Single-Port Radical Prostatectomy
Single-Port Radical Prostatectomy
What is a Single Port Radical Prostatectomy?
Single port radical prostatectomy is a surgery that removes the entire prostate through a single incision in the abdomen. A prostatectomy can be done in an open surgery as well. However, because of the ability of experienced surgeons to reduce abdominal wall trauma in a laproscopic or robotic approach, open surgeries are rarely done unless absolutely necessary. We prefer this approach because it creates less postoperative pain, faster recovery, fewer wound complications and improved cosmetic outcomes. Our experience with single-port robotic transumbilical surgery provided better ergonomics and precision during radical prostatectomy surgeries without complications.
Because the procedure uses only one point of access to the body, single-port surgery can leave minimal to no scarring that can commonly occur after traditional open and laparoscopic abdominal surgery procedures. Some patients are reporting less discomfort and faster recovery times compared with those undergoing traditional laparoscopy.
Distinctively, single port radical prostatectomy (SPRP) is a surgical procedure with potential benefits that are beyond just cosmetic.
About Iranian Surgery
Iranian surgery is an online medical tourism platform where you can find the best Surgeons in Iran. The price of Single Port Radical Prostatectomy in Iran can vary according to each individual’s case and will be determined by an in-person assessment with the doctor.
For more information about the cost of Single Port Radical Prostatectomy in Iran and to schedule an appointment in advance, you can contact Iranian Surgery consultants via WhatsApp number 0098 901 929 0946. This service is completely free.
Before Single Port Radical Prostatectomy
Why Would Someone Need a Single Port Radical Prostectomy?
Localized prostate cancer is the main reason doctors turn to this particular procedure. Your doctor can suggest a single port radical prostatecomy in combination with other therapies such as chemotherapy or radiation treatment.
Laproscopic single port radical prostectomy may be used to treat a blocked urethra caused by benign prostatic hyperplasia (noncancerous prostate enlargement). However, many times a radical prostatectomy doesn't need to be used for benign prostatic hyperplasia.
What Happens Before Single Port Radical Prostatectomy?
Before surgery, your doctor will perform a cystoscopy to visually inspect your bladder and urethra. This gives your doctor a better idea of what the condition your prostate and urinary system are in.
Your doctor will also instruct you on any modifications to your medications you need to make. If you are taking blood thinning medications or NSAID pain relievers (such as Advil or Motrin IB), you will be asked to stop taking those medications in order to decrease the risk of excess bleeding. Do not modify your medication schedule or routine without the doctors’ instructions.
Just like many other forms of surgery, your doctor will ask you to not eat or drink anything starting at midnight before the surgery. Medications that need to be taken before the surgery should be taken with a small sip of water.
If you have housework or other strenuous activities that need done after surgery, make plans to do them in advance or to have a friend or family member help you. Recovery time with a single port radical prostatectomy is less than in an open procedure, however it is important to allow yourself recovery time.
Am I a good candidate for a radical prostatectomy?
Other treatment options may be better for you if:
. Your health is poor and you’re unable to undergo anesthesia or surgery
. Your cancer is growing slowly
. Your cancer has spread beyond your prostate gland
Radical prostatectomy risks
In addition to the risks associated with any surgery, risks with radical prostatectomy include:
. Bleeding
. Urinary tract infection
. Urinary incontinence
. Erectile dysfunction (impotence)
. Narrowing of the urethra or bladder neck
. Formation of cysts containing lymph (lymphocele)
Advantages and disadvantages of Radical prostatectomy
What may be important for one person might be less important for someone else. The advantages and disadvantages of surgery may depend on your age, general health and the stage of your cancer.
Pros:
. If the cancer is completely contained inside the prostate, surgery will remove all of the cancer.
. The prostate is looked at under a microscope to give a clearer picture of how aggressive your cancer is, whether it has spread outside your prostate and if you need further treatment.
. Your health professionals can get a good idea of whether your cancer was completely removed during surgery. Your PSA level should drop so low that it’s not possible to detect it (less than 0.1 ng/ml) at six to eight weeks after surgery.
. If there are signs that your cancer has come back or wasn’t all removed, you may be able to have further treatment.
. Some men find it reassuring to know that their prostate has been physically removed, although you will still need to have follow-up tests to make sure no cancer cells have spread outside the prostate.
Cons:
There are risks in having surgery, as with any major operation.
. You might get side effects such as erection problems and urinary problems.
. If the cancer has started to spread outside the prostate, the surgeon may not be able to remove all of the cancer and you might need further treatment.
During Single Port Radical Prostatectomy
What Happens During Single Port Radical Prostatectomy?
