Placenta Accreta
Placenta Accreta
What is Placenta Accreta?
Placenta accreta is a condition in which the placenta (the food source for a baby in the uterus) grows too deeply into the wall of the uterus. In a typical pregnancy, the placenta easily detaches from the wall of the uterus following delivery. In placenta accreta, the placenta has grown into the uterine wall and does not separate easily following delivery. In severe cases, this condition can lead to excessive bleeding, which can be life-threatening. It can require a blood transfusion and even hysterectomy (removal of the uterus).
Before Placenta Accreta Treatment
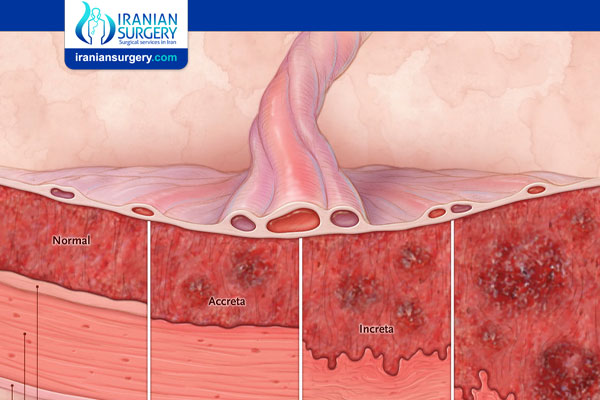
What are the different types of placenta accreta?
There are three types of this condition. The type is determined by how deeply the placenta is attached to the uterus.
. Placenta accreta: The placenta firmly attaches to the wall of the uterus. It does not pass through the wall of the uterus or impact the muscles of the uterus. This is the most common type of the condition.
. Placenta increta: This type of the condition sees the placenta more deeply imbedded in the wall of the uterus. It still does not pass through the wall, but is firmly attached to the muscle of the uterus.
. Placenta percreta: The most severe of the types, placenta percreta happens when the placenta passes through the wall of the uterus. The placenta might grow through the uterus and impact other organs, such as the bladder or intestines.
What are the risks to the mother and baby from placenta accreta?
The risks of placenta accreta can be serious and can expand beyond the mother to the newborn. Once born, the baby may be at additional risk because of a premature birth. Risks for the mother can include:
. Premature delivery
. Damage to the uterus and surrounding organs
. Loss of fertility due to the need for a hysterectomy (removal of uterus)
. Excessive bleeding that requires a blood transfusion
. Death
What leads to placenta accreta?
Placenta accreta is thought to be caused by scarring or other abnormalities with the lining of the uterus. Several risk factors have been linked to placenta accreta, including:
. Multiple cesarean sections (c sections): Women who have had multiple cesarean sections have a higher risk of developing placenta accreta. This results from scarring of the uterus from the procedures. The more cesarean sections a woman has over time, the higher her risk of placenta accreta.
. Placenta previa: This condition occurs when the placenta is located at the bottom of the uterus, blocking the opening of the cervix. The lower part of the uterus is less suited for the placenta to implant. In patients with placenta previa and a history of prior cesarean section(s), the risk for placenta accreta increases with the number of cesarean sections the patient has had.
. History of fibroid removal: If the woman has had a fibroid (a not cancerous growth or tumor of the uterine muscle) removed, the scarring could lead to placenta accreta.
Diagnosis and Tests
How is placenta accreta diagnosed?
Placenta accreta is typically diagnosed prior to delivery with an ultrasound. Magnetic resonance imaging (MRI) can be useful in some cases. Patients who have risk factors for placenta accreta should be carefully evaluated by either or both of these tests.
How important is an early diagnosis of placenta accreta?
An early diagnosis of placenta accreta is very important because it can allow for multiple caregivers to become involved in the pregnancy. Depending on the type and severity of the condition, a team of doctors may need to be involved in the mother’s care. Having the right people involved could prevent the removal of the uterus (hysterectomy) or life-threatening blood loss. In severe cases, hysterectomy and blood transfusion may not be able to be avoided despite early diagnosis and having the appropriate team present; however, risks for other complications are lowered. Continuous monitoring of the pregnancy will be needed after a diagnosis of placenta accreta to ensure the best results for mother and child.
Prevention
Can placenta accreta be prevented?
Placenta accreta cannot be prevented. The risk of placenta accreta goes up if the mother has had multiple cesarean sections in the past and/or has a placenta previa. If you have had previous cesarean sections and have a placenta previa, talk to your doctor about the risks of placenta accreta.
During Placenta Accreta Treatment
Management and Treatment
How is placenta accreta treated?
Treatment of placenta accreta can vary. If the condition is diagnosed before birth, the pregnancy will be monitored closely. The caregiver will schedule a cesarean section (C-section) to deliver the baby, often several weeks before the due date. This is done to decrease the risk of bleeding from contractions or labor. If the woman wishes to have future pregnancies, the caregivers may attempt to save the uterus. However, in severe cases where the placenta is noted to be extremely adherent or invading into other organs, a hysterectomy (removal of the uterus) may be the safest option for the mother. Removing the uterus with the placenta still attached minimizes the risk of excessive bleeding (hemorrhaging).
After Placenta Accreta Treatment
Outlook / Prognosis
What is the outlook for women with placenta accreta?
If the uterus has been removed in a hysterectomy, no future pregnancies will occur. In severe cases, this condition can lead to massive blood loss, injury to the bowel or bladder, and even maternal death.
Source:
. https://my.clevelandclinic.org/health/diseases/17846-placenta-accreta