Pancreatectomy in Iran
Pancreatectomy in Iran
Overview
A pancreatectomy is the surgical removal of all or part of the pancreas. The pancreas is an organ about the size of a hand located in the abdomen in the vicinity of the stomach, intestines, and other organs. It lies behind the stomach and in front of the spine. The pancreas has two critical functions in the body:
- The production juices that help digest food
- The production of hormones such as insulin and glucagon that maintain optimal blood sugar levels and help the body use and store energy from food
Conditions Treated
A pancreatectomy is used to treat a number of conditions involving the pancreas including:
- Acinar cell tumors
- Adenocarcinoma (85% of all cancers in pancrea)
- Cancer of the ampulla of Vater (ampullary cancer)
- Cancer of the distal (lower portion) of the bile duct.
- Cystadenocarcinoma
- Cystadenoma (mucinous/serous)
- Duodenal cancer
- Inflammation
- Islet cell tumors (neuroendocrine tumors)
- Lymphoma
- Necrotising pancreatitis
- Neoplasms
- Papillary cystic neoplasms
- Severe chronic pancreatitis
- Severe hyperinsulinemic hypoglycemia
- Severe Trauma
There are two types of pancreatectomy:
- Distal Pancreatectomy: The body and tail of the pancreas are removed. Often, the spleen is also removed. ...
- Total Pancreatectomy: Removal of the whole pancreas, part of the stomach and small intestine, common bile duct, gallbladder, spleen and lymph nodes.
Ready for surgery
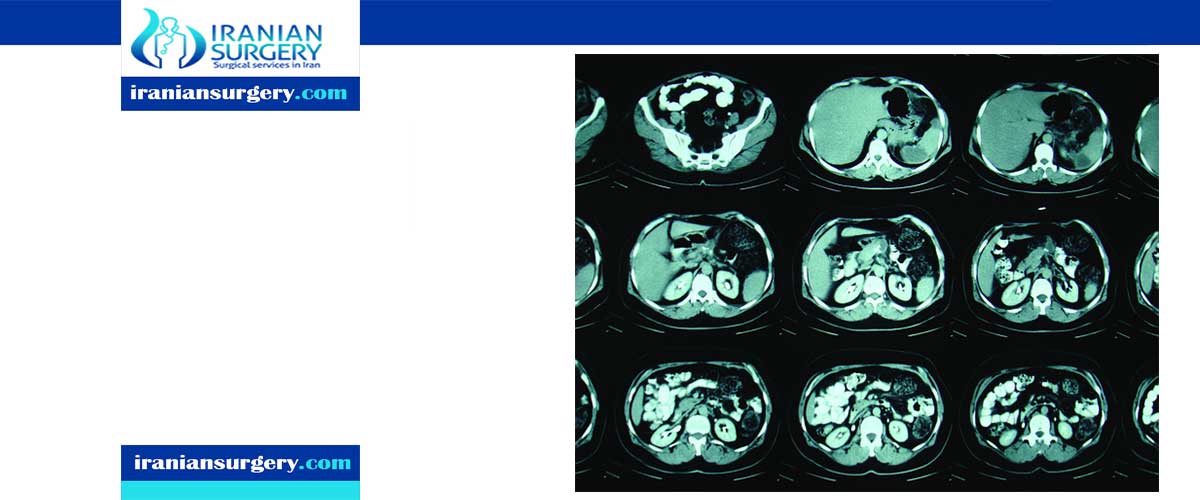
Patients with symptoms of a pancreatic disorder undergo a number of tests before surgery is even considered. These can include ultrasonography, x ray examinations, computed tomography scans (CT scan), and endoscopic retrograde cholangiopancreatography (ERCP), a specialized imaging technique to visualize the ducts that carry bile from the liver to the gallbladder. Tests may also include angiography, another imaging technique used to visualize the arteries feeding the pancreas, and needle aspiration cytology, in which cells are drawn from areas suspected to contain cancer. Such tests are required to establish a correct diagnosis for the pancreatic disorder and in the planning the surgery.
Since many patients with pancreatic cancer are undernourished, appropriate nutritional support, sometimes by tube feedings, may be required prior to surgery.
Some patients with pancreatic cancer deemed suitable for a pancreatectomy will also undergo chemotherapy and/or radiation therapy. This treatment is aimed at shrinking the tumor, which will improve the chances for successful surgical removal. Sometimes, patients who are not initially considered surgical candidates may respond so well to chemoradiation that surgical treatment becomes possible. Radiation therapy may also be applied during the surgery (intraoperatively) to improve the patient's chances of survival, but this treatment is not yet in routine use. Some studies have shown that intraoperative radiation therapy extends survival by several months.
Patients undergoing distal pancreatectomy that involves removal of the spleen may receive preoperative medication to decrease the risk of infection.
After surgery
Pancreatectomy is major surgery. Therefore, extended hospitalization is usually required with an average hospital stay of two to three weeks.
Some pancreatic cancer patients may also receive combined chemotherapy and radiation therapy after surgery. This additional treatment has been clearly shown to enhance survival rates.
After surgery, patients experience pain in the abdomen and are prescribed pain medication. Follow-up exams are required to monitor the patient's recovery and remove implanted tubes.
A total pancreatectomy leads to a condition called pancreatic insufficiency, because food can no longer be normally processed with the enzymes normally produced by the pancreas. Insulin secretion is likewise no longer possible. These conditions are treated with pancreatic enzyme replacement therapy, which supplies digestive enzymes; and with insulin injections. In some case, distal pancreatectomies may also lead to pancreatic insufficiency, depending on the patient's general health condition before surgery and on the extent of pancreatic tissue removal.
What are the risks of a pancreatectomy?
There are risks and side effects related to having a pancreatectomy. Risks and side effects may be:
- Pancreatic fistula (Leakage of pancreatic juice from the place that attaches the pancreas to the intestine).
- Gastroparesis/gastric ileus (Stomach paralysis).
- Delayed gastric emptying.
- Long term digestive complications such as bowel habit changes, malabsorption, need to change your diet, diabetes, infection and weight loss.
What is recovery like?
The hospital stay for a pancreatectomy is often one to three weeks. While in the hospital you may have:
- Abdominal drains to drain extra fluid.
- Nasogastric (NG) tube (tube placed into your nose and down into your stomach) to keep your stomach empty.
- Bladder catheter to empty urine from your bladder.
Depending on your situation, you may also have:
- Epidural tube to deliver pain medications.
- Feeding tube placed into your stomach to provide nutrition.
10 common questions about Pancreatectomy in Iran
[kkstarratings]


