Low Testosterone (Male Hypogonadism)
Low Testosterone (Male Hypogonadism)
What is Low Testosterone (Male Hypogonadism)?
Low testosterone (male hypogonadism) is a condition in which the testes (testicles, the male reproductive glands) do not produce enough testosterone (a male sex hormone).
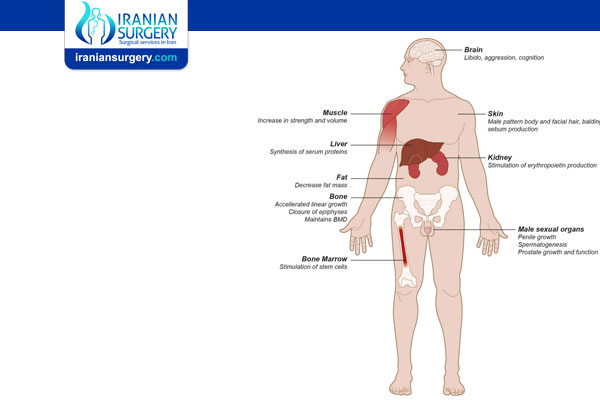
In men, testosterone helps maintain and develop:
. Sexual features
. Muscle mass
. Adequate levels of red blood cells
. Bone density
. Sense of well-being
. Sexual and reproductive function
Low Testosterone Treatment
How common is low testosterone?
Low testosterone affects almost 40% of men aged 45 and older. It is difficult to define normal testosterone levels, because levels vary throughout the day and are affected by body mass index (BMI), nutrition, alcohol consumption, certain medications, age and illness.
What causes low testosterone?
As a man ages, the amount of testosterone in his body gradually drops. This natural decline starts after age 30 and continues (about 1% per year) throughout his life.
There are many other potential causes of low testosterone, including the following:
. Injury (trauma, interrupted blood supply to the testes) or infection of the testes (orchitis)
. Chemotherapy for cancer
. Metabolic disorders such as hemochromatosis (too much iron in the body)
. Dysfunction or tumors of the pituitary gland
. Medications, including opioids, hormones used to treat prostate cancer, and steroids (such as prednisone)
. Acute (short-term) or chronic (long-term) illness
. Alcohol abuse
. Cirrhosis of the liver
. Chronic renal (kidney) failure
. HIV/AIDS
. Inflammatory conditions such as sarcoidosis (a condition that causes inflammation of the lungs and other organs)
. Kallman syndrome (abnormal development of the hypothalamus, a gland in the brain that controls many hormones)
. Klinefelter syndrome (a genetic condition in which a male is born with an extra copy of the X chromosome). Also called XXY syndrome
. High levels of the milk-producing hormone prolactin
. Obesity or extreme weight loss
. Uncontrolled type 2 diabetes mellitus
. Congenital defect (present at birth)
. Obstructive sleep apnea
. Aging
. Estrogen excess (usually from an external or environmental source)
. Previous anabolic steroid abuse
. Severe primary hypothyroidism
. Pubertal delay
. Trauma (head injury)
. Radiation exposure or prior surgery of the brain
What are the symptoms of low testosterone?
Symptoms of low testosterone depend on the age of person, and include the following:
. Low sex drive
. Erectile dysfunction
. Decreased sense of well-being
. Depressed mood
. Difficulties with concentration and memory
. Fatigue
. Moodiness and irritability
. Loss of muscular strength
Other changes that occur with low testosterone include:
. A decrease in hemoglobin and mild anemia
. A decrease in body hair
. Thinning of the bones (osteoporosis)
. Increased body fat
. Breast development (gynecomastia)
. Infertility
Diagnosis and Tests
How is low testosterone diagnosed?
Low testosterone is diagnosed by measuring the amount of testosterone in the blood with a blood test. It may take several measurements to determine if a patient has low testosterone, since levels tend to change throughout the day. The highest levels of testosterone are generally in the morning, near 8 a.m. This is why doctors prefer to measure testosterone levels in the early morning.
Prevention
Can low testosterone be prevented?
There are no known ways to prevent low testosterone that is caused by genetic conditions or damage to the testes or pituitary gland.
A healthy lifestyle that includes good nutrition, exercise, weight management, and that avoids excessive use of alcohol and drugs can help keep testosterone levels normal.
What are the benefits of testosterone replacement therapy?
Potential benefits of testosterone replacement therapy may include:
. In boys, avoiding problems related to delayed puberty
. Loss of fat
. Increased bone density and protection against osteoporosis
. Improved mood and sense of well-being
. Improved sexual function
. Improved mental sharpness
. Greater muscle strength and physical performance
What are the side effects of testosterone replacement therapy?
The side effects of testosterone replacement therapy include:
. Acne or oily skin
. Swelling in the ankles caused by mild fluid retention
. Stimulation of the prostate, which can cause urination symptoms such as difficulty urinating
. Breast enlargement or tenderness
. Worsening of sleep apnea (a sleep disorder that results in frequent nighttime awakenings and daytime sleepiness)
. Smaller testicles
. Skin irritation (in patients receiving topical testosterone replacement)
Laboratory abnormalities that can occur with testosterone replacement include:
. Increase in prostate-specific antigen (PSA)
. Increase in red blood cell count
. Decrease in sperm count, producing infertility (inability to have children), which is especially important in younger men who desire fertility
If you are taking hormone replacement therapy, regular follow-up appointments with your physician are important.
Guidelines suggest discussing the potential risk vs. benefit of evaluating prostate cancer risk and prostate monitoring. The doctor and patient will decide together regarding prostate cancer monitoring. For patients who choose monitoring, clinicians should assess prostate cancer risk before starting testosterone treatment, and 3 to 12 months after starting testosterone:
. PSA levels should be checked at 3, 6, and 12 months within the first year, and then every year after that.
. A digital rectal examination of the prostate should be done at 3-6 months and 1 year after beginning therapy, and then every year after that. This is recommended even for men who are not on testosterone replacement therapy, as an age-related prostate cancer screening. This usually begins at age 50.
. Hematocrit levels will be checked before testosterone therapy starts, and then on a regular basis to make sure red blood cell levels remain normal.
Who shouldn't take testosterone replacement therapy?
Testosterone replacement therapy may cause the prostate to grow. If a man has early prostate cancer, there is concern that testosterone may stimulate the cancer's growth. Therefore, men who have prostate cancer should not take testosterone replacement therapy. It is important for all men considering testosterone replacement therapy to undergo prostate screening before starting this therapy.
Other men who should not take testosterone replacement therapy include those who have:
. An enlarged prostate resulting in urinary symptoms (difficulty starting a urinary stream)
. A lump on their prostate that has not been evaluated
. A PSA measurement above 4
. Breast cancer
. An elevated hematocrit level (higher-than-normal number of red blood cells)
. Severe congestive heart failure
. Obstructive sleep apnea that has not been treated
During Testosterone Treatment
Management and Treatment
How is low testosterone treated?
Low testosterone is treated with testosterone replacement therapy, which can be given in several different ways:
. Intramuscular injections (into a muscle), usually every 10 to 14 days;
. Testosterone patches, which are used every day and are applied to different parts of the body, including the buttocks, arms, back, and abdomen
. Testosterone gels that are applied every day to the clean dry skin of the upper back and arms (the gels require care in making sure that the hormone is not accidentally transferred to another person or partner)
. Pellets that are implanted under the skin every two months.
Source:
. https://my.clevelandclinic.org/health/diseases/15603-low-testosterone-male-hypogonadism