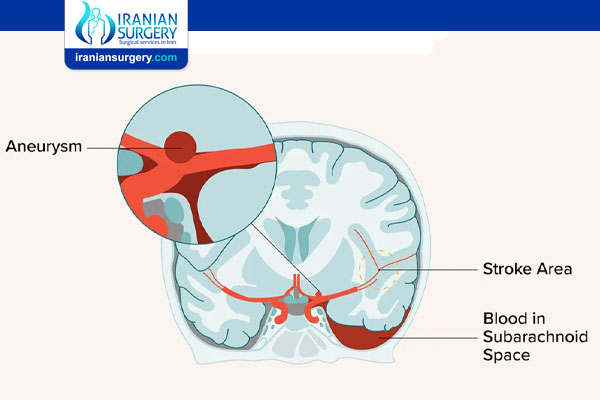
Subarachnoid Hemorrhage
Subarachnoid hemorrhage (SAH) refers to bleeding within the subarachnoid space, which is the area between the brain and the tissues that cover the brain. The subarachnoid space is the space where the cerebrospinal fluid circulates, and it’s responsible for protecting your brain from injury by serving as a cushion. A hemorrhage in this space can cause a coma, paralysis, and even death. This life-threatening condition is also rare. SAH accounts for 1 percent of visits to the emergency room due to headaches.
Symptoms of SAH
When SAH develops, it has several symptoms. The main symptom is a sudden, severe headache, which is more intense at the base of the skull. It’s often described as the worst headache people have ever experienced. Some people may even feel a popping sensation in their head before the hemorrhage begins.
You may also have:
. severe head, neck, and shoulder pain
. seizures
. confusion and rapid loss of alertness
. nausea
. vomiting
. dizziness
. difficulty walking or standing
. vision changes
. difficulty speaking or understanding others
. loss of consciousness
The symptoms of SAH come on suddenly, and you may lose consciousness quickly. Seek emergency medical attention right away if you experience any of these symptoms combined with a severe headache.
Causes of SAH
SAH can occur spontaneously, or as a result of head trauma. Spontaneous SAH is often related to brain aneurysms, which are abnormalities within the brain’s arteries. The most common cause of primary SAH is a berry aneurysm. It’s called a berry aneurysm because it forms a cluster of sac-like pouches in a cerebral vessel that looks like a cluster of berries. These aneurysms swell up and weaken the walls of the arteries over time. When an aneurysm erupts, it quickly bleeds. This condition is responsible for most SAH cases.
Other causes of SAH include:
. bleeding from an arteriovenous malformation (AVM)
. bleeding disorders
. use of blood thinners
A serious head injury, such as one that occurs in a car crash, can also lead to an SAH. Aneurysmal hemorrhage may occur at any age, but it’s most common between ages 40 and 60. Brain aneurysms are more common in women, people who smoke, and those with high blood pressure. In some cases, trauma to the brain during an injury can cause aneurysms and result in a subarachnoid hemorrhage.
Risk factors for SAH
SAH can occur at any age, and some people are even born with cerebral aneurysms that can lead to this condition. According to the National Institute of Neurological Disorders and Stroke, women are more likely than men to develop brain aneurysms, and thus SAH. Smoking and high blood pressure can also increase your risk of developing an aneurysm. Drug use, particularly methamphetamine and cocaine, dramatically increases the risk of having SAH.
According to the Brain Aneurysm Foundation, 1 in 50 people is estimated to have an unruptured aneurysm in the United States. You should speak with a doctor about your risk if you have a history of brain aneurysms. If you have aneurysms, it’s important to see your doctor regularly to determine your risk of hemorrhaging — before SAH develops.
Diagnosing SAH
Signs of SAH are usually severe, and most people seek medical attention for symptoms of SAH. In some cases, a person may lose consciousness, and others may call for emergency help.
A physical examination can show signs of SAH such as a stiff neck, reflex changes, or changes in motor function. You’ll need more testing to find out if an SAH is causing your symptoms and to determine the location and severity of the hemorrhage so you can get proper treatment.
First, a doctor may conduct a CT scan of the head to look for bleeding in your skull. If the results are inconclusive, the doctor may use a contrast dye during the procedure.
Other tests include:
. MRI, which uses radio waves to get clear, detailed images of the brain
. cerebral angiography, which uses an X-ray and injected dye to detect blood flow in the brain
. transcranial ultrasound, which detects blood flow in the arteries within the brain
. lumbar puncture to see if blood cells are found in the cerebrospinal fluid (this test is not always done and may pose a risk if you have had an SAH that increases the risk of herniation)
Sometimes, SAH may cause moderately painful headaches or headaches that get better with pain relievers. If an SAH is very small, it might not be detected.
