Endolymphatic hydrops
Endolymphatic hydrops Symptoms
Endolymphatic hydrops Prognosis
Endolymphatic hydrops Causes
Endolymphatic hydrops treatment
Endolymphatic hydrops
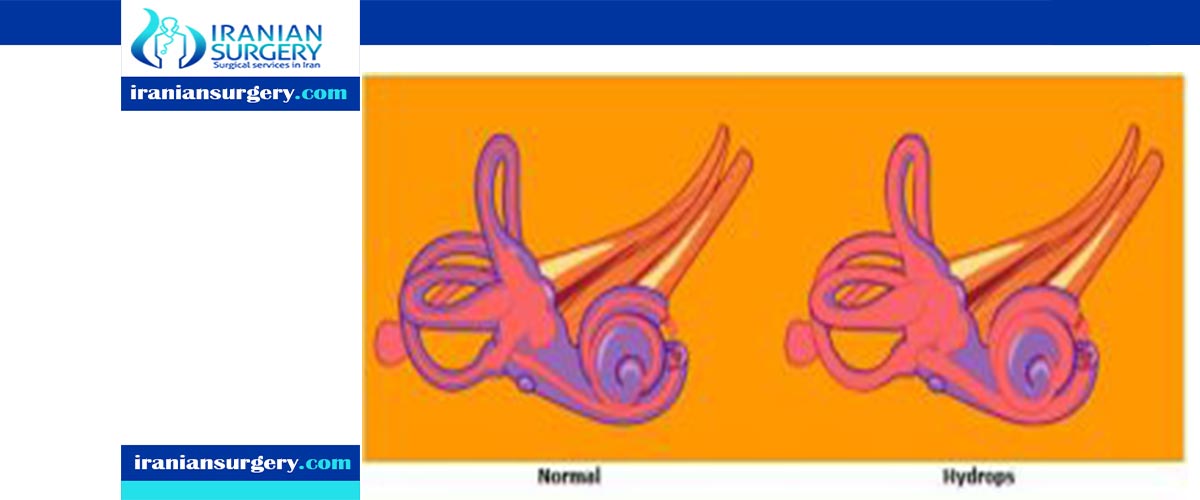
Endolymphatic hydrops is a disorder of the inner ear. It consists of an excessive build-up of the endolymph fluid, which fills the hearing and balance structures of the inner ear. Endolymph fluid, which is partly regulated by the endolymph sac, flows through the inner ear and is critical to the function of all sensory cells in the inner ear. In addition to water, endolymph fluid contains salts such as sodium, potassium, chloride and other electrolytes. If the inner ear is damaged by disease or injury, the volume and composition of the endolymph fluid can change, causing the symptoms of endolymphatic hydrops.
Endolymphatic hydrops Symptoms
The symptoms of endolymphatic hydrops include the feeling of pressure or fullness in the ears, hearing loss, tinnitus (ringing in the ears) and balance problems. Individuals who have Meniere’s disease have a degree of endolymphatic hydrops that is strong enough to trigger the symptoms of this disease, but individuals with endolymphatic hydrops do not always progress to Meniere’s disease.
Read more about: Submandibular gland surgery
Endolymphatic hydrops Prognosis
Hydrops is a chronic disease, like diabetes or hypertension. It needs to be treated medically (low sodium diet and diuretic) like other disease processes for many years. Like other disease states, it is can often be well controlled with medical therapies. This fact needs to be taken into account when surgical options are entertained. Certain individuals with hydrops will develop the disease in the opposite ear, which occurs in 5-30% of patients with hydrops. If an individual has had Meniere’s disease in one ear for three or more years, without symptoms in the other ear, the likelihood of getting dizziness in the other ear is quite rare.

Read more about: Cochlear implant sound
Endolymphatic hydrops Causes
Endolymphatic hydrops may occur as a result of trauma such as a blow to the head, infection, degeneration of the inner ear, allergies, dehydration and loss of electrolytes or in extremely rare circumstances a benign tumor such as an endolymphatic sac tumor. In many cases, it is not clear what causes the disorder. Meniere’s attacks occur when there is an increase in endolymphatic volume in the inner ear, causing a temporary leak in the membrane separating the perilymph (potassium poor fluid) and the endolymph (potassium rich fluid). The mix of these two fluids surrounding the vestibular sensory cells can lead to a temporary electrical blockade and loss of sensory function. The sudden change in the rate of the vestibular nerve firing results in a disturbance of signal processing in the corresponding brain regions, and thus to acute sensations of imbalance, otherwise known as vertigo.
Read more about: cochlear implant
Endolymphatic hydrops treatment
Ménière’s disease is characterized by sudden, violent attacks or episodes of vertigo, tinnitus, hearing loss, and aural fullness. The attacks typically occur at intervals of weeks to months, with symptom-free periods between attacks. Over several years, there is partial destruction of hearing and sometimes of balance function. Ménière’s disease affects both ears in up to half of those who experience it. Treatment is intended to improve symptoms, manage acute attacks, deal with the damage to hearing and balance, and maintain quality of life.
The treatment of secondary endolymphatic hydrops (SEH) is somewhat different. Since SEH is secondary to (that is, results from) an underlying disorder, the symptoms tend to be present more continuously, rather than occurring in spontaneous attacks. However, they are often less violent, and SEH may cause less damage to hearing and balance than does Ménière’s disease.
Treatment of SEH has five goals: to stabilize the body’s fluid and electrolyte levels; to identify and treat the underlying condition that is driving the SEH; to improve daily symptoms; to manage persistent symptoms and changes; and to maintain quality of life.
