Prostatitis
Prostatitis
What is Prostatitis?
Prostatitis refers to four different conditions that affect the prostate gland. Two types of prostatitis are linked to urinary tract infections (UTIs). Other types are not. Men with prostatitis may have infection, inflammation and/or pain. Adult men of any age can get prostatitis.
Many men who are told they have prostatitis are misdiagnosed and actually have a different condition. There’s a lot of outdated information about prostatitis. It’s important to see a healthcare provider who is up to date on the latest prostatitis research, diagnostic tests and treatments.
Before Prostatitis Treatment
What is the prostate gland?
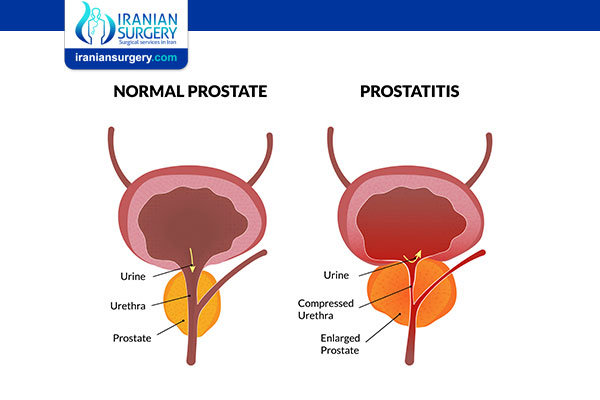
The prostate gland is part of the male reproductive system. It sits below your bladder, in front of the rectum. The urethra (tube that carries urine and semen out of the body) runs through the center of the gland.
How common is prostatitis?
Half of all men have symptoms of prostatitis at some point in their lives. It’s the most common urinary tract issue in men younger than 50. In men over 50, it’s the third most common. More than two million men see a healthcare provider every year for prostatitis symptoms.
What are the types of prostatitis?
Types of prostatitis include:
. Acute bacterial prostatitis (category 1): A UTI causes an infection in the prostate gland. Symptoms include fever and chills. You may experience painful and frequent urination or have trouble urinating. Acute bacterial prostatitis requires immediate medical treatment.
. Chronic bacterial prostatitis (category 2): Bacteria become trapped in the prostate gland, causing recurrent UTIs that are difficult to treat.
. Chronic pelvic pain syndrome, or CPPS (category 3): CPPS is the most common prostatitis type. Prostate gland inflammation occurs in approximately 1 out of 3 men. As the name implies, this type causes chronic pain in the pelvis, perineum (the area between the scrotum and rectum) and genitals.
. Asymptomatic inflammatory prostatitis (category 4): This condition causes prostate gland inflammation but no symptoms. You may learn you have this condition after getting tests to find the cause of other problems. For example, a semen analysis for infertility may detect asymptomatic inflammatory prostatitis. This type doesn’t need treatment.
Is prostatitis a sign of prostate cancer?
Prostatitis is benign (not cancerous). It doesn’t increase your risk of prostate cancer. However, inflammation from prostatitis sometimes raises the level of prostate-specific antigens (PSA) in blood — just like prostate cancer does. Further tests can help determine what’s causing elevated PSA levels.
What are the complications of prostatitis?
Men with acute bacterial prostatitis may develop sepsis. This widespread inflammation can be life-threatening. It requires immediate medical treatment.
Antibiotics can cause an upset stomach. Men with chronic bacterial prostatitis may need lots of antibiotics to treat recurring infections. Some people develop antibiotic resistance, making treatment ineffective.
Asymptomatic inflammatory prostatitis can lower sperm count, affecting fertility.
What causes prostatitis?
Different types of prostatitis have different causes. Risk factors for chronic pelvic pain syndrome (CPPS), the most common type, aren’t clear. Potential contributors to CPPS include:
. Autoimmune diseases.
. Pelvic floor muscle spasms.
. Stress.
Potential causes of bacterial forms of prostatitis include:
. Bladder infections or bladder stones.
. Surgery or biopsy requiring use of a urinary catheter.
. Prostate stones.
. Urinary retention (not emptying the bladder completely).
. UTIs.
What are the symptoms of prostatitis?
Prostatitis symptoms vary depending on the type and cause. People with asymptomatic inflammatory prostatitis don’t have any symptoms.
Men with chronic pelvic pain syndrome or chronic bacterial prostatitis may experience:
. Pain in the penis, testicles or perineum (area between the testicles and rectum). The pain may radiate to the lower back.
. Frequent urge to urinate.
