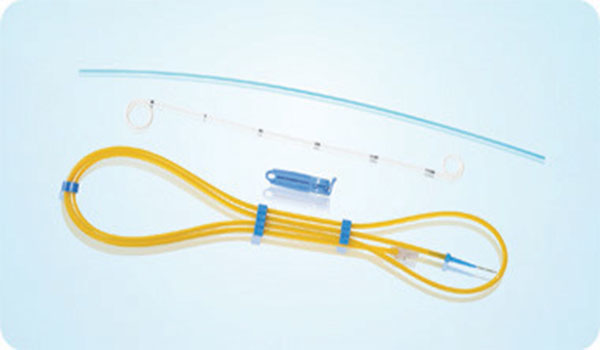
During ureteral stenting, a fluoroscope and a guide wire are used to place a stent into the ureter.
A guide wire may be inserted with the aid of a fluoroscope, an imaging device that uses x-rays to see structures on a fluorescent screen.
A stent is 10 to 15 inches long and less than a quarter inch thick.
During a nephrostomy, a fluoroscope, or an ultrasound, and a needle are used to place a catheter in the kidney.
A catheter is a long, thin plastic tube that is considerably smaller than a "pencil lead", or approximately 1/8 inch in diameter.
Ultrasound scanners consist of a console containing a computer and electronics, a video display screen and a transducer that is used to do the scanning. The transducer is a small hand-held device that resembles a microphone, attached to the scanner by a cord. Some exams may use different transducers (with different capabilities) during a single exam. The transducer sends out high-frequency sound waves (that the human ear cannot hear) into the body and then listens for the returning echoes from the tissues in the body. The principles are similar to sonar used by boats and submarines.
The ultrasound image is immediately visible on a video display screen that looks like a computer or television monitor. The image is created based on the amplitude (loudness), frequency (pitch) and time it takes for the ultrasound signal to return from the area within the patient that is being examined to the transducer (the device placed on the patient's skin to send and receive the returning sound waves), as well as the type of body structure and composition of body tissue through which the sound travels. A small amount of gel is put on the skin to allow the sound waves to travel from the transducer to the examined area within the body and then back again. Ultrasound is an excellent modality for some areas of the body while other areas, especially air-filled lungs, are poorly suited for ultrasound.
Other equipment that may be used during the procedure includes an intravenous line (IV), ultrasound machine and devices that monitor your heart beat and blood pressure.
How are these procedures performed?
Image-guided, minimally invasive procedures such as ureteral stenting and nephrostomy are most often performed by a specially trained interventional radiologist in an interventional radiology suite or occasionally in the operating room.
This procedure is often done on an outpatient basis. However, some patients may require admission following the procedure. Please consult with your physician as to whether or not you will be admitted.
Prior to your procedure, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) may be performed.
You may be given medications to help prevent nausea and pain, and antibiotics to help prevent infection.
You may be connected to monitors that track your heart rate, blood pressure and pulse during the procedure.
A nurse or technologist will insert an intravenous (IV) line into a vein in your hand or arm so that sedative medication can be given intravenously. Moderate sedation may be used. As an alternative, you may receive general anesthesia.
If you receive moderate sedation, you will be asleep but have the ability to be awakened. The sedation will be administered and monitored by your physician and nursing staff.
If you receive a general anesthetic, you will be unconscious for the entire procedure, and you will be monitored by an anesthesiologist. If you receive conscious sedation, you will be monitored by a nurse who will administer medications to make you drowsy and comfortable for the procedure.
The area of your body where the catheter is to be inserted will be sterilized and covered with a surgical drape.
Your physician will numb the area with a local anesthetic.
The interventional radiologist will use x-rays and/or ultrasound to locate your kidney and a needle will be inserted through your skin into the kidneys. Contrast material will be injected through the needle.
During ureteral stenting, you are positioned on your stomach. Using a fluoroscope to see the ureter, a guide wire is inserted into the ureter. The stent is run over the guide wire and placed in its permanent position within the ureter. Once the stent has been placed, the guide wire may be removed, or a nephrostomy catheter may be left in place for a day or two and then removed.
At the end of the procedure, the catheter will be removed and pressure will be applied to stop any bleeding. The opening in the skin is then covered with a dressing. No sutures are needed.
During nephrostomy, you are positioned on your stomach. Using a fluoroscope to see the kidney, a guide wire is inserted into the kidney, followed by a catheter. This will be left in place until a ureteral stent can be placed or the ureteral blockage is resolved. Most commonly, the nephrostomy catheter is connected to an external bag that collects urine. Prior to leaving the hospital, you will be instructed on how to empty and care for the drainage bag. For prolonged durations, the catheter may require routine check and changes every two to three months.
Your intravenous line will be removed.
Both procedures are usually completed within one hour.
What will I experience during and after the procedure?
Devices to monitor your heart rate and blood pressure will be attached to your body.
You will feel a slight pin prick when the needle is inserted into your vein for the intravenous line (IV) and when the local anesthetic is injected. Most of the sensation is at the skin incision site, which is numbed using local anesthetic. You may feel pressure when the catheter is inserted into the vein or artery.
If the procedure is done with sedation, the intravenous (IV) sedative will make you feel relaxed, sleepy and comfortable for the procedure. You may or may not remain awake, depending on how deeply you are sedated.
You may feel slight pressure as the catheter is inserted into the kidney and down the ureter. During placement of a ureteral stent, until the stent is positioned, you may feel pressure as the guide wire is inserted into the bladder resulting in a sensation to urinate. You may experience blood-tinged urine for several days following the procedure, which will usually clear up on its own.
You will remain in the recovery room until you are completely awake and ready to return home.
You will not feel when the contrast is excreted into the urine.
You should be able to resume your normal activities within a few days.
Who interprets the results and how do I get them?
The interventional radiologist can advise you as to whether the procedure was a technical success when it is completed.
Your interventional radiologist may recommend a follow-up visit after your procedure or treatment is complete.
The visit may include a physical check-up, imaging procedure(s) and blood or other lab tests. During your follow-up visit, you may discuss with your doctor any changes or side effects you have experienced since your procedure or treatment.
What are the benefits vs. risks?
Benefits
A ureteral stent or nephrostomy catheter will allow urine to flow again from the kidney and permit the kidney to function normally.
Risks
Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
Rarely, you may experience ongoing spasm of the bladder after placement of a ureteral stent. If this happens, notify you doctor. This spasm may be treated with medication.
Because the kidney is an organ with a substantial amount of blood flow to it, bleeding is a possible but rare complication. There is also a small risk of damage to surrounding organs. Imaging guidance is used to minimize this risk.
There is a very slight risk of an allergic reaction if contrast material is injected.
10 common Questions about ureteral stenting and nephrostomy procedure
[kkstarratings]