tympanoplasty surgery in Iran
tympanoplasty surgery in Iran
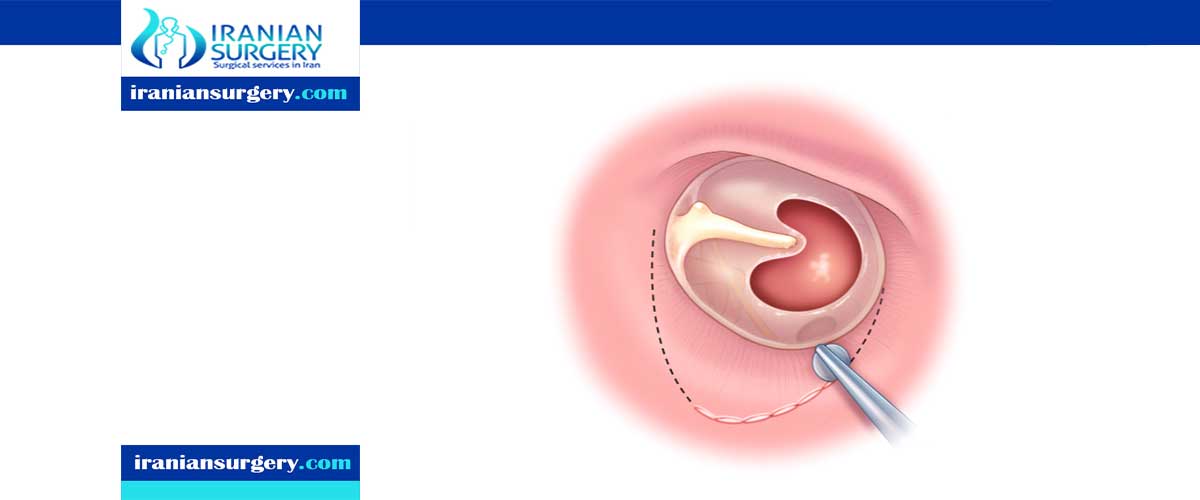
Tympanoplasty is a surgical technique to repair a defect in the tympanic membrane with the placement of a graft, either medial or lateral to the tympanic membrane annulus. The goal of this surgical procedure is not only to close the perforation but also to improve hearing. The success of the operation depends on the ability to eradicate disease from the middle ear (e.g., inflamed granulation tissue and cholesteatoma). Various techniques have been developed and refined, and a number of grafting materials are available
How to prepare for tympanoplasty surgery in Iran
Your health care provider will tell you what and when your child can eat and drink before the surgery. Your child's stomach must be empty on the day of the procedure.
You can help prepare your child and ease any fears by talking about what to expect during and after the tympanoplasty.
During the tympanoplasty surgery in Iran
A graft consisting of cartilage, fat (often harvested from behind the ear), or fascia (tissue overlaying muscle) is used to reconstruct the eardrum. Depending on the size and location of the perforation, tympanoplasty can be performed in the procedure room under local anaesthetic. In this case, the surgeon enters through the external ear canal.
In more complex cases, tympanoplasty may be performed in the operating room under general anaesthetic. In the operating room, the surgeon may decide to either make a small incision above the ear canal to approach the repair (endaural incision) or they can go behind the ear (post-auricular).
Aftercare tympanoplasty surgery in Iran
Full tympanoplasty surgery recovery time can be 2 to 3 months. In fact, the hearing will probably be worse than it was before surgery until this packing dissolves. At the first postoperative visit, your doctor may gently clean the ear canal with a vacuum in order to inspect the reconstructed eardrum.
tympanoplasty surgery complications in Iran
Pain, infection and bleeding are complications of any surgical procedure. These are fortunately rare in ear surgery. Blood loss after tympanoplasty surgery is usually too small to measure. The ear is numbed with long lasting drugs that generally keep the patient comfortable for many hours. Most patients use Tylenol or Motrin/Advil for pain. Narcotics are occasionally used. Infection after ear surgery is very rare. Antibiotics are used for 1 week after medial and lateral tympanoplasty.
The most common complication is failure of the hole to heal. The frequency of this depends on its size, location, health of the ear and procedure chosen. It can occur in up to 8% of difficult cases. Most patients can then go on to have revision surgery which is usually successful. A second complication is hearing loss. Most patients enjoy improvement of their hearing after successful tympanoplasty but scar tissue formation, Eustachian tube problems and problems with the bones in the middle ear can result in on-going hearing loss. The hearing can rarely be worse after surgery. Conductive, sensorineural or mixed hearing loss may occur. Tinnitus, or ringing in the ear can occur if the hearing worsens.
Taste change can occur after ear surgery due to a nerve of taste that runs under the eardrum and brings taste to the side of the tongue. Loss of taste on the side of the tongue can occur in up to 10% of ear procedures and last for a few months. It can rarely be permanent and is more of a problem in patients who have had surgery in their other ear.
Vertigo and dizziness are common after ear surgery but is usually short-lived and rarely persists. Many medications are given during surgery to prevent nausea and vomiting.
Facial nerve paralysis is a very rare complication of ear surgery. The facial nerve travels through the ear and can rarely be injured during surgery. A facial nerve monitor is used during medial and lateral tympanoplasty which delivers an EMG of the facial nerve to prevent injury.
Risks of tympanoplasty surgery in Iran
- Hearing loss: There is a slight chance of hearing loss in the inner ear. This loss can be complete and permanent.
- Dizziness: Some patients experience dizziness that resolves within a day of surgery. It is not likely for dizziness to be a persistent problem.
- Facial paralysis: The nerve that innervates the muscle of the face courses through the ear. Therefore, there is a slight chance of a facial paralysis. The facial paralysis affects the movement of the facial muscles for closing of the eye, making a smile and raising the forehead. The paralysis could be partial or complete. It may occur immediately after surgery or have a delayed onset. Recovery can be complete or partial.
- Tinnitus: Tinnitus, or noises in the ear, can occur with surgery, but is an uncommon post-operative problem.
- Taste abnormalities: A small nerve that innervates some of the taste and salivary function courses through the ear. After ear surgery, some patients experience an abnormal taste in the mouth or some dryness of the mouth. Many times, this problem will improve over time.
10 common questions about tympanoplasty surgery in Iran
[kkstarratings]


