Periodontal disease
Periodontal disease, also known as gum disease, is a set of inflammatory conditions affecting the tissues surrounding the teeth. In its early stage, called gingivitis, the gums become swollen, red, and may bleed. In its more serious form, called periodontitis, the gums can pull away from the tooth, bone can be lost, and the teeth may loosen or fall out. Bad breath may also occur.
Periodontal disease is generally due to bacteria in the mouth infecting the tissue around the teeth. Risk factors include smoking, diabetes, HIV/AIDS, family history, and certain medications. Diagnosis is by inspecting the gum tissue around the teeth both visually and with a probe and X-rays looking for bone loss around the teeth.
Treatment involves good oral hygiene and regular professional teeth cleaning. Recommended oral hygiene include daily brushing and flossing. In certain cases antibiotics or dental surgery may be recommended. Globally 538 million people were estimated to be affected in 2015. In the United States nearly half of those over the age of 30 are affected to some degree, and about 70% of those over 65 have the condition. Males are affected more often than females.
Signs and symptoms

1: Total loss of attachment (clinical attachment loss, CAL) is the sum of 2: Gingival recession, and 3: Probing depth
In the early stages, periodontitis has very few symptoms, and in many individuals the disease has progressed significantly before they seek treatment.
Symptoms may include:
- Redness or bleeding of gums while brushing teeth, using dental floss or biting into hard food (e.g., apples) (though this may occur even in gingivitis, where there is no attachment loss)
- Gum swelling that recurs
- Spitting out blood after brushing teeth
- Halitosis, or bad breath, and a persistent metallic taste in the mouth
- Gingival recession, resulting in apparent lengthening of teeth. (This may also be caused by heavy-handed brushing or with a stiff toothbrush.)
- Deep pockets between the teeth and the gums (pockets are sites where the attachment has been gradually destroyed by collagen-destroying enzymes, known as collagenases)
- Loose teeth, in the later stages (though this may occur for other reasons, as well)
People should realize gingival inflammation and bone destruction are largely painless. Hence, people may wrongly assume painless bleeding after teeth cleaning is insignificant, although this may be a symptom of progressing periodontitis in that person.
Associated conditions
Periodontitis has been linked to increased inflammation in the body, such as indicated by raised levels of C-reactive protein and interleukin-6. It is associated with an increased risk of stroke,]myocardial infarction, atherosclerosis and hypertension. It also linked in those over 60 years of age to impairments in delayed memory and calculation abilities. Individuals with impaired fasting glucose and diabetes mellitus have higher degrees of periodontal inflammation, and often have difficulties with balancing their blood glucose level owing to the constant systemic inflammatory state, caused by the periodontal inflammation. Although no causal association was proven, there is an association between chronic periodontitis and erectile dysfunction, and heart disease.
Causes
Periodontitis is an inflammation of the periodontium, i.e., the tissues that support the teeth. The periodontium consists of four tissues:
- gingiva, or gum tissue,
- cementum, or outer layer of the roots of teeth,
- alveolar bone, or the bony sockets into which the teeth are anchored, and
- periodontal ligaments (PDLs), which are the connective tissue fibers that run between the cementum and the alveolar bone.
This X-ray film displays two lone-standing mandibular teeth, the lower left first premolar and canine, exhibiting severe bone loss of 30–50%. Widening of the periodontal ligament surrounding the premolar is due to secondary occlusal trauma.
The primary cause of gingivitis is poor or ineffective oral hygiene, which leads to the accumulation of a mycotic and bacterial matrix at the gum line, called dental plaque. Other contributors are poor nutrition and underlying medical issues such as diabetes. Diabetics must be meticulous with their homecare to control periodontal disease. New finger prick tests have been approved by the Food and Drug Administration in the US, and are being used in dental offices to identify and screen people for possible contributory causes of gum disease, such as diabetes.
In some people, gingivitis progresses to periodontitis – with the destruction of the gingival fibers, the gum tissues separate from the tooth and deepened sulcus, called a periodontal pocket. Subgingival microorganisms (those that exist under the gum line) colonize the periodontal pockets and cause further inflammation in the gum tissues and progressive bone loss. Examples of secondary causes are those things that, by definition, cause microbic plaque accumulation, such as restoration overhangs and root proximity.

The excess restorative material that exceeds the natural contours of restored teeth, such as these, are termed "overhangs", and serve to trap microbic plaque, potentially leading to localized periodontitis.
Smoking is another factor that increases the occurrence of periodontitis, directly or indirectly, and may interfere with or adversely affect its treatment. It is arguably the most important environmental risk factor for periodontitis. Research has shown that smokers have more bone loss, attachment loss and tooth loss compared to non-smokers. The reason for this is that smoking has several effects on the immune response including:
- Decreased wound healing
- Suppresses antibody production
- It reduces neutrophilic phagocytosis
Ehlers–Danlos syndrome is a periodontitis risk factor and so is the Papillon–Lefèvre syndrome also known as palmoplantar keratoderma.