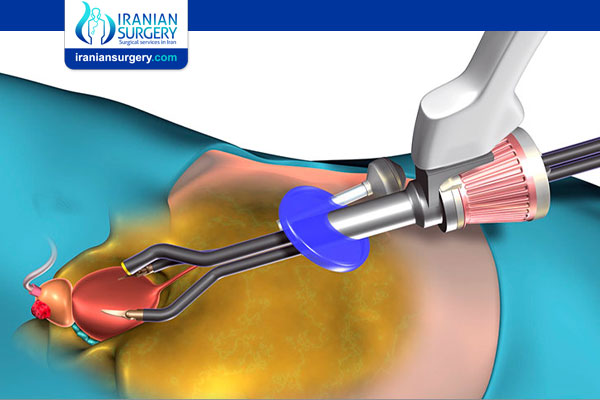
During a single port radical prostectomy you will be administered general anesthesia. Your surgeon will operate a state of the art robotic control console near you that allows him or her to manipulate the Da Vinci surgical robot. This robotic approach allows your surgeon to have precise control over the surgery and helps better visualize the prostate with a magnified view of the surgical area.
Using this advanced robotic technology, the surgeon will proceed to make incisions and remove your prostate gland through the port in your abdomen near your belly button.
After Single Port Radical Prostatectomy
Post-operative Care
If you have had a robotic prostatectomy, it is essential for your own safety and for the success of your surgery that you carefully read and follow these instructions.
Post-Operative Instructions:
While robotic prostatectomy is performed routinely, it is still a relatively major surgery that will take some time and effort to recover from. Life will be harder for at least a few weeks, if not months after surgery; however it is certainly preferable to the life-threatening hardships of letting the cancer progress unchecked. So stay positive, you can get through this.
Leaving the Hospital
. Patients can generally be discharged from the hospital about 24 hours after surgery.
. All patients will be discharged from the hospital with a urinary catheter in place. This catheter is known as a Foley catheter and is held in place by a balloon inside the bladder. It allows continuous drainage of the bladder into a small external collection bag which is emptied as needed. Absolutely, do not try to remove this catheter on your own. It must stay in place until you heal enough that it is no longer needed.
. Since you will not be cleared to drive yourself, you will need someone to drive you home.
When you get Home
. Activity
. Please refrain from driving for 1 week after your surgery. After one week, you can resume driving and most activities. Refrain from vigorous activity (running, golf, exercising, horseback riding, motorcycles, bicycling however, for six weeks after surgery to give yourself time to heal. After six weeks you may resume full activities using common sense.
. Avoid climbing stairs as a form of exercise.
. Avoid sitting still in one position for too long (more than 45 minutes)
. Avoid bathtubs, swimming pools, hot tubs or otherwise submerging yourself in water for as long as the catheter is in place. Showering is fine as soon as you go home.
. When you may return to work depends on your occupation and how fast you recover. Most jobs you may return to in 1-3 weeks. Use common sense.
. Medication
. Most of our patients experience only minimal discomfort, and we recommend that you try ibuprofen or Tylenol (acetaminophen) for pain first, as they usually suffice. Stronger, prescription pain killers tend to be extremely constipating and so it is better to avoid them if possible. However, if you still have significant pain despite Motrin or Tylenol, contact your physician for a prescription for stronger pain medication, which will typically be hydrocodone or codeine.
. Upon discharge from the hospital, you will also be prescribed an oral antibiotic, which will most likely be Cipro. You will not take these until the morning you are scheduled to have your catheter removed. On that morning, take one pill. Then take one pill each 12 hours after that. This is twice a day for 3 days, for a total of six pills. For example, if you are going to have your catheter removed on Thursday, take your first antibiotic pill on Thursday morning, then every 12 hours after that, ending on Saturday night.
. You may resume any of the usual daily medications you may have been taking before surgery for other medical conditions, as soon as you are discharged.
. At the time of discharge, you will be given a stool softener to be used for constipation. We recommend that in addition to the stool softener you also drink prune juice or milk of magnesia until you have your first bowel movement after surgery. You many continue taking the stool softener as needed to combat constipation.
. You may also be provided with a small amount of Ditropan (oxybutinin) to be used in the event you develop bladder spasms while the catheter is still inserted. Bladder spasms are typically associated with a sudden onset of lower-abdominal discomfort, a strong urge to urinate, or with sudden leakage of urine from around the catheter.
. Food
. To make it easier on you immediately out of the hospital, you may initially want to stick to a bland diet. Some patients prefer a mostly liquid diet. Avoid carbonated beverages.
. Once you have had a bowel movement, you should move to a soft food diet of things like soups, scrambled eggs, toast, oatmeal etc... And then work your way back to your normal diet as you feel comfortable.
. Avoid gas-producing foods such as flour, beans, and broccoli.
. Try to spread out eating throughout the day with snacks and small meals, to avoid eating large meals at once for a few days after surgery.
. Clothing
. Immediately after surgery, your abdomen will be slightly bloated so you may have trouble fitting into your regular clothes. For comfort, wear lose fitting clothing such as sweatpants or other pants with elastic (not button) waist bands. You will probably need to do so initially anyway to accommodate the catheter and collection bag.
