Lymphadenectomy
Lymphadenectomy
Overview
A lymphadenectomy, also known as lymph node dissection, is a surgical procedure to remove one or more lymph nodes or groups of lymph nodes, which are then evaluated for the presence of cancer. It is important to know whether cancer has spread to the lymph nodes. After the lymph nodes are removed a sample of tissue is checked under a microscope for signs of cancer. For a regional lymphadenectomy, some of the lymph nodes in the tumor area are removed; for a radical lymphadenectomy, most or all of the lymph nodes in the tumor area are removed. Also called lymph node dissection.
With sentinel node biopsy
For clinical stages I and II breast cancer, axillary lymph node dissection should only be performed after first attempting sentinel node biopsy. Sentinel node biopsy can establish cancer staging of the axilla if there are positive lymph nodes present. It also is less risky than performing lymphadenectomy, having fewer side effects and a much lower chance of causing lymphedema. If cancer is not present in sentinel lymph nodes, then the axillary lymph node dissection should not be performed.
With sentinel lymph node mapping
The concept of sentinel lymph node mapping was popularized by Donald Morton and others. [citation needed] Cancer with various primary sites (breast, melanoma, colorectal, etc.) often metastasize early to the first drainage lymphatic basin. This process is predictable anatomically according to the primary site in the organ and the lymphatic channels. The first nodes (sentinel nodes) can be identified by particulate markers such as lymphazurin, methylene blue, India ink and radio-labelled colloid protein particles injected near the tumor site. The draining sentinel node can then be found by the surgeon and excised for verification by the pathologist if tumor cells are present, and often these tumor cells are few and only easily recognized by careful examination or by using techniques such as special stains, i.e. immunohistochemically. When the sentinel node is free of tumor cells, this is highly predictive of freedom from metastasis in the entire lymphatic basin, thus allowing a full node dissection to be avoided.
purpose
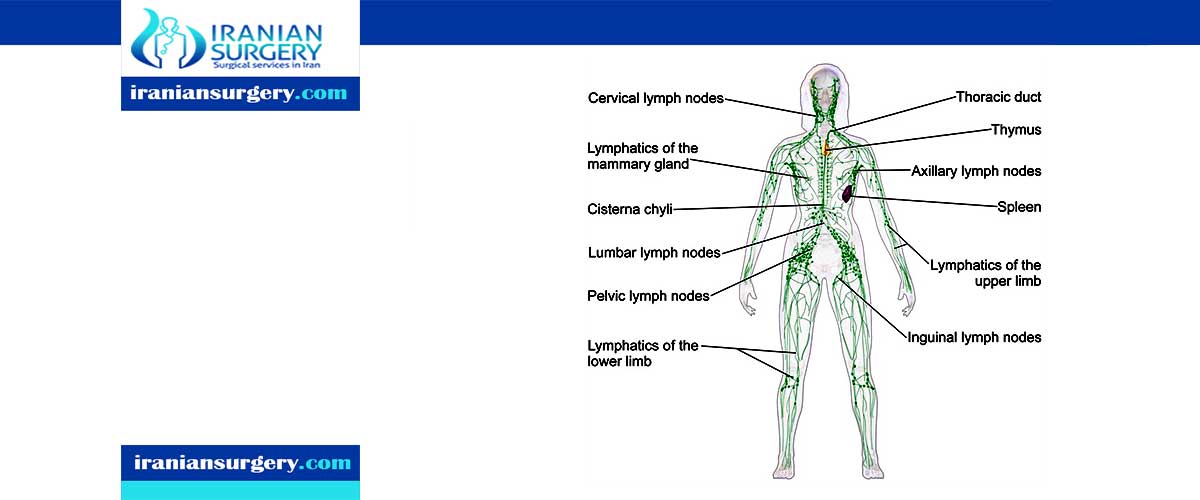
The lymphatic system is responsible for returning excess fluid from body tissues to the circulatory system and for defending against foreign or harmful agents such as bacteria, viruses, or cancerous cells. The major components of the lymphatic system are lymph capillaries, lymph vessels, and lymph nodes. Lymph is a clear fluid found in tissues that originates from the circulatory system. Lymph capillaries are tiny vessels that carry excess lymph to larger lymph vessels; these in turn empty to the circulatory system. Lymph nodes are small, oval- or bean-shaped masses found throughout the lymphatic system that act as filters against foreign materials. They tend to group in clusters in such areas as the neck (cervical lymph nodes), under the arm (axillary lymph nodes), the pelvis (iliac lymph nodes), and the groin (inguinal lymph nodes).
The lymphatic system plays an important role in the spread of cancerous cells throughout the body. Cancer cells can break away from their primary site of growth and travel through the bloodstream or lymphatic system to other sites in body. They may then begin growing at these distant sites or in the lymph nodes themselves; this process is called metastasis. Removal of the lymph nodes, then, is a way that doctors can determine if a cancer has begun to metastasize. Lymphadenectomy may also be pursued as a cancer treatment to help prevent further spread of abnormal cells.
Preparation
Lymph nodes may become swollen or enlarged as result of invasion by cancer cells. Swollen lymph nodes may be palpated (felt) during a physical exam. Before lymph nodes are removed, a small amount of tissue is usually removed. A biopsy will be performed on it to check for the presence of abnormal cells.
The patient will be asked to stop taking aspirin or aspirin-containing drugs for a period of time prior to surgery, as these can interfere with the blood's ability to clot. Such drugs may include prescription blood thinners (for example, Coumadin—generically known as warfarin and heparin). However, patients should discuss their medications with regard to their upcoming surgery with their doctors, and not make any adjustments or prescription changes on their own. No food or drink after midnight the night before surgery will be allowed.
Aftercare
Directly following surgery, the patient will be taken to the recovery room for constant monitoring and to recover from the effects of anesthesia. The patient may then be transferred to a regular room. If axillary nodes have been removed, the patient's arm will be elevated to help prevent postsurgical swelling. Likewise, the legs will be elevated if an inguinal lymphadenectomy had been performed. A drain placed during surgery to remove excess fluids from the surgical site will remain until the amount of fluid collected in the drain decreases significantly. The patient will generally remain in the hospital for one day.
Specific steps should be taken to minimize the risk of developing lymphedema, a condition in which excess fluid is not properly drained from body tissues, resulting in swelling. This swelling can sometimes become severe enough to interfere with daily activity. Common sites where lymphedema can develop are the arm or leg. Prior to being discharged, the patient will receive the following instructions for care of areas of the body that may be affected by lymph node removal:
- All cuts to the area should be properly cleaned, treated with an antibiotic ointment, and covered with a bandage.
- Heavy lifting should be avoided; bags should be carried on the unaffected arm.
- Tight jewelry and clothing with tight elastic bands should be avoided.
- Injections, blood draws, and blood pressure measurements should be done on the unaffected arm.
- Sunblock should be worn on the affected area to minimize the risk of sunburn.
- Steps should be taken to avoid cuts to the skin. For example, an electric razor should be used to shave the affected area; protective gloves should be worn when working with abrasive items.

Complications
Lymphedema may result from lymphadenectomy. Extensive resection of lymphatic tissue can lead to the formation of a lymphocele.
10 common questions about Lymphadenectomy
[kkstarratings]