If left undisturbed, microbial plaque calcifies to form calculus, which is commonly called tartar. Calculus above and below the gum line must be removed completely by the dental hygienist or dentist to treat gingivitis and periodontitis. Although the primary cause of both gingivitis and periodontitis is the microbial plaque that adheres to the tooth surfaces, there are many other modifying factors. A very strong risk factor is one's genetic susceptibility. Several conditions and diseases, including Down syndrome, diabetes, and other diseases that affect one's resistance to infection, also increase susceptibility to periodontitis.
Another factor that makes periodontitis a difficult disease to study is that human host response can also affect the alveolar bone resorption. Host response to the bacterial-mycotic insult is mainly determined by genetics; however, immune development may play some role in susceptibility.
According to some researchers periodontitis may be associated with higher stress. Periodontitis occurs more often in people from the lower end of the socioeconomic scale than people from the upper end of the socioeconomic scale.
Genetics appear to play a role in determining the risk for periodontitis. It is believed genetics could explain why somepeople with good plaque control have advanced periodontitis, whilst some others with poor oral hygiene are free from the disease. Genetic factors which could modify the risk of a person developing periodontitis include:
- Defects of Phagocytosis: person may have hypo-responsive phagocytes.
- Hyper-production of interleukins, prostaglandins and cytokines. This results in a massively exaggerated immune response.
- Interleukin 1 (IL-1) gene polymorphism: people with this polymorphism produce more IL-1, and subsequently are more at risk of developing chronic periodontitis.
Diabetes appears to exacerbates the onset, progression, and severity of periodontitis. Although the majority of research has focused on type 2 diabetes, type 1 diabetes appears to have an identical effect on the risk for periodontitis. The extent of the increased risk of periodontitis is dependent on the level of glycaemic control. Therefore, in well managed diabetes there seems to be a small effect of diabetes on the risk for periodontitis. However, the risk increases exponentially as glycaemic control worsens. Overall, the increased risk of periodontitis in diabetics is estimated to be between 2-3 times higher. So far, the mechanisms underlying the link are not fully understood, but it’s known to involve aspects of inflammation, immune functioning, neutrophil activity, and cytokine biology.
Mechanism
As dental plaque or biofilm accumulates on the teeth near and below the gums that is some dysbiosis of the normal oral microbiome.As of 2017 it was not certain what species were most responsible for causing harm, but gram-negative anaerobic bacteria, spirochetes, and viruses have been suggested; in individual people it is sometimes clear that one or more species is driving disease. Research in 2004 indicated three species gram negative anerobic species: Actinobacillus actinomycetemcomitans, Porphyromonas gingivalis, Bacteroides forsythus and Eikenella corrodens.
Plaque may be soft and uncalcified, hard and calcified, or both; for plaques that are on teeth the calcium comes from saliva; for plaques below the gumline, it comes from blood via oozing of inflamed gums.
The damage to teeth and gums comes from the immune system as it attempts to destroy the microbes that are disrupting the normal symbiosis between the oral tissues and the oral microbe community. As in other tissues, Langerhans cells in the epithelium take up antigens from the microbes, and present them to the immune system, leading to movement of white blood cells into the affected tissues. This process in turn activates osteoclasts which begin to destroy bone, and it activates matrix metalloproteinases that destroy ligaments. So, in summary, it is bacteria which initiates the disease, but key destructive events are brought about by the exaggerated response from the host's immune system.
Classification
There were several attempts to introduce an agreed-upon classification system for periodontal diseases: in 1989, 1993, 1999, and 2017.
1999 classification
The 1999 classification system for periodontal diseases and conditions listed seven major categories of periodontal diseases, of which 2–6 are termed destructive periodontal disease, because the damage is essentially irreversible. The seven categories are as follows:
- Gingivitis
- Chronic periodontitis
- Aggressive periodontitis
- Periodontitis as a manifestation of systemic disease
- Necrotizing ulcerative gingivitis/periodontitis
- Abscesses of the periodontium
- Combined periodontic-endodontic lesions
Moreover, terminology expressing both the extent and severity of periodontal diseases are appended to the terms above to denote the specific diagnosis of a particular person or group of people.