- Goal 1: stabilizing the body’s fluid and electrolyte levels
Stabilizing the fluid and electrolyte levels may help reduce or relieve the symptoms. Modifications in diet may be necessary in order to achieve such stabilization.
A hydrops diet regimen (HDR) often makes many people with SEH feel significantly better without any other treatment. The HDR is the cornerstone of stabilizing overall fluid levels. The most important aspect of this regimen is consistency. Eating a balanced diet in moderate amounts at regular intervals—with meals and snacks of a consistent size, eaten at about the same time every day, without skipping meals or alternating tiny snacks with huge meals—helps the body’s fluid and electrolyte levels remain stable.
A second key element of the HDR is minimizing the use of solutes (salts and sugars) in the diet. Solutes require the body to use large amounts of fluid for dilution and digestion. This causes large fluctuations in body fluids and consequently in the endolymph, which can trigger hydrops symptoms. An important starting point of this diet is to avoid adding salt or sugar to food and to avoid eating prepared foods (those that come out of a can or other container).
Adequate fluid intake is another mainstay of the HDR. In order to function at its best, the body needs lots of water—six to eight glasses spaced evenly throughout the day. It is also important to anticipate and replace the additional fluid lost through perspiration during exercise, fever, or hot weather. Other fluids—for example, low-sugar sodas, herbal teas, and low-sugar fruit and vegetable juices—may also make up part of the daily allotment. Caffeine (found in coffee, tea, some herbal teas, colas, chocolate, and some medications) and alcohol have strong diuretic properties and may need to be restricted, because they can cause the body to lose more fluid than it has taken in.
Physicians may prescribe diuretics as part of treatment, not to cause fluid loss, but rather to “push” the kidneys to excrete a constant amount of urine throughout the day, thus helping to minimize large swings in the body’s fluid content. With diuretic use, drinking lots of water is important to avoid dehydration. Certain diuretics require the use of a potassium supplement to replace potassium lost through the urine. It is important to discuss proper use of medication and intake of food and water with the prescribing physician.
Read more about: cochlear implant surgery
- Goal 2: identifying and treating the underlying condition
This goal is complex and will likely involve both the otologist (ear specialist) and the primary care provider (internist, family practice physician, nurse practitioner, etc.). Once an underlying condition is identified and treated, SEH symptoms tend to improve over time with proper management. Hydrops associated with head trauma or ear surgery usually improves over the course of one to two years following the causative event.
- Goal 3: improving daily symptoms
With the use of the HDR and possibly also a diuretic, balance symptoms may improve dramatically. Other medications may be used to help with persistent dizziness, nausea, or vomiting.
Other strategies to reduce the symptoms of SEH include:
- Maintaining normal weight, or losing any excess weight. When a person is overweight, the vestibular system must struggle to deal with a larger-than-normal and displaced center of gravity.
- Avoiding aspirin in high doses, which can cause temporary tinnitus.
- Avoiding ibuprofen and other NSAIDS (nonsteroidal anti-inflammatory drugs), which can have a direct effect on fluid balance and may increase symptoms in some SEH patients.
- Stopping smoking. Smoking constricts the single, tiny artery that feeds the ear, thus depriving it of oxygen and nutrients.
- Maintaining general health by getting adequate exercise and sleep, both can help with cardiovascular health to support the inner ear. Exercise can help the musculature needed for balance stay active.
Vestibular rehabilitation, a type of specialized physical therapy for vestibular patients, can improve tolerance for activity, overall energy level, and symptoms of dizziness and imbalance. The cognitive symptoms that often accompany vestibular disorders—for instance, trouble with concentration, short-term memory, reading, or prioritizing tasks—may diminish as the hydrops is brought under control, but occupational and speech therapists can help if any symptoms remain.
- goal 4: managing persistent symptoms and changes
If dizziness and vertigo become intractable, more aggressive measures may be considered. Medications or surgery can be used to selectively destroy the problematic inner ear structures.
There are various surgeries that may be recommended. Endolymphatic decompression procedures aim at relieving fluid pressure in the inner ear. Another type of surgery is a labyrinthectomy, which destroys the membranous structures of the inner ear that detect gravity and motion changes. Semi-circular canal plugging and neurectomy (cutting the vestibular nerve between the ear and the brain) create mechanical changes that prevent abnormal inner ear signals from reaching the brain, thus reducing symptoms. These procedures do not cure the underlying disorder and are not without risk, but they may improve symptoms in some cases.
SEH does not usually result in significant hearing loss. If it does occur, modern hearing aids and other assistive devices may be useful. In addition, tinnitus-masking devices can be used to help deal with annoying tinnitus.
Very often, people with inner ear disorders attempt to avoid aggravating their symptoms by restricting their activity and becoming reclusive. This is counterproductive. In fact, remaining as active and busy as possible (within safe limits) helps the brain adjust to changes in inner ear function and helps control symptoms. The physician may recommend a course of vestibular rehabilitation therapy to help the brain compensate for changes in balance function.
- Goal 5: maintaining quality of life
As with any chronic disorder, maintaining a healthy outlook and as normal a routine as possible is essential. Creating a safe physical environment in the home is also important, as well as taking into consideration whether one should undertake potentially hazardous activities such as driving a car, climbing ladders, or participating in sports.
As an “invisible” disability, an inner ear disorder can be frustrating to manage. A person may feel miserable, yet “look normal” to friends and family. Educating others about the illness can help them better understand the difficulties and consequences of having a vestibular disorder. Counseling or participating in a support group for people with inner ear disorders may help to deal with the confusion or secondary depression that often accompanies these conditions. In any case, the physician and the physician’s staff remain the patient’s primary resource in understanding and dealing with SEH.
Read more about: eardrum repair surgery in Iran

