Bicornuate Uterus
Bicornuate Uterus
What is a Bicornuate Uterus?
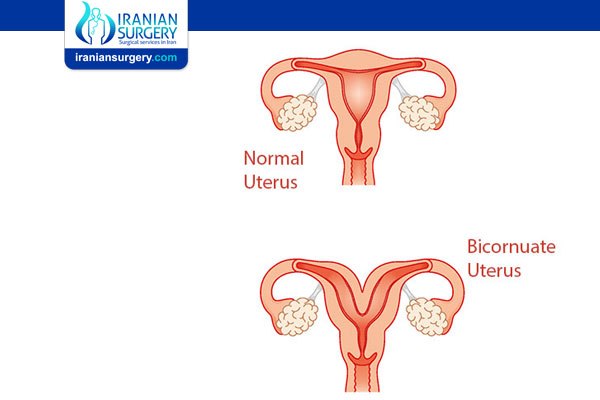
If you have a bicornuate uterus it means your uterus appears heart-shaped instead of round. A typical uterus is shaped like an upside-down pear. The wide, round part of the pear most resembles the top portion of the uterus (called the fundus). If your uterus is bicornuate, the top of your uterus dips inward at the middle, making it look like a heart. It’s commonly referred to as a heart-shaped uterus.
The uterus is one hollow cavity and is made to expand to accommodate a growing baby during pregnancy. If you have a bicornuate uterus, the top of your uterus is separated by a piece of tissue. Depending on the degree of separation, this can cause problems during pregnancy because your uterus may not be able to fully expand.
A bicornuate uterus is a congenital condition, which means it formed this way before you were born. A bicornuate uterus is usually not a cause for concern. For people who become pregnant with a bicornuate uterus, there is an increased risk of miscarriage and preterm labor. Most people won’t be aware they have a bicornuate uterus because they usually don’t have symptoms. Some people do experience painful periods or repeat miscarriages.
Before Bicornuate Uterus Treatment
What are the symptoms of a bicornuate uterus?
If you have symptoms of a bicornuate uterus, you might experience:
. Frequent miscarriages (usually more than three).
. Vaginal bleeding.
. Painful menstruation.
. Painful intercourse (dyspareunia).
. Pelvic pain.
In some cases, you may not realize you have a heart-shaped uterus because you don’t have symptoms. Since you’re born with a bicornuate uterus, the symptoms may feel normal to you. Oftentimes, a person isn’t aware they have a heart-shaped uterus until they’re pregnant or have had several miscarriages.
What causes a bicornuate uterus?
A bicornuate uterus is congenital, meaning you were born with it. Your uterus forms while you’re still in the womb — sometime between 10 and 20 weeks of pregnancy.
During development, two ducts (called the Mullerian ducts) normally fuse together to form one uterine cavity. In the case of a bicornuate uterus, two uterine cavities exist because the ducts did not merge together completely. A bicornuate uterus can have a deep heart shape or it can be minor and never cause a problem.
A heart-shaped uterus is not hereditary — meaning you won’t pass it on to your children.
How common is a bicornuate uterus?
A bicornuate uterus is one of the more common abnormalities of the uterus, but it’s still considered rare. Less than .5% of people assigned female at birth (AFAM) have a bicornuate uterus. Most people won’t be aware they have an irregularly shaped uterus until they’re pregnant and experience several miscarriages.
Is having a bicornuate uterus bad?
No. Having a bicornuate uterus isn’t bad or dangerous. In most cases, you won’t know you have a heart-shaped uterus because you won't have noticeable symptoms. Having an irregular-shaped uterus can contribute to complications during pregnancy. If you have a bicornuate uterus, speak with your healthcare provider to understand the condition and how it affects your life.
Diagnosis and Tests
How is a bicornuate uterus diagnosed?
Most people aren’t aware they have a bicornuate uterus until they experience repeated pregnancy loss. Checking the shape of the uterus after repeat miscarriage will reveal the irregularity. In other cases, a heart-shaped uterus is found during a routine ultrasound during pregnancy or because of painful periods.
After an initial pelvic exam, your healthcare provider will use several imaging techniques to confirm a bicornuate uterus. This is done to measure the depth of separation and distinguish a bicornuate uterus from other uterine abnormalities.
. Ultrasound: An ultrasound is usually the first diagnostic test used to detect a heart-shaped uterus. After it’s detected, your healthcare provider may use more advanced diagnostics to get a better view of the shape of your uterus. 3D ultrasound can also be very helpful.
. MRI (magnetic resonance imaging): This produces the most detailed images of the uterus because it can show multiple dimensions and angles.
What are the different types of bicornuate uterus?
Your healthcare provider may describe your bicornuate uterus as either partial (or incomplete) or complete. These terms refer to how far your uterus dips down at the top of the uterus towards the cervix.