Severity
The "severity" of disease refers to the amount of periodontal ligament fibers that have been lost, termed "clinical attachment loss". According to the 1999 classification, the severity of chronic periodontitis is graded as follows:
- Slight: 1–2 mm (0.039–0.079 in) of attachment loss
- Moderate: 3–4 mm (0.12–0.16 in) of attachment loss
- Severe: ≥ 5 mm (0.20 in) of attachment loss
Extent
mesiobuccalThe "extent" of disease refers to the proportion of the dentition affected by the disease in terms of percentage of sites. Sites are defined as the positions at which probing measurements are taken around each tooth and, generally, six probing sites around each tooth are recorded, as follows:
- mid-buccal
- distobucca
- mesiolingual
- mid-lingual
- distolingual
If up to 30% of sites in the mouth are affected, the manifestation is classified as "localized"; for more than 30%, the term "generalized" is used.
2017 classification
The 2017 classification of periodontal diseases is as follows:
Periodontal health, gingival disease and conditions
- Periodontal health and gingival health. There are two types: a. Clinical gingival health on an intact periodontiutm b. Clinical gingival health on a reduced periodontium i.Stable periodontitis ii.Non periodontitis person
- Gingivitis: Dental biofilm induced. There are 3 types: Associated with the dental biofilm alone, mediated by systemic and local risk factors, or drug induced gingival enlargement.
- Gingival diseases: Non dental biofilm induced. There are six sub-types: Genetic/developmental disorders, Specific infections, Inflammatory and immune conditions, Reactive processes, Neoplasms, Endocrine, nutritional and metabolic, Traumatic lesions or Gingival pigmentation.
Periodontitis
- Necrotizing periodontal diseases
- Periodontitis
- Periodontitis as a manifestation of systemic disease
Other conditions affecting the periodontium
- Systemic disease of conditions affecting the periodontal support tissues
- Periodontal abscesses and endodontic periodontal lesions
- Mucogingival deformities and conditions
- Traumatic occlusal forces
- Tooth and prosthesis related factor
Peri-implant diseases and conditions
- Peri-implant health
- Peri-implant mucositis
- Peri-implantitis
- Peri-implant soft and hard tissue deficiencies
Staging
The goals of staging periodontitis is to classify the severity of damage and assess specific factors that may affect management.
According to the 2017 classification, periodontits is divided into four stages (1 to 4); after considering a few factors such as:
- Amount and percentage bone loss radiographically
- Clinical attachment loss, probing depth
- Presence of furcation
- Vertical bony defects
- History of tooth loss related to periodontitis
- Tooth hypermobility due to secondary occlusal trauma.
Grading
According to the 2017 classification, the grading system for periodontitis consists of three grades:
- Grade A: Slow progression of disease; no evidence of bone loss over last five years
- Grade B: Moderate progression; <2mm of bone loss over last five years
- Grade C: Rapid progression and/or future progression at high risk; >_ 2mm bone loss over five years
Risk factors affecting which grade a person is classified into include:
- Smoking
- Diabetes
Prevention
Daily oral hygiene measures to prevent periodontal disease include:
- Brushing properly on a regular basis (at least twice daily), with the person attempting to direct the toothbrush bristles underneath the gumline, helps disrupt the bacterial-mycotic growth and formation of subgingival plaque.
- Flossing daily and using interdental brushes (if the space between teeth is large enough), as well as cleaning behind the last tooth, the third molar, in each quarter
- Using an antiseptic mouthwash: Chlorhexidine gluconate-based mouthwash in combination with careful oral hygiene may cure gingivitis, although they cannot reverse any attachment loss due to periodontitis.
- Using periodontal trays to maintain dentist-prescribed medications at the source of the disease: The use of trays allows the medication to stay in place long enough to penetrate the biofilms where the microorganism are found.
- Regular dental check-ups and professional teeth cleaning as required: Dental check-ups serve to monitor the person's oral hygiene methods and levels of attachment around teeth, identify any early signs of periodontitis, and monitor response to treatment.
- Microscopic evaluation of biofilm may serve as a guide to regaining commensal health flora.
Typically, dental hygienists (or dentists) use special instruments to clean (debride) teeth below the gumline and disrupt any plaque growing below the gumline. This is a standard treatment to prevent any further progress of established periodontitis. Studies show that after such a professional cleaning (periodontal debridement), microbial plaque tends to grow back to precleaning levels after about three to four months. Nonetheless, the continued stabilization of a person's periodontal state depends largely, if not primarily, on the person's oral hygiene at home, as well as on the go. Without daily oral hygiene, periodontal disease will not be overcome, especially if the person has a history of extensive periodontal disease.