. Wound Care
. You may now start showering the day of your discharge. The catheter collection bag may be removed during showering. Gently pull the colored catheter straight off of the clear plastic tubing from the bag and allow urine to run into the shower. After showering, gently pad the suture sites (do not rub or otherwise irritate them) with a towel.
. Application of ointments (such as Neosporin) to incision sites is not recommended.
. Sutures were utilized which will dissolve on their own, there is no need to have them removed. A small amount of redness at the edges of the incision sites, as well as a small amount of clear or bloody leakage from the wound, is acceptable. Drainage of sufficient quantity to soak dressings, or redness greater than 1/2 inch from the incision should be reported to the physician.
. Catheter Care
. As mentioned above, you will be discharged from the hospital with a Foley catheter in place which continuously drains urine from your bladder. It must stay in place while your anastamosis heals. Do not attempt to remove this on your own. If it should accidentally fall out, you must immediately notify your Urologist to have it replaced. Do NOT allow a non-urologist (even if they are a nurse or a doctor) to replace it. The catheter was carefully placed by your urologist with specific regard to your prostatectomy and cannot be replaced by just anyone.
. You will be given antibiotic ointment to lubricate the outside catheter where it enters the tip of your penis (the uretheral meatus.) This ointment will reduce inflammation to the uretheral meatus and reduce discomfort. Apply the ointment as needed.
. You will provided with a "stat-lock," a plastic clip which will be glued to your thigh to hold the catheter. This will be removed when your catheter is removed 1 week after surgery.
. You will be provided with two urine collection bags of different sizes, a smaller bag to be worn under your pants during the day, and a larger bag to be used at night. The smaller bag usually lasts about 3-4 hours before needing to be emptied, but of course this varies with how much liquid you consume. The larger bag should last you all night, so you do not need to wake up to empty it. Remove, empty, and exchange these two bags as needed.
. Alert the surgeon if the catheter does not drain well, or if you have any other serious problems with it.
. This catheter will stay in place for one week while you heal, and can generally be removed by your urologist at the end of this time. Sometimes it may have to stay in place longer if you are not sufficiently healed, perhaps two weeks instead of one. You should have already scheduled a follow-up appointment for this purpose. Remember from above, that you will start taking your oral antibiotic (probably Cipro) on the morning of this day.
. Regaining Urinary Control
. Most men have difficulty with urinary control after catheter removal. You should bring an adult urinary pad (such as Depend Guards) with you the day your catheter is removed. You should be prepared to wear these pads for a while because normal urinary control may not be regained for 2 months from the time of your surgery. Remember, everyone is different. Some men regain control in a week, some take six months. Don't be discouraged! Also, remember you will typically leak more standing, moving, and straining, and less when lying down and sleeping.
. Remember to do your kegel exercises regularly. The operation removed your prostate and affected your secondary urinary control mechanisms. Your external sphincter muscle must now take over all responsibility for control. It will take time and effort to strengthen this mechanism.
. Some men may continue to have mild incontinence with straining even several years after surgery. You can avoid a problem in these situations by wearing a small pad. Rarely, urinary control will be unsatisfactory even after a year. If so, something can still be done. Though rarely needed, there are techniques for restoring control such as placement of an artificial urinary sphincter.
. Regaining Sexual Function
. The operation will affect sexual function in several ways, but it should not prevent you from having a fulfilling sex life when you recover. There are three components to sexual function in men: sexual drive, sensation, erection and climax (orgasm). Although these normally occur together, they actually are separate functions. Losing one does not necessarily mean you will lose the others.
. Erections occur due to a complex sequence of events involving stimulation of the cavernosal nerves and engorgement of the penis with blood. The cavernosal nerves run alongside the prostate, only millimeters away from where cancer often occurs. Prostate cancer also tends to spread along these nerves. For these reasons, although it may have been technically possible to spare the nerves, it may not have been done.
. Since the primary goal of the surgery was to rid you of cancer, one or both of these nerves may have been resected. There is a chance of recovering erections, but recovery may be slow. Nerves can heal, but very slowly. The average time to recovery for erections adequate for sexual intercourse is 6-18 months, but in some men can be even longer. While you are waiting for erections to return, a number of approaches are available for achieving erections. Ask about these in our office. If these methods are unsuccessful, a prosthesis can be placed to restore sexual function.
. Climax will not be affected by the surgery, but ejaculation (the release of fluid during orgasm) will no longer occur. You will still have the same sensations of pleasure, but no fluid will be discharged and you will have a dry ejaculation. This is because the seminal vesicles, which store fluid for ejaculation, and the vas deferens, the tubes that carry sperm to the prostate, are removed and cut during the operation. This means that you will be infertile and no longer able to father children.
If you have any questions about these instructions please contact your physician. You should have received similar instructions on paper upon discharge from the hospital. These instructions are given in your best interest and should be followed as carefully and closely as possible.
Sources:
. https://my.clevelandclinic.org/health/treatments/17475-single-port-radical-prostatectomy
. https://urology.uci.edu/prostate/postop.html