. Painful urination (dysuria).
. Weak urine flow or urine stream that starts and stops.
. Painful ejaculation or pain during intercourse.
. Blood in semen (hematospermia).
. Erectile dysfunction.
Acute bacterial prostatitis causes a fever and chills.
Diagnosis and Tests
How is prostatitis diagnosed?
Your healthcare provider will assess your symptoms and perform a physical exam.
Less invasive tests for prostatitis may include:
. Digital rectal exam: Your provider inserts a gloved, lubricated finger into the rectum to check the prostate gland for pain and swelling. This exam may include prostate massage to collect a sample of seminal fluid.
. Urinalysis: A urinalysis and urine culture check for bacteria and UTIs.
. Blood test: A blood test measures PSA, a protein made by the prostate gland. High levels may indicate prostatitis, BPH or prostate cancer.
More invasive tests for prostatitis include:
. Cystoscopy: A cystoscopy can look for other urinary tract problems but does not diagnose prostatitis. Your provider uses a cystoscope (a pencil-sized lighted tube with a camera or viewing lens on the end) to view inside the bladder and urethra.
. Transrectal ultrasound: Men with acute bacterial prostatitis or chronic bacterial prostatitis that doesn’t improve with antibiotics may get a transrectal ultrasound. A slender ultrasound probe inserted into the rectum uses sound waves to produce images of the prostate gland. This test can show prostate gland abnormalities, abscesses or stones.
Prevention
How can I prevent prostatitis?
Prompt treatment for UTIs may keep the infection from spreading to the prostate. If you have pain in your perineum when sitting, see a provider. You can take steps to address this problem before it leads to chronic pelvic pain syndrome.
During Prostatitis Treatment
Management and Treatment
How is chronic pelvic pain syndrome (CPPS) managed or treated?
Prostatitis treatments vary depending on the cause and type. Asymptomatic inflammatory prostatitis doesn’t require treatment.
For chronic pelvic pain syndrome (CPPS), your healthcare provider may use a system called UPOINT to classify symptoms into six categories. Your provider uses multiple treatments at the same time to treat only the symptoms you’re experiencing.
Approximately 80% of men with CPPS improve with the UPOINT system. The system focuses on these symptoms and treatments:
. Urinary: Medications, such as tamsulosin (Flomax®) and alfuzosin (Uroxatral®), relax muscles around the prostate and bladder to improve urine flow.
. Psychosocial: Stress management can help. Some men benefit from counseling or medications for anxiety, depression and catastrophizing (over-reaction to minor stresses common in people with chronic pain).
. Organ: Quercetin and bee pollen supplements may relieve a swollen, inflamed prostate gland.
. Infection: Antibiotics kill infection-causing bacteria.
. Neurologic: Prescription pain medicines, such as amitriptyline (Elavil®) and gabapentin (Gralise®), relieve neurogenic pain. This pain can include fibromyalgia or pain that extends into the legs, arms or back.
. Tenderness: Pelvic floor physical therapy may include myofascial release (gentle massage to ease tension on tight pelvic floor muscles). This therapy can reduce or eliminate muscle spasms.
How are bacterial forms of prostatitis managed or treated?
Antibiotics can kill bacteria that cause bacterial types of prostatitis. Men with acute bacterial prostatitis may need 14 to 30 days of antibiotics, starting with IV antibiotics in the hospital. Rarely, men need surgery to drain an abscess on the prostate.
Treating chronic bacterial prostatitis is challenging. You may need up to three months of antibiotics to sterilize the prostate. If the prostate can’t be sterilized, low-dose antibiotics can be used long term to prevent recurrences. Some men need surgery to remove prostate stones or scar tissue in the urethra. Rarely, surgeons remove part or all of the prostate gland (prostatectomy).
After Prostatitis Treatment
Outlook / Prognosis
What is the prognosis (outlook) for people who have prostatitis?
Antibiotics can cure acute bacterial prostatitis. These medications also ease chronic bacterial prostatitis symptoms in approximately 30% to 60% of men. Up to 80% of men with chronic pelvic pain syndrome feel better after receiving appropriate treatments for their symptoms using the UPOINT system. Men with asymptomatic inflammatory prostatitis don’t need treatment.
When should I call the doctor?
You should call your healthcare provider if you experience:
. Blood in your urine or semen.
. Difficulty urinating.
. Frequent urination (incontinence).
. Pain during urination or intercourse.
Source:
. https://my.clevelandclinic.org/health/diseases/15319-prostatitis