Treating SAH
Rapid treatment is important to save your life and reduce the possibility and extent of brain damage. Bleeding and pressure may build up in the brain, leading to coma and additional brain damage. This pressure needs to be alleviated by medications or a procedure to remove blood. Second, the cause of the bleeding needs to be identified and treated, as new bleeding from the same aneurysm can frequently occur without treatment. Surgery is performed to clip, or repair, the aneurysm and stop future bleeding.
If an aneurysm is being clipped, a craniotomy is performed and the aneurysm is repaired. A craniotomy involves opening the skull to expose the affected area. A technique called endovascular coiling may also be used to reduce the risk of further bleeding.
If SAH causes a coma, treatment will include appropriate support with mechanical ventilation, protection of the airways, and placement of a draining tube in the brain to relieve pressure.
If you don’t lose consciousness from the SAH, you’ll be given strict instructions to prevent complications such as swelling or additional bleeding in the brain.
Bed rest is standard for people recovering from this condition. Your doctor will also ask you to avoid straining your body or bending over. These actions can increase the pressure on your brain.
Your doctor may prescribe medications to:
. regulate blood pressure with medication through an IV
. prevent artery spasms with nimodipine
. relieve severe headaches with pain relievers
. relieve anxiety and agitation with anti-anxiety medications
Recovery From a Subarachnoid Hemorrhage
Recovery is different for each person. It can take months or years. The time it takes to recover depends on many factors, including the cause and severity of the SAH. During recovery, you might experience:
. Headaches. These headaches are milder than those caused by a SAH and can be managed with pain relievers. The headaches usually get better over time.
. Strange sensations. You might have a strange “tickly“ feeling in your head. Like headaches, these sensations should go away over time.
. Fatigue. It’s normal to feel very tired during the first few months of recovery. You may need to take frequent breaks throughout the day.
. Sleeping problems. Insomnia commonly affects people during recovery. It might help to follow a daily routine and take frequent breaks.
. Loss of movement or feeling. You might lose some movement or sensation on one side of your body.
. Changes in senses. Your sense of taste and smell may change during recovery. Typically, these changes are temporary.
. Vision changes. It’s common to develop vision changes like blurring, black spots, and double vision. These changes usually go away after a couple of months.
. Mood disorders. You might experience depression or anxiety during the recovery process.
What Follow-Up Is Needed After a Subarachnoid Hemorrhage?
Rehabilitation is an essential part of SAH recovery. It involves regular follow-up appointments that will support recovery and improve quality of life. After a SAH, you will need to receive the following therapies:
. Physical therapy. A physical therapist can teach you exercises and other techniques for regaining movement.
. Speech therapy. Speech therapy can help improve your ability to speak and communicate.
. Occupational therapy. Occupational therapy may improve your ability to perform basic tasks like bathing and making food.
. Psychotherapy. A mental health professional can help you cope with the recovery process.
You will also need to meet with a neuropsychologist or neuropsychiatrist before returning to work.
What Are the Complications Of SAH?
Even after SAH treatment, you may be at risk of related complications. The most common is called repeated bleeding. This happens when a rupture that has healed itself ruptures again. Repeated bleeding can increase your risk of death. Comas due to SAH can also eventually lead to death. In some cases, people may experience seizures or strokes due to brain damage from SAH, and the effects can last.
How Can I Prevent SAH?
The only way to prevent this condition is to identify potential problems within the brain. Early detection and, in some cases, treatment of a brain aneurysm can prevent a subsequent hemorrhage in the subarachnoid space.
What Is the Long-Term Outlook For SAH?
SAH is a serious condition that can frequently be fatal. The recovery period is long, and you may be at a higher risk of complications if you’re older or have poor overall health. The earlier you seek emergency medical care, the better your chances of survival.
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best doctors and surgeons in Iran. The price of Subarachnoid Hemorrhage Treatment in Iran can vary according to each individual’s case and will be determined by an in-person assessment with the doctor.
For more information about the cost of Subarachnoid Hemorrhage Treatment in Iran and to schedule an appointment in advance, you can contact Iranian Surgery consultants via WhatsApp number 0098 901 929 0946. This service is completely free.
Source:
https://www.healthline.com/health/subarachnoid-hemorrhage


4 Comments
Ciao a tutti vengo dall’italia
ciao how can I help you?
hello everyone thanks for approve
hi guys :). I am looking for help for me and my girl. i am from France