. Partial bicornuate uterus: A partial bicornuate uterus describes a lesser degree of separation between the two cavities. Your uterus is still heart-shaped, but the indentation that divides your uterus is not as severe.
. Complete bicornuate uterus: A complete bicornuate uterus is when the indentation at the top of your uterus is severe, making the separation of the uterine cavity more distinct.
What are the complications of treating a bicornuate uterus?
The risks associated with the surgery to correct a bicornuate uterus are:
. Bleeding (hemorrhage).
. Infection.
. Uterine adhesions/scarring.
If treatment for a bicornuate uterus is recommended, your healthcare provider will explain the procedure, its risks and your chances of having a successful pregnancy.
Prevention
How can I prevent a bicornuate uterus?
There is nothing you can do to prevent a heart-shaped uterus. It’s a condition that is present at birth and was not caused by anything your parents did or didn’t do.
During Bicornuate Uterus Treatment
Management and Treatment
How do you fix a bicornuate uterus?
In most cases, this condition does not need to be surgically treated.
A bicornuate uterus may be surgically treated through a surgery called metroplasty. But, this procedure is controversial and only performed in specific circumstances. The shape of the uterus will be corrected to the preferred upside-down pear shape. This surgery can be done laparoscopically, a minimally invasive surgery that does not require a large incision. The surgery involves removing the tissue that is causing the indentation or heart-shape appearance.
People should wait at least three months to try to conceive after having a mitoplast. This is due to the increased risk for uterine rupture during labor.
After Bicornuate Uterus Treatment
Outlook / Prognosis
Can I still have a baby if I have a bicornuate uterus?
Yes, you’re still able to have a baby if you have a bicornuate uterus. However, you’re more at risk for pregnancy complications. This is mostly due to your uterus not being able to expand to accommodate your baby. Your healthcare provider will discuss any precautions you should take during pregnancy and how a heart-shaped uterus can affect your pregnancy and delivery.
How will a bicornuate uterus affect my pregnancy?
Your ability to conceive is not usually affected by a bicornuate uterus. However, the shape of your uterus does put you at a slightly higher risk for certain pregnancy complications like:
. Miscarriage.
. Preterm birth and early labor.
. Low birth weight (caused by not having enough room to grow in the womb).
. Vaginal bleeding.
. Your baby is breech, transverse or in another position in the uterus other than head-down.
. Increased chance for cesarean delivery.
. Postpartum hemorrhage.
. Placenta previa or other condition of the placenta.
. Pregnancy-induced high blood pressure.
. Incompetent cervix.
Management for a pregnancy in a bicornuate uterus is increased monitoring. You will likely have more prenatal ultrasounds so your healthcare provider can observe the size and shape of your uterus and the position of your baby and the placenta. The unusual shape of your uterus increases your chance of having a c-section because your baby is more likely to be breech.
People with a bicornuate uterus can have a healthy pregnancy and normal delivery. The precautions are taken to ensure you and your baby stay safe through pregnancy and birth.
Are my labor and delivery affected by a bicornuate uterus?
Your delivery could be impacted by a heart-shaped uterus. Since your uterus is irregularly shaped, it might not expand enough to accommodate a full-term baby. This means your baby could be in an awkward position or be crammed very tightly inside your womb. Having a bicornuate uterus increases the likelihood of your baby being breech. For this reason, healthcare providers often recommend a c-section.
Will my baby have a birth defect if I have a bicornuate uterus?
No, your baby isn’t going to have a birth defect just because you have a bicornuate uterus. You’re at increased risk for preterm labor (labor occurring before 37 weeks of pregnancy). This means your baby can be born premature or before certain organs or systems have fully developed.
Are there health risks associated with a bicornuate uterus?
People who aren’t pregnant, or don’t wish to become pregnant, don’t have as many health risks to be concerned about. If you have a bicornuate uterus, you have a higher risk for endometriosis and repeat miscarriages.
If you are pregnant, the highest risks associated with a bicornuate uterus are:
. Miscarriages.
. Preterm delivery.
. Low birth weight babies.
. Babies in a breech or transverse position in the uterus.
When should I see my healthcare provider?
Contact your healthcare provider if you have irregular vaginal bleeding or experience pelvic pain during menstruation or sex. These are signs of a bicornuate uterus.
If you are pregnant and have been diagnosed with a bicornuate uterus, you should also contact your healthcare provider immediately if there are any signs of premature labor, like uterine cramping or rupturing of your membranes.
Can you have twins if you have a bicornuate uterus?
It’s rare but possible, to have a twin pregnancy with a bicornuate uterus. Both conditions (twin pregnancy and bicornuate uterus) are associated with a number of risks such as preterm birth, low birth weight, miscarriage and malpresentation. Malpresentation is when your baby is not in a head-down position in the uterus before delivery.
Source:
. https://my.clevelandclinic.org/health/diseases/22798-bicornuate-uterus