Management
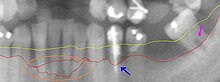
This section from a panoramic X-ray film depicts the teeth of the lower left quadrant, exhibiting generalized severe bone loss of 30–80%. The red line depicts the existing bone level, whereas the yellow line depicts where the gingiva was located originally (1–2 mm above the bone), prior to the person developing periodontal disease. The pink arrow, on the right, points to a furcation involvement, or the loss of enough bone to reveal the location at which the individual roots of a molar begin to branch from the single root trunk; this is a sign of advanced periodontal disease. The blue arrow, in the middle, shows up to 80% bone loss on tooth #21, and clinically, this tooth exhibited gross mobility. Finally, the peach oval, to the left, highlights the aggressive nature with which periodontal disease generally affects mandibular incisors. Because their roots are generally situated very close to each other, with minimal interproximal bone, and because of their location in the mouth, where plaque and calculus accumulation is greatest because of the pooling of saliva, mandibular anteriors suffer excessively. The split in the red line depicts varying densities of bone that contribute to a vague region of definitive bone height.
The cornerstone of successful periodontal treatment starts with establishing excellent oral hygiene. This includes twice-daily brushing with daily flossing. Also, the use of an interdental brush is helpful if space between the teeth allows. For smaller spaces, products such as narrow picks with soft rubber bristles provide excellent manual cleaning. Persons with dexterity problems, such as arthritis, may find oral hygiene to be difficult and may require more frequent professional care and/or the use of a powered toothbrush. Persons with periodontitis must realize it is a chronic inflammatory disease and a lifelong regimen of excellent hygiene and professional maintenance care with a dentist/hygienist or periodontist is required to maintain affected teeth.
Initial therapy
Removal of microbial plaque and calculus is necessary to establish periodontal health. The first step in the treatment of periodontitis involves nonsurgical cleaning below the gumline with a procedure called Root Surface Instrumentation or RSI, this causes a mechanical disturbance to the bacterial biofilm below the gumline. This procedure involves the use of specialized curettes to mechanically remove plaque and calculus from below the gumline, and may require multiple visits and local anesthesia to adequately complete. In addition to initial Root Surface Instrumentation, it may also be necessary to adjust the occlusion (bite) to prevent excessive force on teeth that have reduced bone support. Also, it may be necessary to complete any other dental needs, such as replacement of rough, plaque-retentive restorations, closure of open contacts between teeth, and any other requirements diagnosed at the initial evaluation. It is important to note that RSI is different to Scaling and Root planing: RSI only removes the calculus, whilst scaling and root planing removes the calculus as well as underlying softened dentine, which leaves behind a smooth and glassy surface, which is not a requiste for periodontal healing. Therefore RSI is now advocated over root planing.
Reevaluation
Nonsurgical scaling and root planing are usually successful if the periodontal pockets are shallower than 4–5 mm (0.16–0.20 in). The dentist or hygienist must perform a re-evaluation four to six weeks after the initial scaling and root planing, to determine if the person's oral hygiene has improved and inflammation has regressed. Probing should be avoided then, and an analysis by gingival index should determine the presence or absence of inflammation. The monthly reevaluation of periodontal therapy should involve periodontal charting as a better indication of the success of treatment, and to see if other courses of treatment can be identified. Pocket depths of greater than 5–6 mm (0.20–0.24 in) which remain after initial therapy, with bleeding upon probing, indicate continued active disease and will very likely lead to further bone loss over time. This is especially true in molar tooth sites where furcations (areas between the roots) have been exposed.
Surgery
If nonsurgical therapy is found to have been unsuccessful in managing signs of disease activity, periodontal surgery may be needed to stop progressive bone loss and regenerate lost bone where possible. Many surgical approaches are used in the treatment of advanced periodontitis, including open flap debridement and osseous surgery, as well as guided tissue regeneration and bone grafting. The goal of periodontal surgery is access for definitive calculus removal and surgical management of bony irregularities which have resulted from the disease process to reduce pockets as much as possible. Long-term studies have shown, in moderate to advanced periodontitis, surgically treated cases often have less further breakdown over time and, when coupled with a regular post-treatment maintenance regimen, are successful in nearly halting tooth loss in nearly 85% of diagnosed people.
10 common question about Periodontal disease
[kkstarratings]






2 Comments
My husband was diagnosed with early onset Parkinson’s disease at 68. His symptoms were shuffling of feet, slurred speech, low volume speech, degradation of hand writing, horrible driving skills, right arm held at 45 degree angle. Things were tough for me, I too was diagnosed of COPD but now we both finally free from these diseases with the help of total cure herbal foundation, He now walks properly and all symptoms has reversed. He had trouble with balance especially at night, getting into the shower and exiting it is difficult. Getting into bed is also another thing he finds impossible. We had to find a better solution for his condition which has really helped him a lot,The biggest helped we had was totalcureherbsfoundation .c om They walked us through the proper steps, im highly recommending this herbal formula to anyone who needs help.
Dear friend,we are deeply saddened by your problem.for the best remedy of parkinsom please check http://www.drvaziritabar.com for the best and certain solution.
thank you for your chice and your trust